Blood Collection For Therapeutic Drug Monitoring Requires

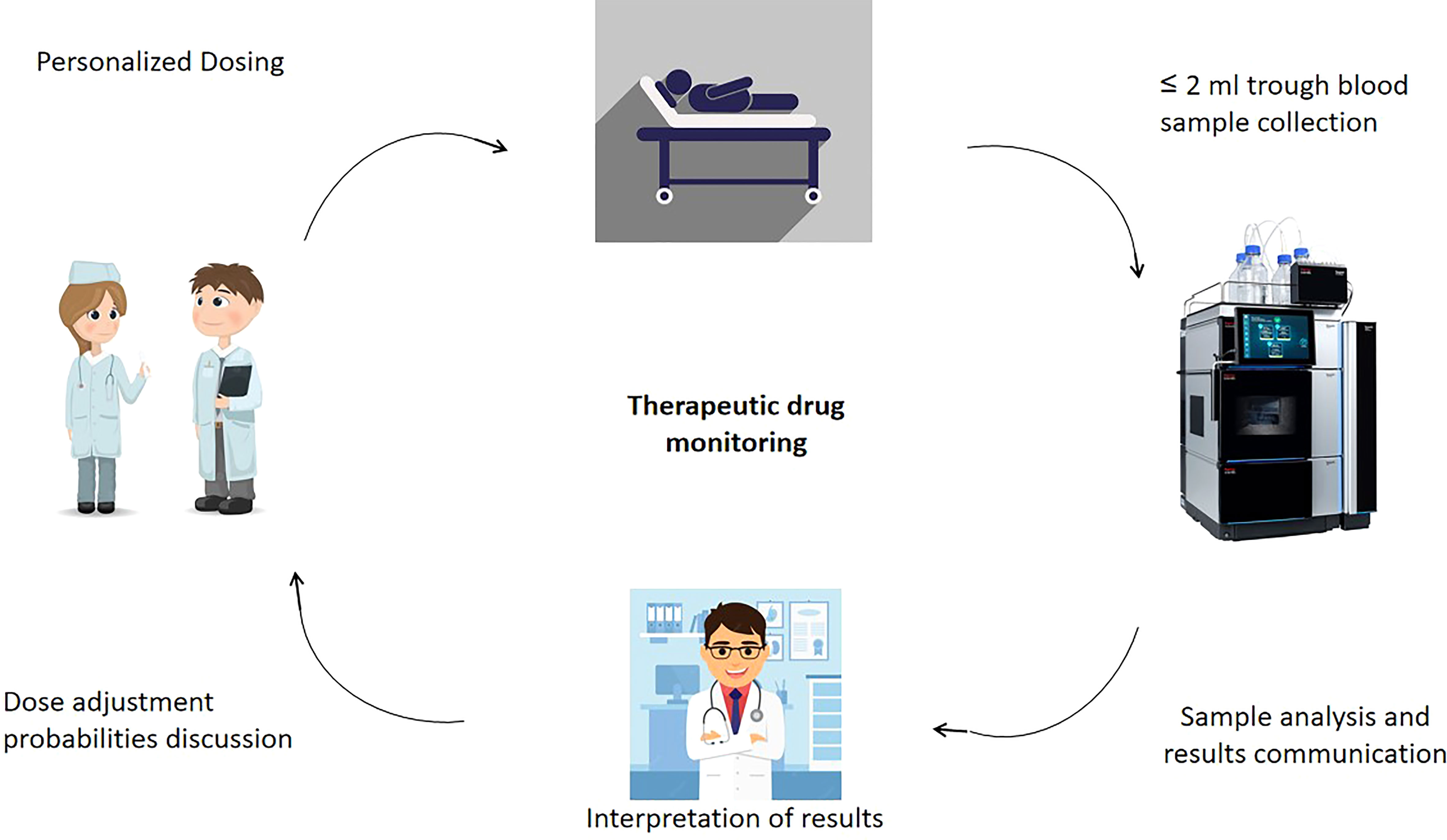
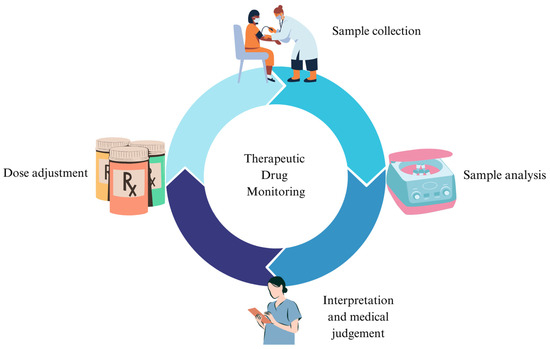
A silent revolution is underway in how doctors personalize medicine, driven by increasingly precise methods of monitoring drug levels in patients' blood. This revolution, however, hinges on a seemingly mundane but critically important aspect: blood collection. Errors in this process, from improper timing to incorrect handling, can compromise the accuracy of therapeutic drug monitoring (TDM), potentially leading to misinformed clinical decisions and jeopardizing patient safety.
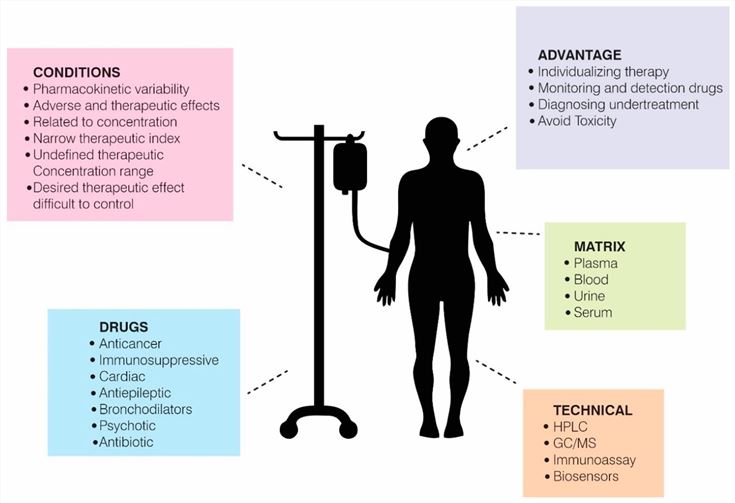
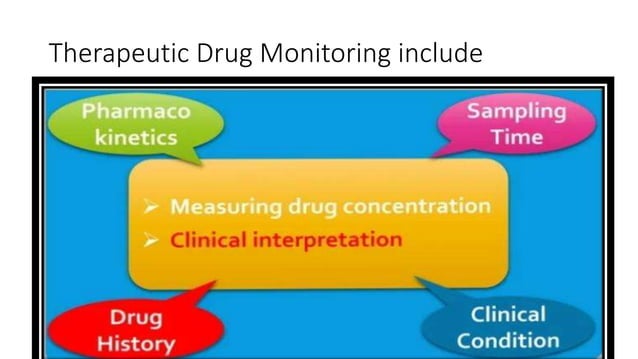
The effectiveness of TDM, the practice of measuring drug concentrations in a patient's blood, serum, or plasma, is directly linked to the quality of the blood sample collected. This article will delve into the intricate requirements for blood collection in TDM, highlighting the potential pitfalls, best practices, and the future of this essential component of personalized medicine. It will explore the impact of pre-analytical variables on TDM results and the crucial role of standardized procedures in ensuring reliable and actionable data for clinicians.
The Critical Role of Pre-Analytical Variables
The journey of a blood sample, from the patient's vein to the laboratory analyzer, is fraught with potential errors. These errors, referred to as pre-analytical variables, can significantly alter drug concentrations and skew TDM results.
Timing is paramount. Many drugs exhibit peak and trough concentrations, meaning their levels fluctuate significantly throughout the dosing interval. Therefore, blood samples must be drawn at specific times relative to the drug administration to accurately reflect the drug's exposure profile, according to guidelines published by the International Association of Therapeutic Drug Monitoring and Clinical Toxicology (IATDMCT).
Furthermore, improper blood collection tubes can introduce contamination or interact with the drug, affecting its measured concentration. Hemolysis, the rupture of red blood cells, is another common pre-analytical error that can interfere with TDM assays.
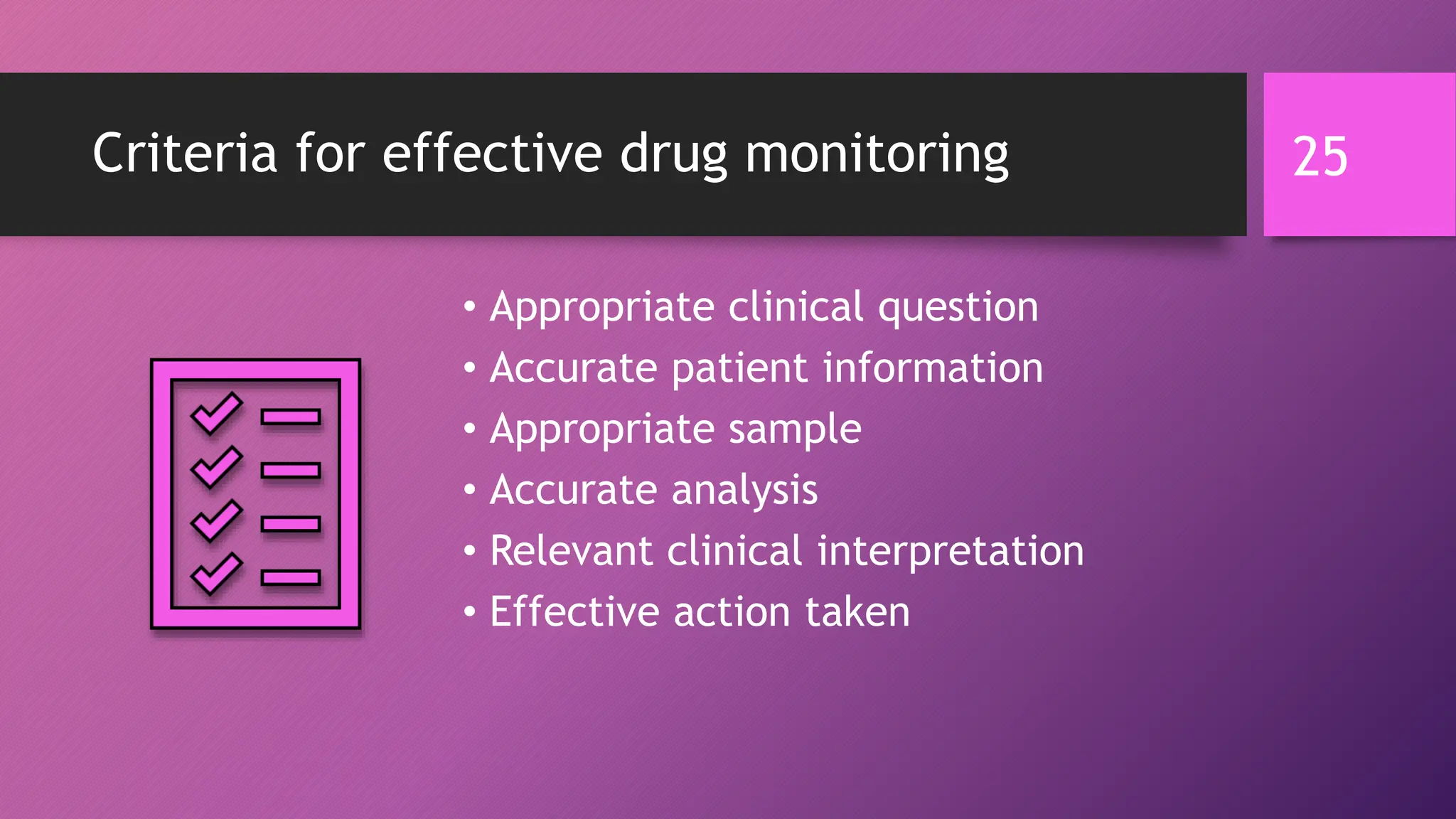
These variables emphasize the need for meticulously standardized protocols and adequately trained personnel to ensure the integrity of blood samples intended for TDM.
Specific Drug Considerations
The requirements for blood collection in TDM vary depending on the specific drug being monitored. For example, certain immunosuppressants, like tacrolimus and cyclosporine, require collection in specific tubes with particular anticoagulants to prevent drug binding to the tube material.
Drugs with narrow therapeutic windows, such as vancomycin, necessitate precise timing of blood collection to accurately assess trough levels and avoid toxicity. In cases where therapeutic window is close, deviations from recommended procedures can have serious consequences for patient care.
Furthermore, the patient's physiological state, including factors like hydration status and co-administered medications, can also influence drug concentrations and must be considered when interpreting TDM results.
Standardized Procedures and Training
To minimize the impact of pre-analytical variables, laboratories and healthcare institutions must implement standardized procedures for blood collection. This includes detailed protocols for timing, tube selection, venipuncture technique, and sample handling.
Comprehensive training for phlebotomists and other healthcare personnel involved in blood collection is also essential. This training should cover the principles of TDM, the importance of pre-analytical variables, and the specific requirements for collecting blood samples for different drugs.
Some institutions utilize checklists and visual aids to ensure adherence to standardized procedures. Additionally, real-time data entry to monitor performance, along with regular audits, can identify areas for improvement and promote continuous quality enhancement.
"Standardization is the cornerstone of reliable TDM. Without it, we risk making clinical decisions based on inaccurate or misleading data," states Dr. Emily Carter, a clinical pharmacologist at the Mayo Clinic.
The Impact of Technology
Technological advancements are playing an increasingly important role in improving the accuracy and efficiency of blood collection for TDM. Point-of-care testing (POCT) devices allow for rapid drug concentration measurements at the patient's bedside, eliminating the need for transportation to a central laboratory and reducing the potential for pre-analytical errors.
Micro-sampling techniques, such as dried blood spot (DBS) analysis, require only small volumes of blood, which can be collected with minimal invasiveness. DBS offers the advantage of easy sample transport and storage, making it suitable for remote monitoring and home-based TDM.
Furthermore, electronic health records (EHRs) can be integrated with TDM systems to automate order entry, sample tracking, and result reporting, reducing the risk of transcription errors and improving data integrity.
Patient Involvement and Education
Patient participation plays a crucial role in successful TDM. Patients must be educated about the importance of adhering to their medication regimen and attending scheduled blood draws. They also need to understand the potential impact of factors like food intake, concurrent medications, and lifestyle choices on their drug levels.
Clear and concise communication between healthcare providers and patients is paramount. Patients should be provided with detailed instructions on how to prepare for blood draws, including any dietary restrictions or medication adjustments.
In some cases, patients may be able to participate in self-monitoring using home-based devices, which can empower them to take control of their health and improve treatment outcomes.
Looking Ahead
The future of blood collection for TDM is likely to be shaped by further technological advancements and a greater emphasis on personalized medicine. Minimally invasive sampling techniques, such as microneedle arrays and wearable sensors, may offer even less invasive and more convenient alternatives to traditional venipuncture.
Artificial intelligence (AI) and machine learning (ML) algorithms could be used to analyze TDM data and predict drug concentrations, optimizing dosing regimens and improving patient outcomes. The use of AI could flag potential pre-analytical errors, offering an extra layer of quality control.
However, even with these advancements, the fundamental principles of accurate and reliable blood collection will remain paramount. By adhering to standardized procedures, investing in training, and embracing new technologies, healthcare professionals can ensure that TDM delivers its full potential to improve patient care.