Benign Prostatic Hyperplasia Vs Prostate Cancer

For men, the subtle whispers of urinary changes can trigger anxieties far beyond mere inconvenience. Is it simply the innocent bloat of an aging prostate, or does it herald a more sinister foe – prostate cancer? Differentiating between Benign Prostatic Hyperplasia (BPH) and prostate cancer is paramount, not only for peace of mind but for life-saving treatment.
This article unpacks the crucial distinctions between these two common prostate conditions. We'll delve into the symptoms, diagnostic approaches, treatment options, and the overarching importance of awareness and proactive screening. Understanding the nuances is the first step toward empowering men to take control of their prostate health.
Understanding Benign Prostatic Hyperplasia (BPH)
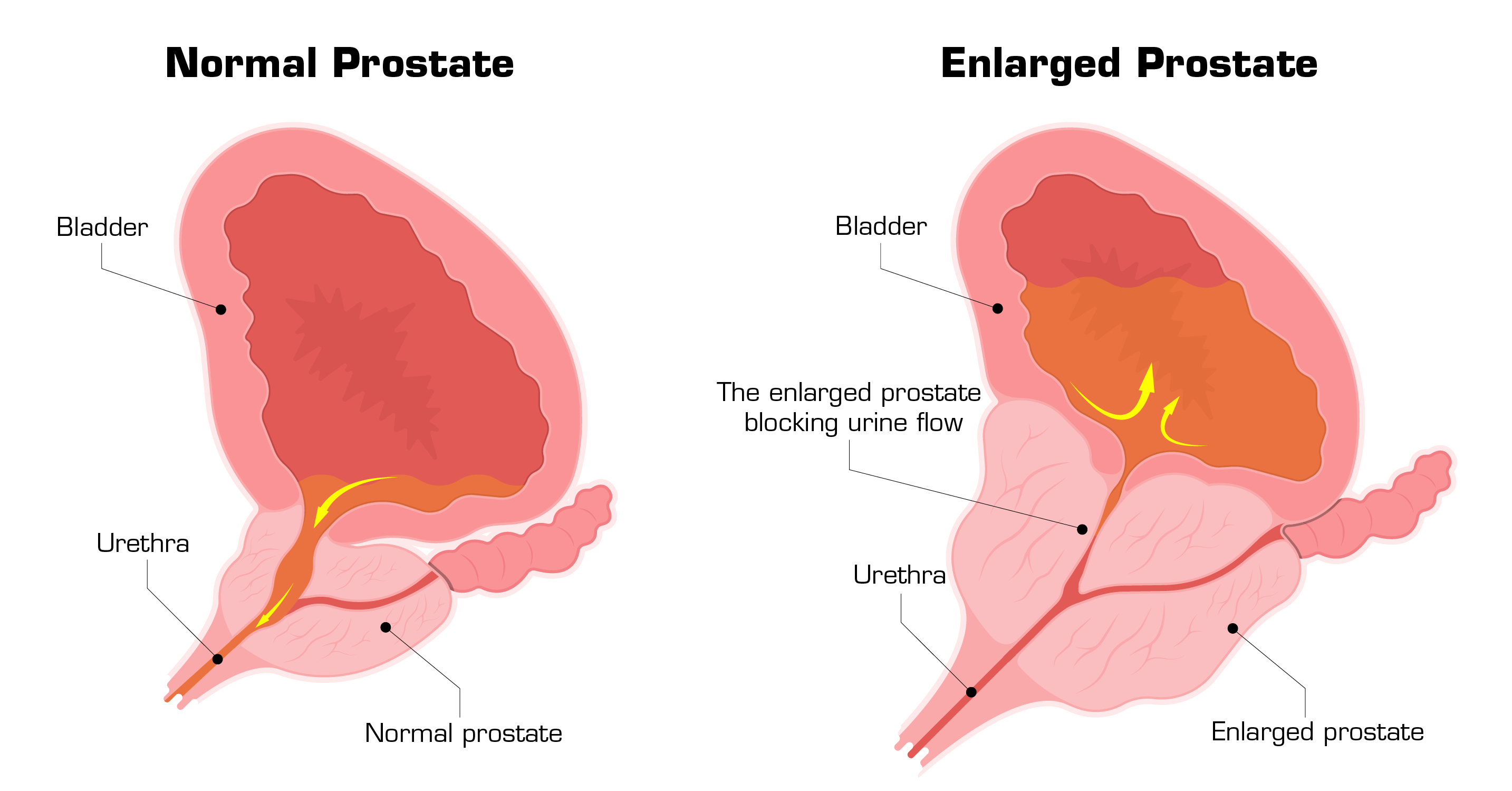
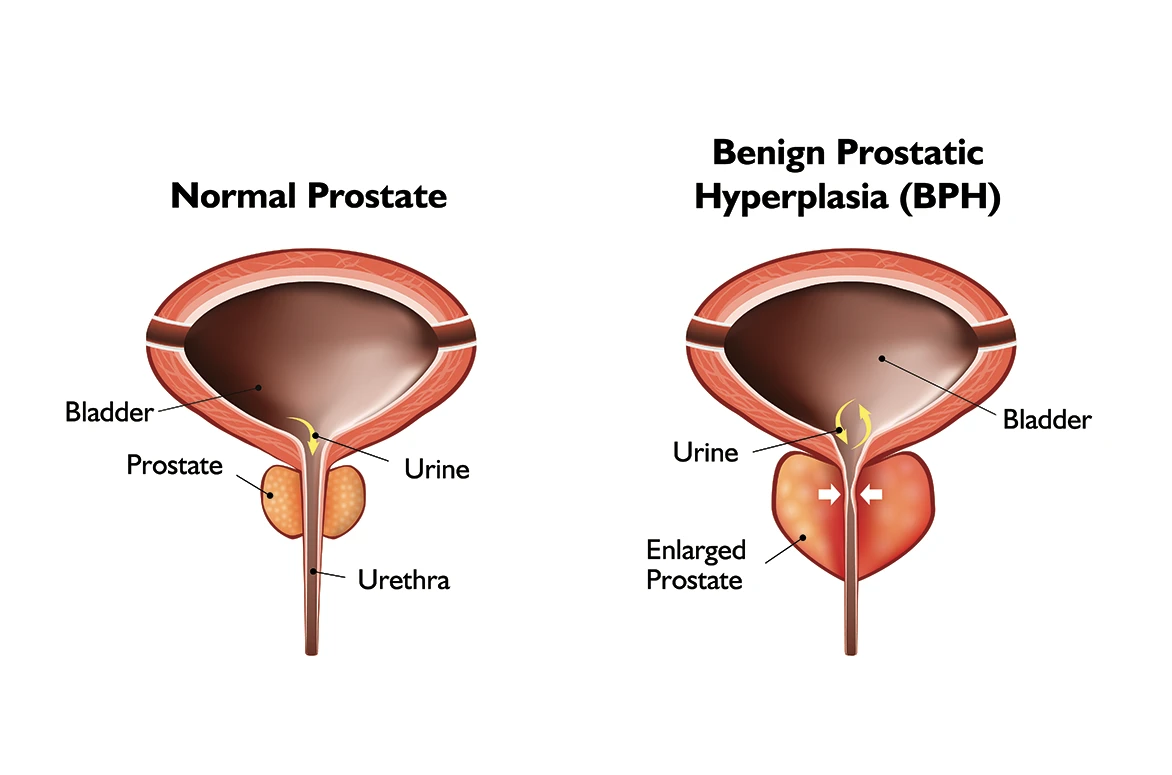
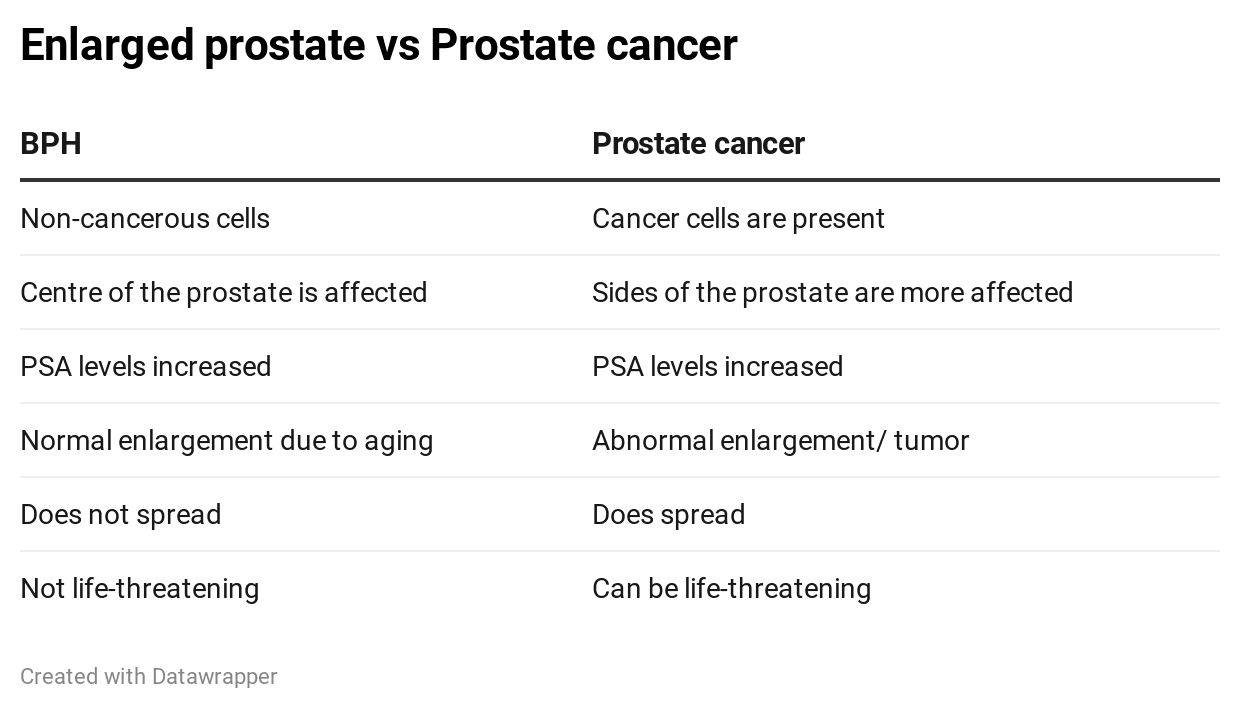
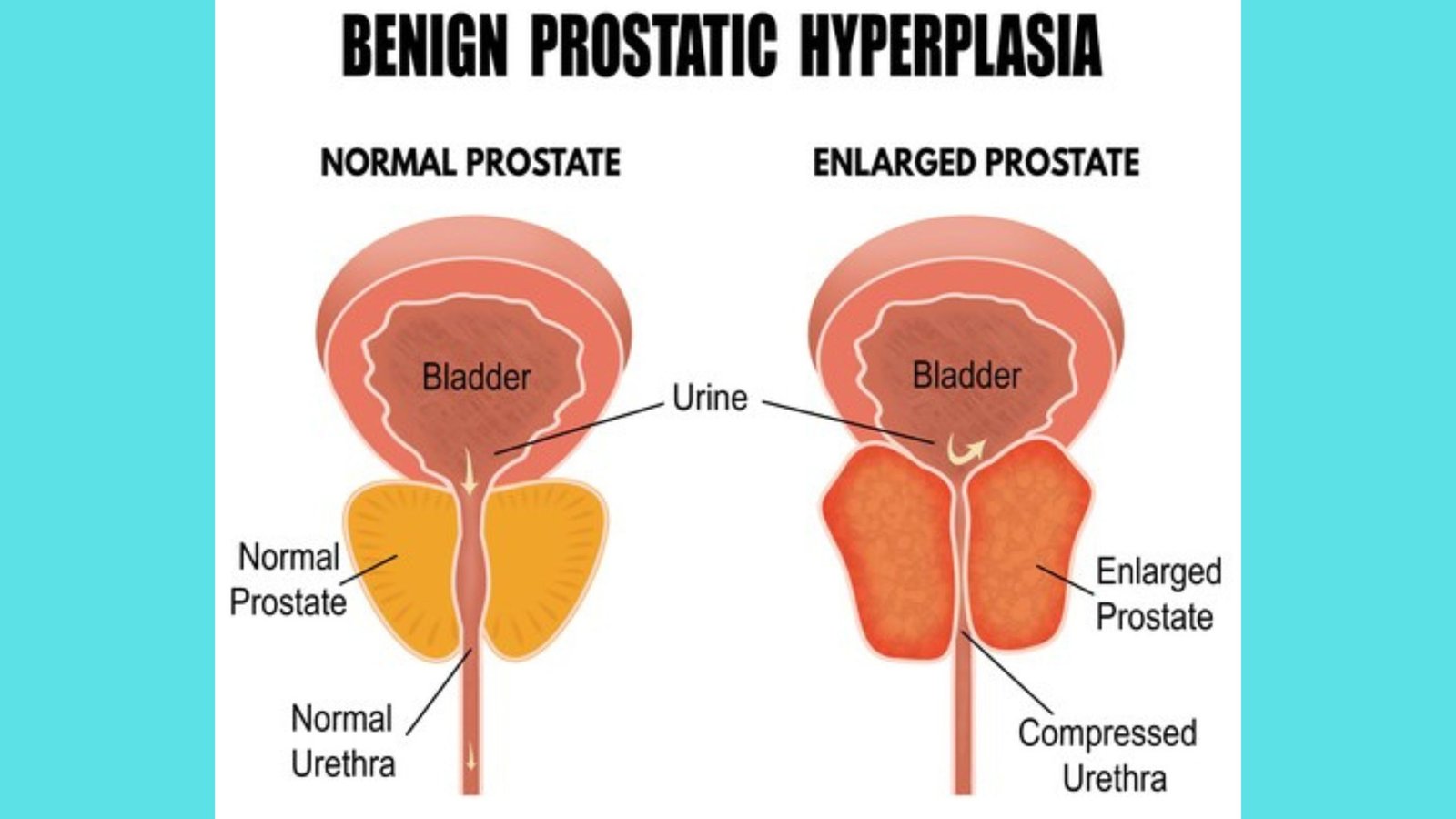
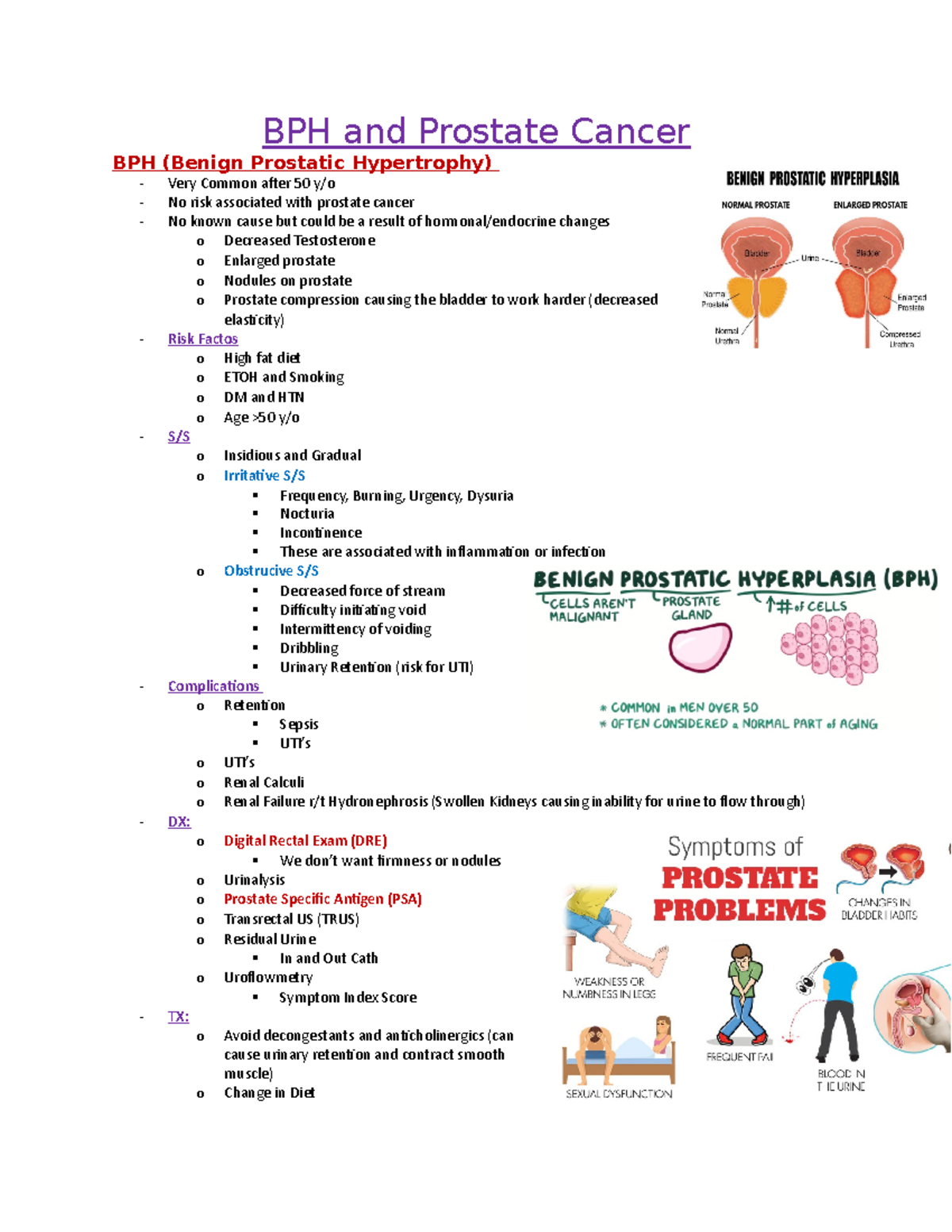
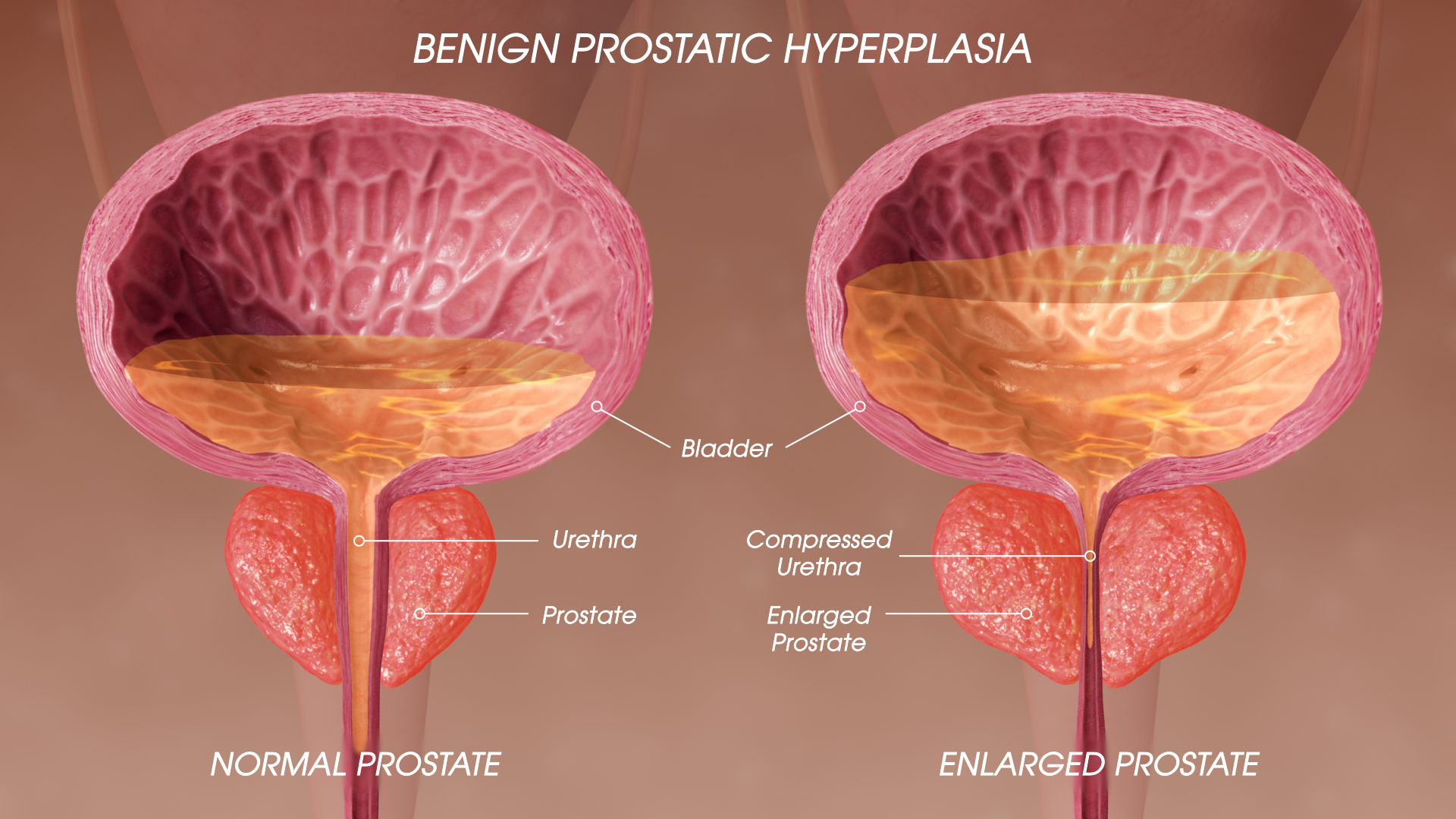
BPH, often described as prostate enlargement, is a non-cancerous condition. It is incredibly common, affecting a significant proportion of men as they age. The prostate gland, responsible for producing fluid for semen, gradually increases in size.
This enlargement can compress the urethra. This leads to a variety of urinary symptoms. These include frequent urination, especially at night (nocturia), difficulty starting urination, a weak urine stream, dribbling after urination, and a feeling of incomplete bladder emptying.
While bothersome, BPH does not directly increase the risk of prostate cancer. However, its symptoms can significantly impact quality of life, warranting medical intervention.
Prostate Cancer: A More Serious Threat
Prostate cancer, on the other hand, is a malignant tumor that develops in the prostate gland. It is the second most common cancer among men in the United States, according to the American Cancer Society. The severity of prostate cancer can range from slow-growing, less aggressive forms to more rapidly progressing, life-threatening types.
Early-stage prostate cancer often presents with no noticeable symptoms. This is why regular screening is so critical. As the cancer progresses, it may cause symptoms similar to BPH.
These overlapping symptoms include urinary frequency and difficulty urinating. Other indicators may include blood in the urine or semen, erectile dysfunction, and pain in the hips, back, or chest if the cancer has spread to the bones.
Key Differences in Symptoms
While both conditions can cause urinary problems, some subtle differences may hint at the underlying issue. The presence of blood in the urine or semen, or bone pain, is more indicative of prostate cancer. Rapidly worsening symptoms, especially with accompanying weight loss or fatigue, should also raise suspicion for cancer.
However, it's crucial to emphasize that symptoms alone are not enough for diagnosis. Definitive diagnosis requires medical evaluation and specific tests.
Diagnostic Approaches: Unraveling the Mystery
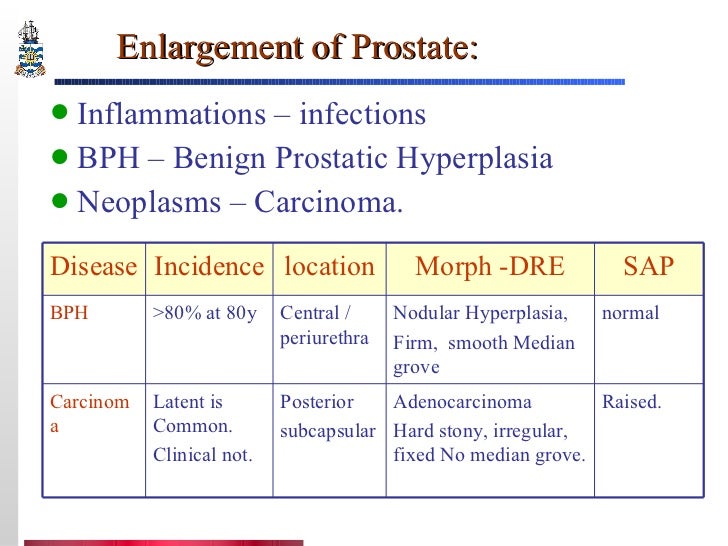
Differentiating between BPH and prostate cancer requires a comprehensive diagnostic approach. This typically begins with a physical examination, including a digital rectal exam (DRE). During a DRE, a doctor inserts a gloved, lubricated finger into the rectum to feel the prostate gland for any abnormalities in size, shape, or texture.
A prostate-specific antigen (PSA) blood test is also a standard part of the evaluation. PSA is a protein produced by both normal and cancerous prostate cells. Elevated PSA levels can indicate prostate enlargement, inflammation, infection, or cancer.
However, PSA levels can be influenced by various factors, making it an imperfect screening tool. Therefore, further investigation is often required if PSA levels are elevated.
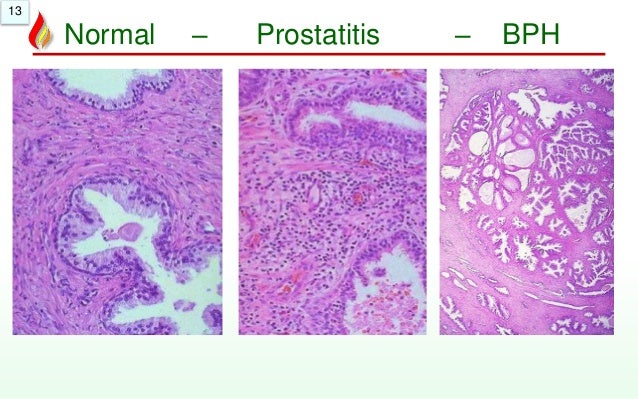
If the DRE or PSA test raises concerns, a prostate biopsy is typically performed. This involves taking small tissue samples from the prostate gland for microscopic examination. A biopsy is the only way to definitively diagnose prostate cancer and determine its grade, which indicates how aggressive the cancer is.
Additional Diagnostic Tools
In addition to DRE, PSA, and biopsy, other diagnostic tools may be used. These include transrectal ultrasound (TRUS), which provides an image of the prostate gland. Magnetic resonance imaging (MRI) can offer more detailed images and help guide biopsies.
Treatment Options: A Tailored Approach
Treatment for BPH and prostate cancer differs significantly, reflecting the distinct nature of each condition. BPH treatment aims to relieve symptoms and improve quality of life. This can include lifestyle modifications, such as limiting fluid intake before bed and avoiding caffeine and alcohol.
Medications like alpha-blockers and 5-alpha reductase inhibitors can help relax the prostate muscles and shrink the gland, respectively. Minimally invasive procedures, such as transurethral resection of the prostate (TURP), can remove excess prostate tissue to alleviate urinary obstruction. In some cases, surgery may be necessary to remove part or all of the prostate.
Prostate cancer treatment depends on several factors. These include the stage and grade of the cancer, the patient's age and overall health, and their personal preferences. Treatment options may include active surveillance, surgery (radical prostatectomy), radiation therapy, hormone therapy, chemotherapy, and immunotherapy.
Active surveillance involves closely monitoring the cancer without immediate treatment. This approach is often used for slow-growing, low-risk cancers.
The Importance of Early Detection and Screening
Early detection is crucial for both BPH and prostate cancer. While BPH isn't life-threatening, untreated symptoms can lead to complications. These complications include urinary tract infections, bladder stones, and kidney damage. Early detection of prostate cancer significantly improves treatment outcomes. It increases the chances of successful eradication or management of the disease.
Screening recommendations for prostate cancer vary depending on individual risk factors. The American Urological Association recommends that men aged 55 to 69 discuss prostate cancer screening with their doctor. This is especially true for men with a family history of prostate cancer or African American men, who have a higher risk of developing the disease.
Shared decision-making between patients and their doctors is essential. This allows individuals to make informed choices about screening based on their specific circumstances.
Looking Ahead: Future Directions in Prostate Health
Research continues to advance our understanding of BPH and prostate cancer. It leads to improved diagnostic tools and treatment strategies. New imaging techniques and biomarkers are being developed to enhance early detection and risk assessment.
Targeted therapies and immunotherapies are showing promise in treating advanced prostate cancer. These precision medicine approaches aim to personalize treatment based on the individual characteristics of the cancer.
Raising awareness about prostate health is paramount. Empowering men to proactively engage in screening and seek medical attention for any concerning symptoms can save lives. It's critical to remember that open communication with healthcare providers is key to maintaining optimal prostate health throughout life.