All Of These Are Quality Improvement Strategies Except

The healthcare industry is constantly evolving, driven by the relentless pursuit of improved patient outcomes, increased efficiency, and reduced costs. Quality improvement (QI) strategies form the backbone of this evolution, with hospitals and clinics across the nation implementing various methodologies to enhance their services. However, not every initiative marketed as a QI strategy delivers tangible results.
This article explores the landscape of QI strategies, highlighting common approaches and dissecting a scenario to identify a practice that, despite potential merit, doesn't fall under the traditional definition of a QI initiative. Understanding the nuances of effective QI is critical for healthcare professionals seeking to genuinely elevate their organization's performance.
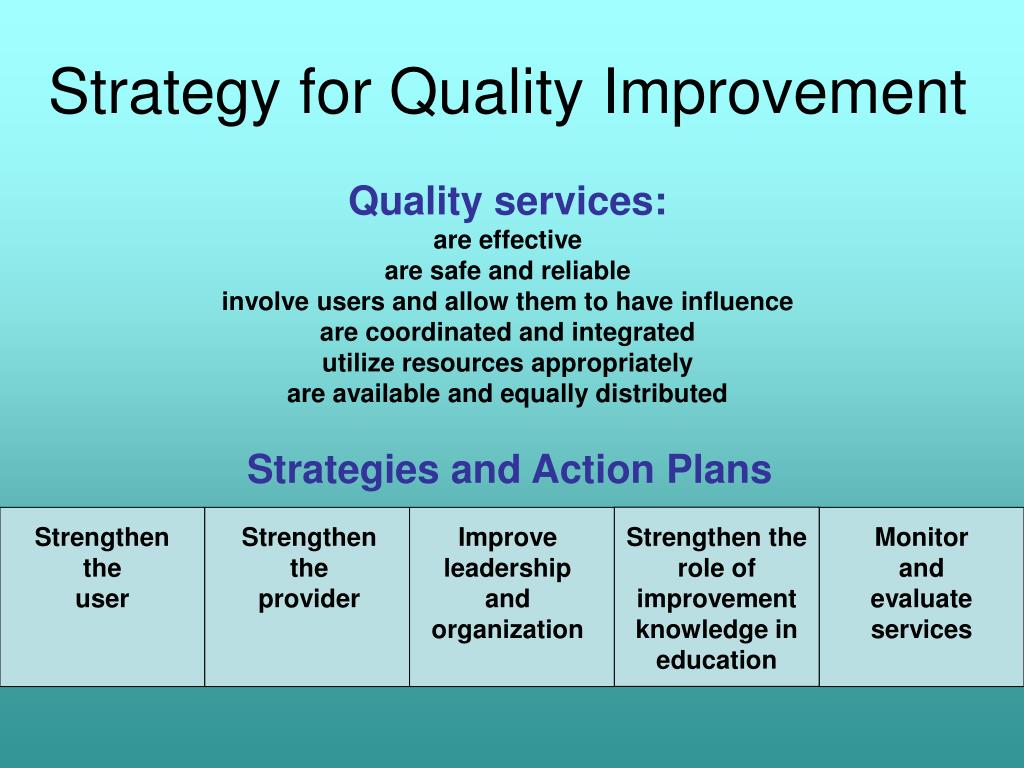
Defining Quality Improvement Strategies
At its core, quality improvement involves systematic and continuous efforts to enhance healthcare delivery. These efforts are data-driven, patient-centered, and often involve multidisciplinary teams working towards specific, measurable goals.
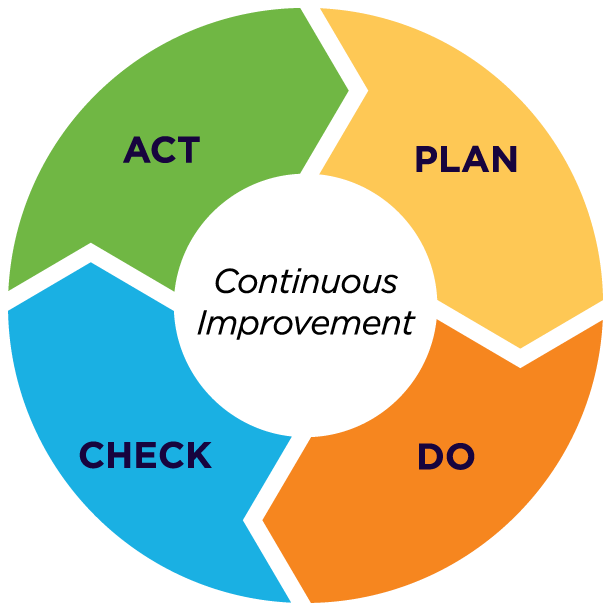
Successful QI initiatives rely on structured methodologies like Plan-Do-Study-Act (PDSA) cycles, Lean principles, and Six Sigma. These frameworks provide a roadmap for identifying problems, implementing solutions, evaluating their impact, and refining the approach as needed.
PDSA cycles, for example, enable iterative testing of changes on a small scale before widespread implementation. Lean focuses on eliminating waste and streamlining processes to improve efficiency. Six Sigma employs statistical tools to reduce variation and defects in healthcare processes.
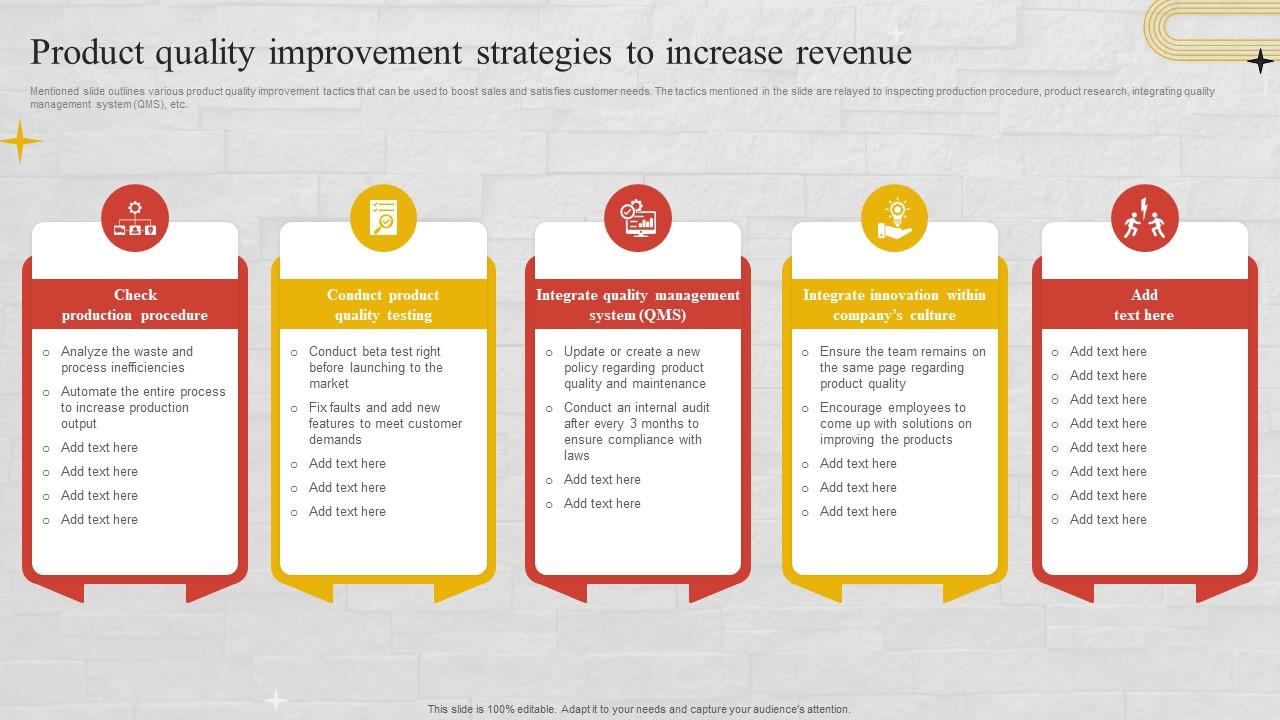
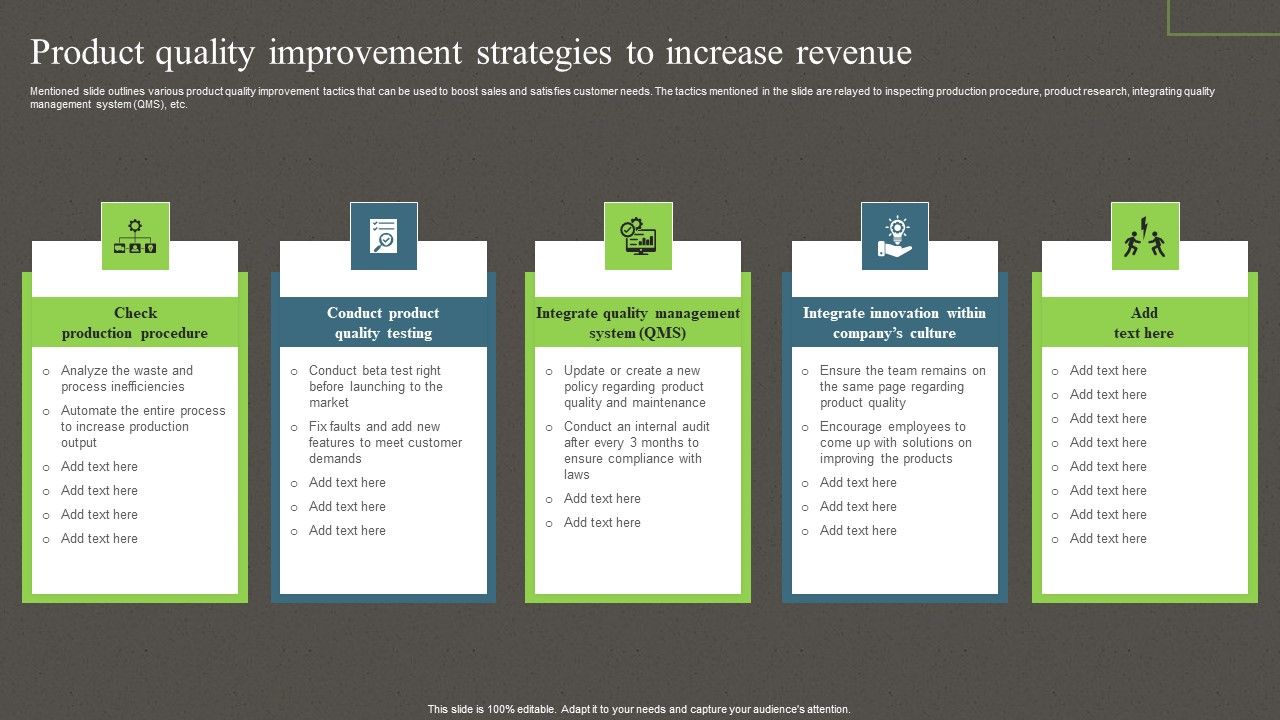
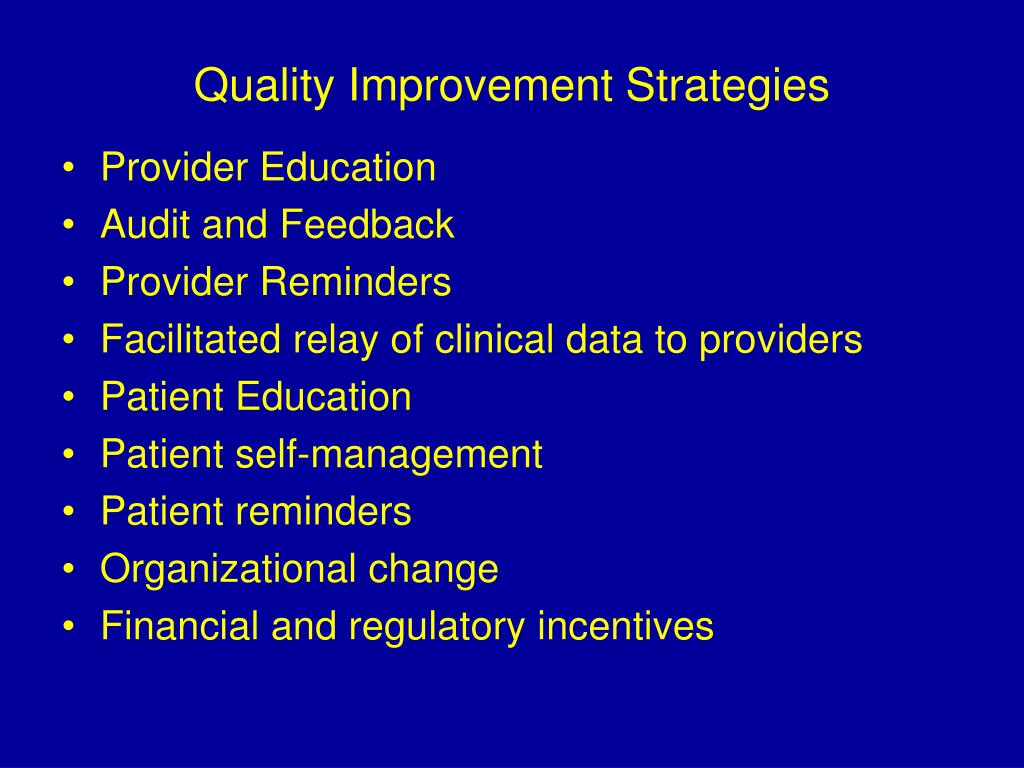
Commonly Used Quality Improvement Methodologies
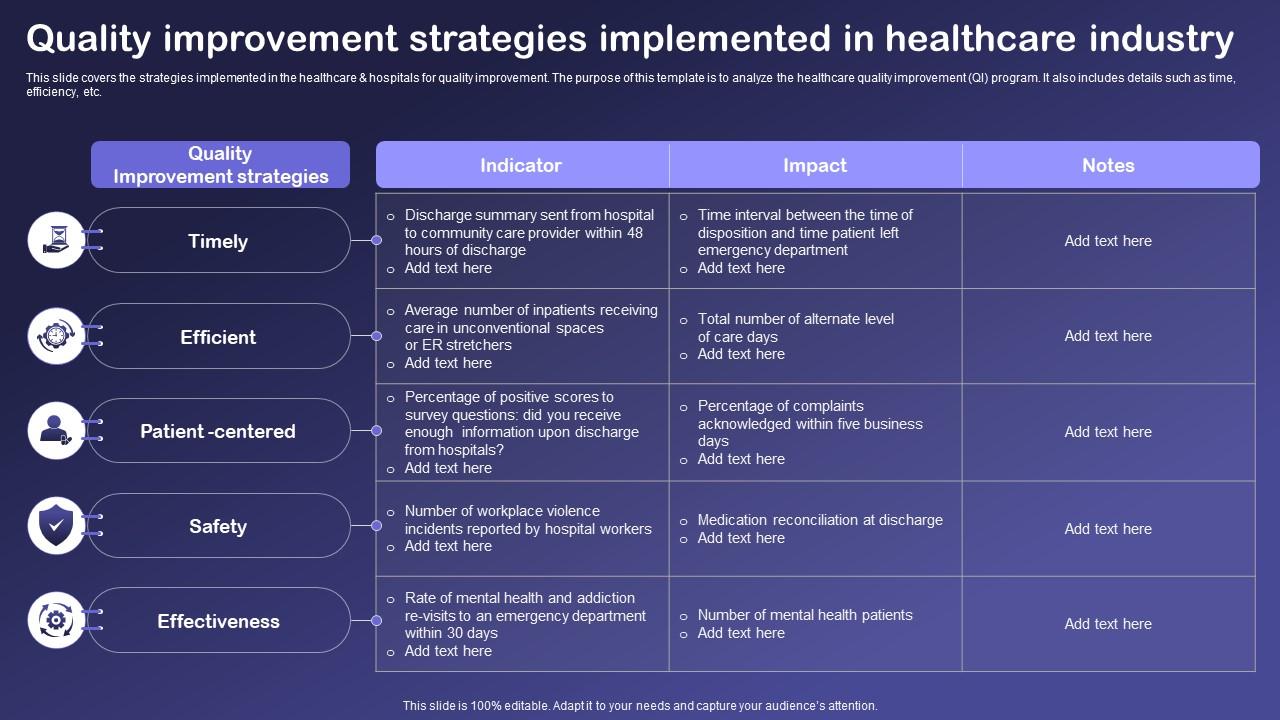
Numerous specific strategies fall under the umbrella of quality improvement. Implementing electronic health records (EHRs), for instance, enhances data collection and analysis, facilitating better clinical decision-making.
Standardizing clinical pathways ensures consistent and evidence-based care for patients with specific conditions. Conducting regular patient satisfaction surveys provides valuable feedback for identifying areas for improvement.
Focusing on medication reconciliation aims to reduce medication errors and improve patient safety. Team-based care models promote collaboration and communication among healthcare professionals.
Identifying the Exception
Consider the following options, and try to identify which one would be the *least* suited for a quality improvement strategy:
- Implementing a new electronic health record (EHR) system.
- Providing continuing education for staff on the latest medical guidelines.
- Rewarding employees based solely on seniority.
- Standardizing post-operative pain management protocols.
The answer is "Rewarding employees based solely on seniority." This practice, while potentially valuable in terms of employee recognition and retention, does not directly address a specific problem in healthcare delivery or aim to improve a measurable outcome.
Unlike the other options, rewarding seniority lacks a direct link to patient care quality or operational efficiency. It doesn't inherently drive improvement in processes, outcomes, or patient satisfaction.
Why Seniority-Based Rewards Aren't Always QI
Genuine quality improvement strategies are data-driven. They begin with identifying a specific problem or opportunity for improvement, collecting data to understand the current state, implementing an intervention, and then collecting data again to assess the impact of the intervention.
Rewarding employees based on seniority doesn't inherently involve this cycle. While experienced employees may contribute valuable insights and skills, simply rewarding them for their tenure doesn't guarantee improved performance or patient outcomes.
Furthermore, relying solely on seniority for rewards can potentially stifle innovation and discourage newer employees from contributing their ideas. A robust QI culture fosters a meritocratic environment where contributions are recognized and rewarded regardless of tenure.
The Importance of Targeted QI Initiatives
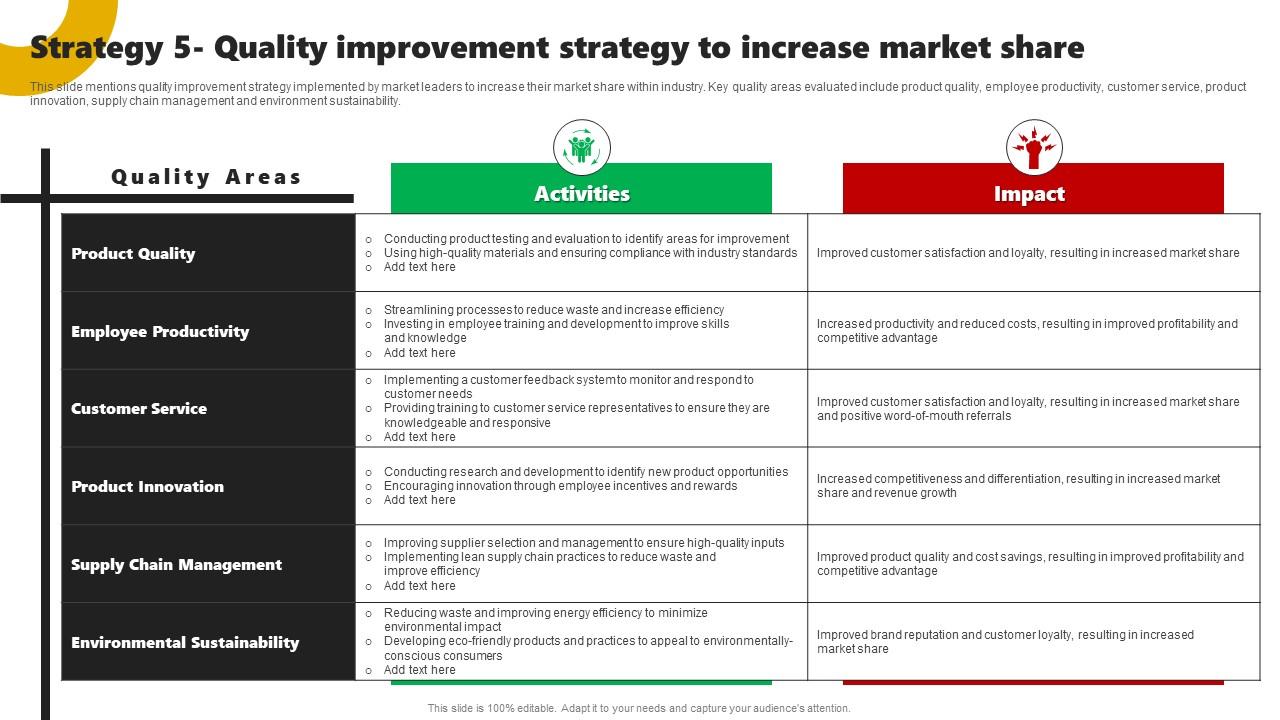
Effective QI requires a targeted approach. Healthcare organizations must carefully select initiatives that address their specific needs and priorities.
Implementing a new EHR system, for example, can significantly improve data management and clinical decision support, but only if it's integrated effectively and accompanied by adequate training for staff.
Similarly, standardizing post-operative pain management protocols can reduce variability in care and improve patient comfort, but it requires careful consideration of individual patient needs and preferences.
Conclusion: A Strategic Approach to Quality Improvement
While employee recognition programs can contribute to a positive work environment, it's crucial to distinguish them from genuine quality improvement strategies. QI initiatives must be data-driven, patient-centered, and focused on achieving measurable improvements in healthcare delivery.
Healthcare leaders must ensure that their QI efforts are aligned with their organization's strategic goals and that they are utilizing appropriate methodologies and tools to achieve desired outcomes. By adopting a strategic and evidence-based approach to quality improvement, healthcare organizations can create a culture of continuous learning and improvement, ultimately leading to better patient care and a more efficient and effective healthcare system.