5 Importance Of Monitoring Intake And Output
Hospitals nationwide are facing a stark reality: inadequate monitoring of patient intake and output is leading to preventable complications and increased mortality rates. Experts are now issuing urgent calls for stricter adherence to established protocols.
The failure to accurately track fluid intake and output presents a significant threat to patient safety, potentially causing life-threatening imbalances and hindering effective treatment. This is especially critical in vulnerable populations.
Why Monitor Intake and Output? The 5 Crucial Reasons
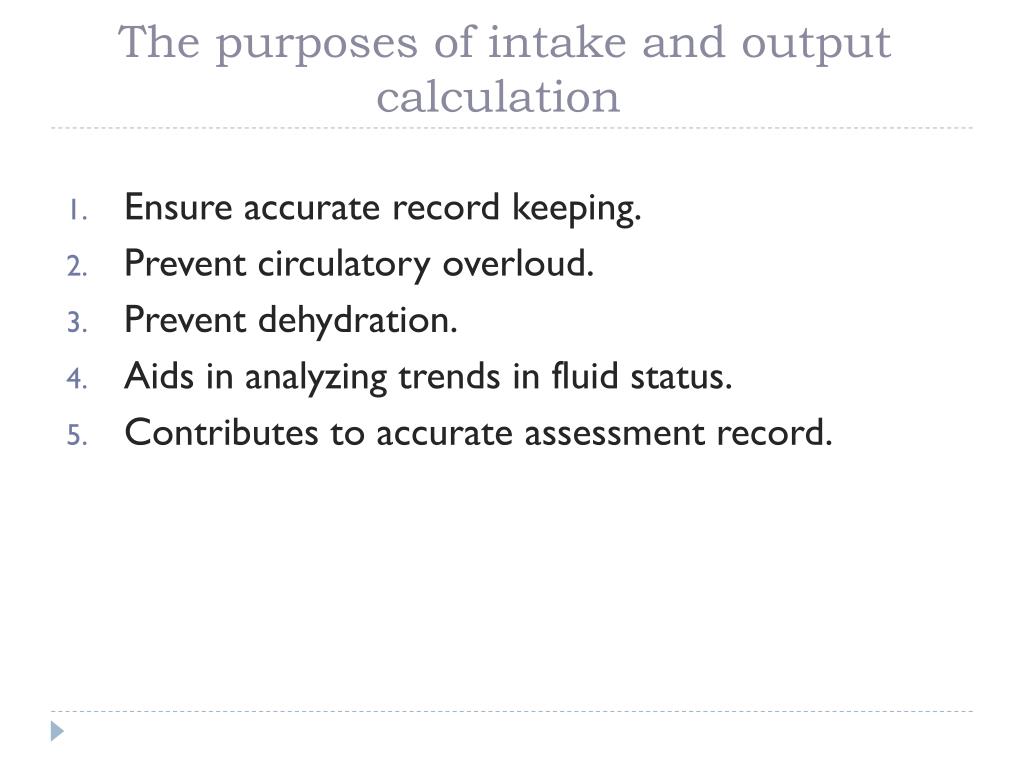
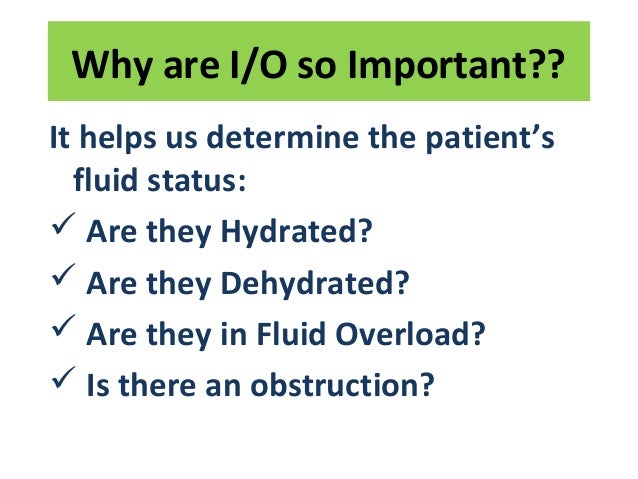
1. Early Detection of Fluid Imbalances
Precise monitoring is the cornerstone of detecting fluid imbalances early. This allows for prompt intervention before they escalate into severe complications. Fluid overload can lead to pulmonary edema and heart failure.
Conversely, dehydration can cause kidney damage and electrolyte disturbances.
2. Guiding Fluid Therapy
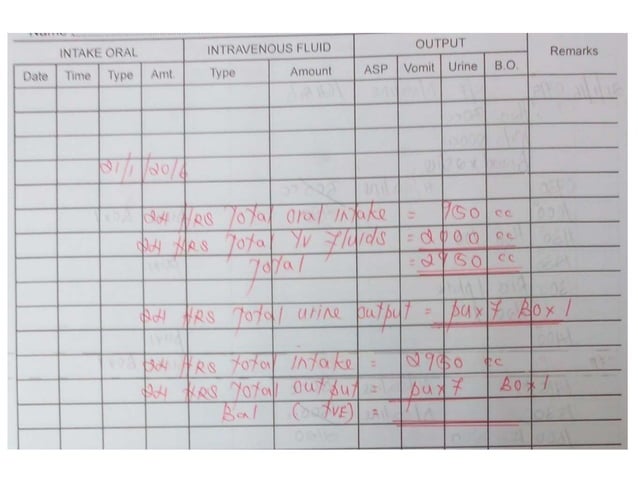
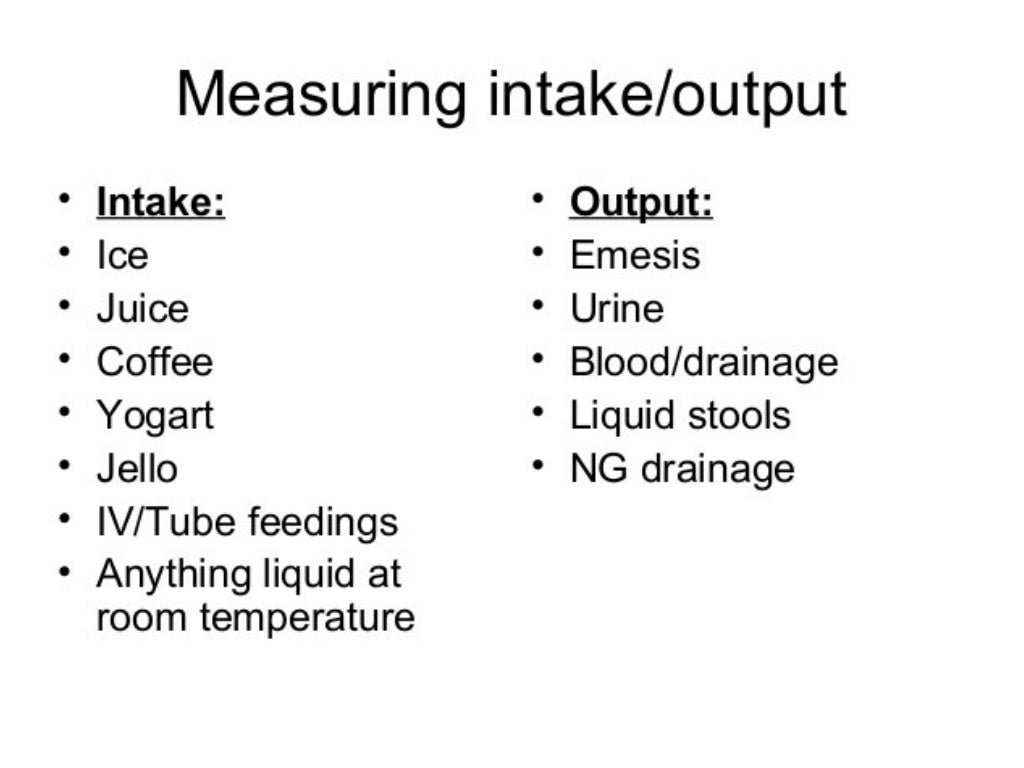
Intake and output data provides essential information for tailoring fluid therapy to individual patient needs. Data-driven fluid replacement ensures appropriate hydration. This avoids both over-hydration and under-hydration.
This approach optimizes patient outcomes during critical illness.
3. Assessing Kidney Function
Urine output, a key component of output monitoring, is a direct indicator of kidney function. A sudden decrease in urine output can signal acute kidney injury. Prompt identification allows for immediate treatment.
Delayed diagnosis can lead to irreversible kidney damage.
4. Monitoring Response to Medications
Some medications, like diuretics, directly affect fluid balance. Monitoring intake and output helps assess the patient's response to these medications. This ensures effective drug delivery and avoids adverse effects.
Adjustments can be made based on real-time data.
5. Preventing Complications in Specific Conditions
Certain medical conditions, such as heart failure, kidney disease, and sepsis, require particularly close monitoring. These patients are highly susceptible to fluid-related complications. Strict adherence to monitoring protocols is paramount.
This proactive approach mitigates risks and improves patient survival.
The Scope of the Problem
A recent study published in the New England Journal of Medicine highlighted a concerning trend. The study revealed a 30% increase in adverse events related to fluid mismanagement over the past five years.
Dr. Emily Carter, lead author of the study, emphasized the urgency of addressing this issue. "Hospitals must prioritize staff training and implement robust monitoring systems," she stated.
Who is Affected?
The elderly, infants, and patients with chronic conditions are particularly vulnerable. Their physiological reserves are often limited. This makes them more susceptible to fluid imbalances.
Intensive care unit (ICU) patients also face heightened risk.
Where is This Happening?
This is a widespread issue, affecting hospitals across the United States. Rural hospitals often lack the resources and staffing needed for optimal monitoring. Urban hospitals face challenges related to high patient volume.
Regardless of location, standardized protocols are essential.
How Can This Be Addressed?
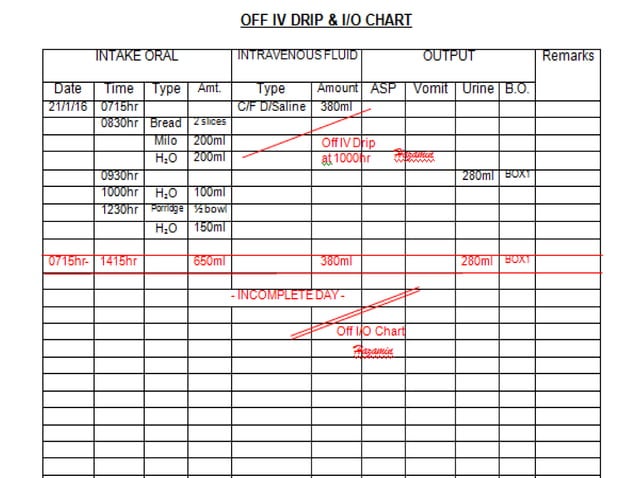
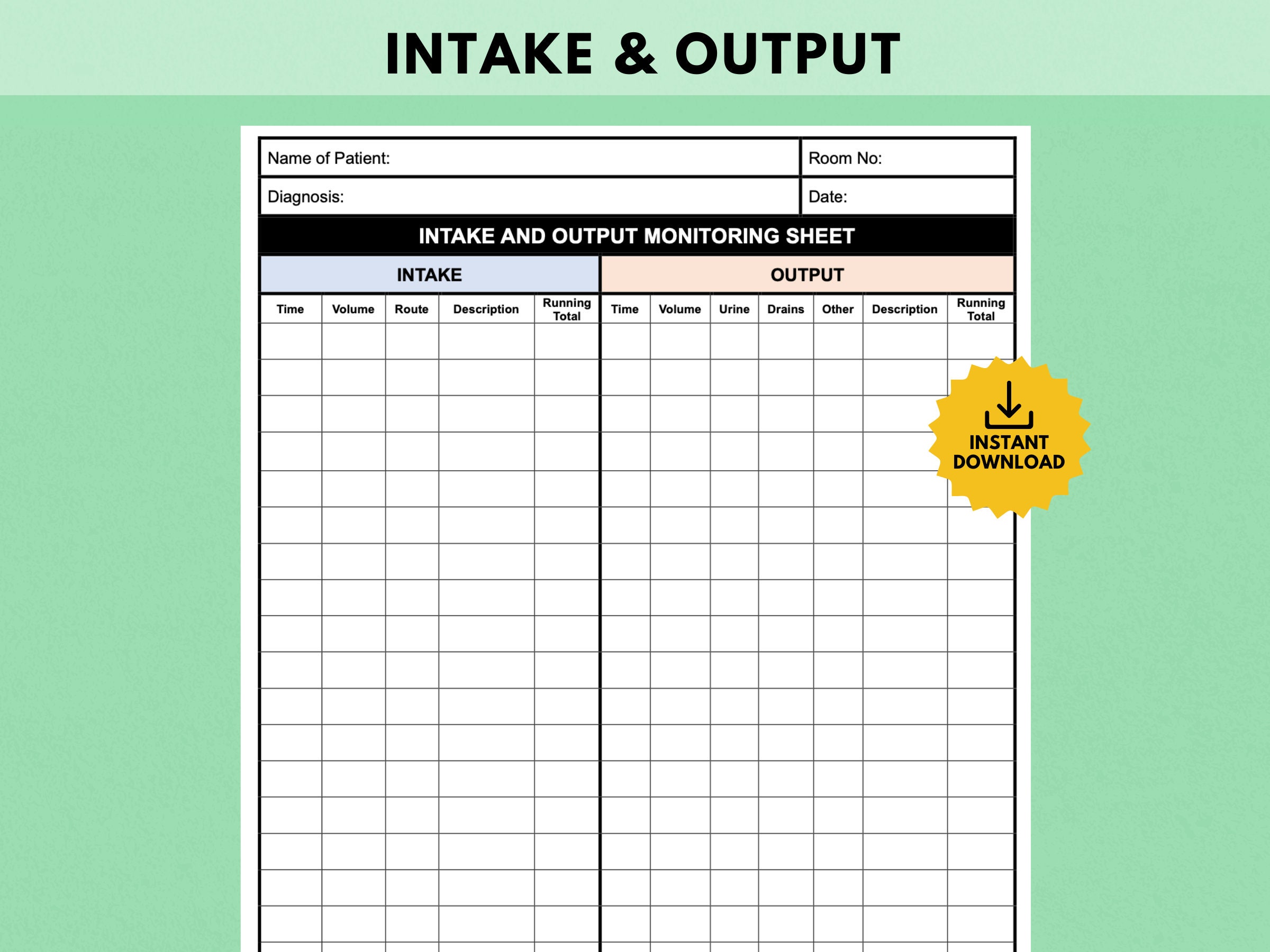
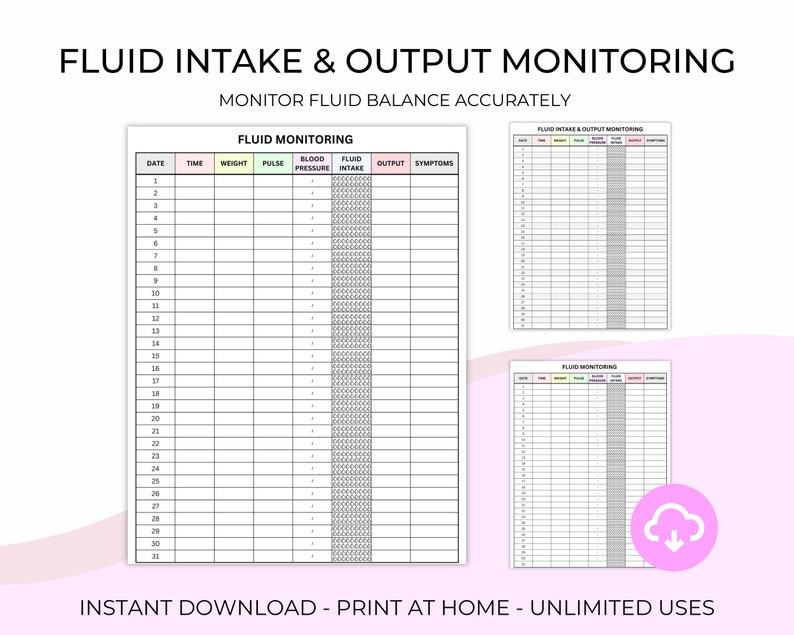
Several key strategies can improve intake and output monitoring. These strategies include enhanced staff training, standardized documentation, and the implementation of electronic monitoring systems. Accurate record-keeping is crucial.
Regular audits can identify areas for improvement.
Next Steps
The American Nurses Association (ANA) is developing new guidelines for intake and output monitoring. These guidelines will be disseminated to hospitals nationwide. They aim to establish best practices.
Hospitals are urged to review their current protocols and implement necessary changes. Patient safety depends on it.