Bone Marrow Transplant And Sickle Cell Disease
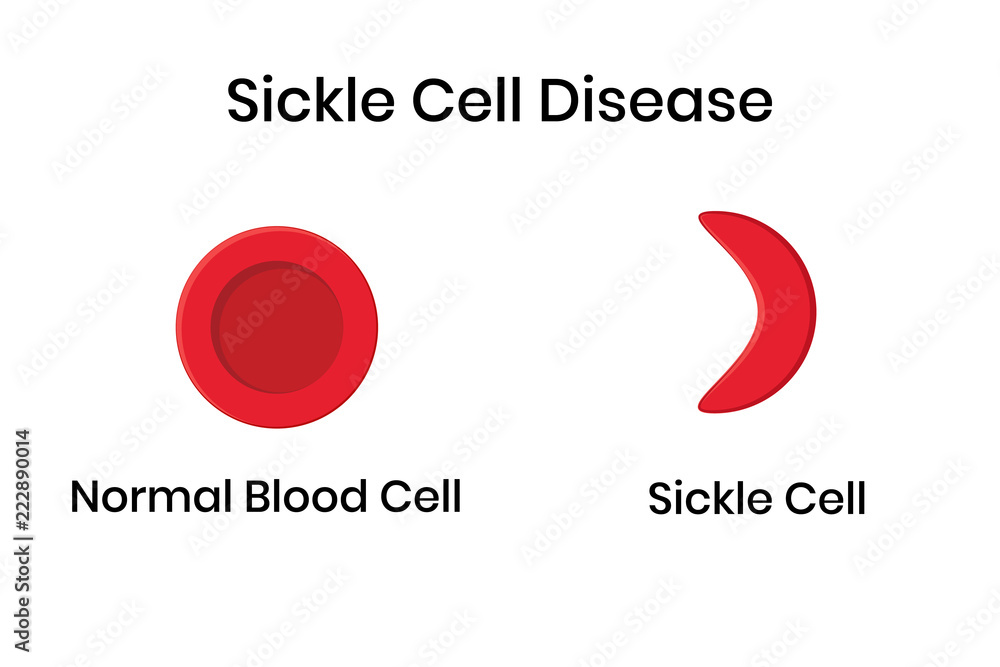
For decades, sickle cell disease (SCD), a debilitating inherited blood disorder affecting millions globally, has presented a formidable challenge to medical science. While advancements in pain management and supportive care have improved the quality of life for many, a curative option has remained elusive. Now, bone marrow transplant (BMT), also known as hematopoietic stem cell transplant (HSCT), is emerging as a potentially life-saving intervention, offering the promise of a future free from the agonizing pain and life-threatening complications of SCD.
This article explores the complex landscape of BMT for SCD. It examines the procedure itself, its benefits and risks, the challenges associated with finding suitable donors, and the long-term outcomes for patients. Furthermore, it will delve into the ongoing research aimed at expanding access to this potentially curative therapy and making it safer and more effective, offering a glimpse into the future of SCD treatment.
Understanding Bone Marrow Transplant for Sickle Cell Disease
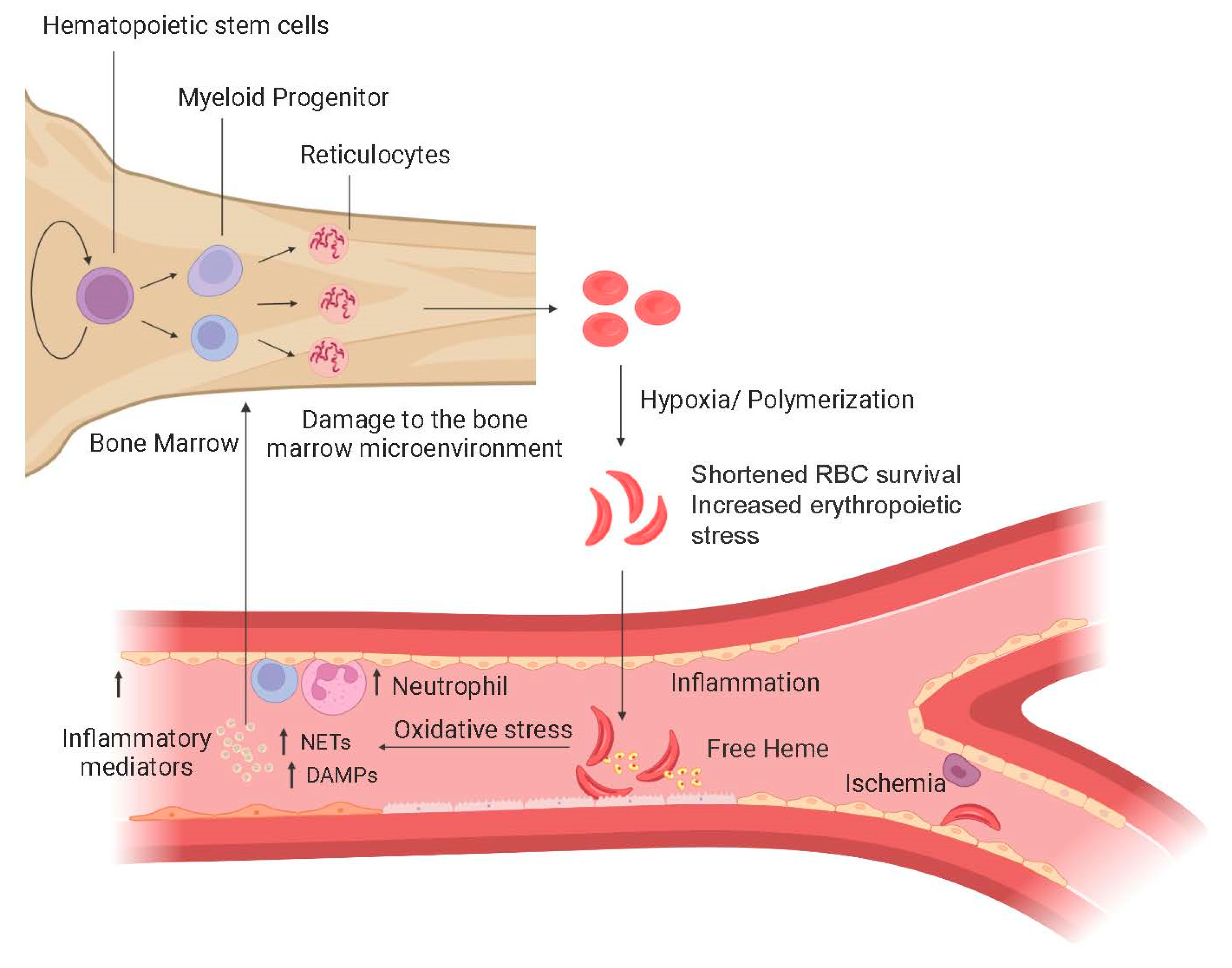
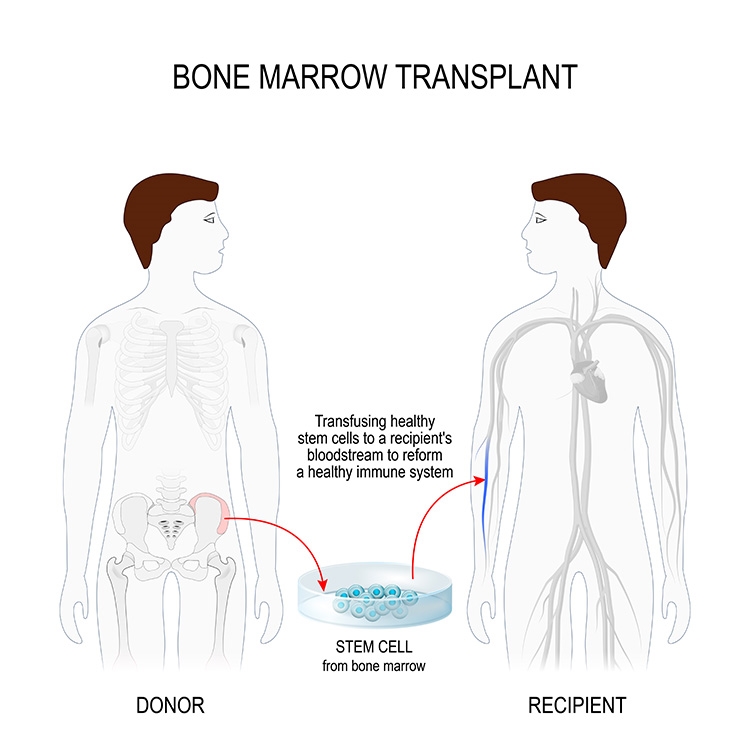
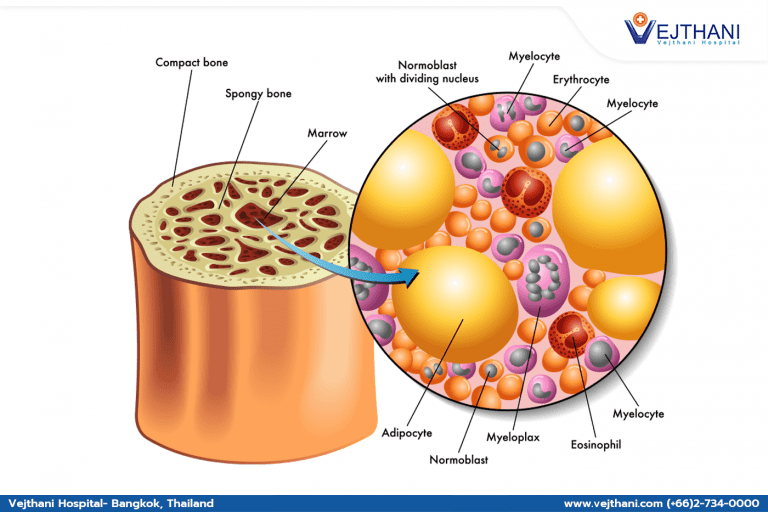
Bone marrow transplant is a complex medical procedure that involves replacing a patient's damaged or diseased bone marrow with healthy stem cells. These stem cells then develop into healthy blood cells, including red blood cells that do not sickle.
In the context of SCD, BMT aims to replace the patient's faulty bone marrow, which produces the abnormal hemoglobin characteristic of the disease, with healthy bone marrow from a donor. This essentially "reboots" the patient's blood production system, enabling it to produce normal red blood cells.
The Procedure: A Step-by-Step Overview
The BMT process typically begins with a rigorous evaluation of the patient to determine their suitability for the procedure. This includes assessing their overall health, the severity of their SCD, and the availability of a suitable donor.
Next, the patient undergoes conditioning therapy, which usually involves high doses of chemotherapy, sometimes combined with radiation. This intensive treatment aims to destroy the patient's existing bone marrow, creating space for the new, healthy stem cells to engraft and grow.
Once the conditioning therapy is complete, the healthy stem cells from the donor are infused into the patient's bloodstream. These cells then travel to the bone marrow, where they ideally begin to grow and produce healthy blood cells.
Finding a Matching Donor: A Critical Hurdle
A critical factor in the success of BMT is finding a matched donor. Ideally, this would be a sibling with a perfectly matched human leukocyte antigen (HLA) type.
However, only about 30% of patients have a matched sibling donor, making the search for unrelated donors crucial. National and international bone marrow registries play a vital role in connecting patients with potential unrelated donors who have a compatible HLA type.
"The availability of matched donors remains a significant barrier for many patients, particularly those from underrepresented ethnic backgrounds," says Dr. Emily Carter, a hematologist specializing in BMT at the National Institutes of Health (NIH).
Benefits and Risks: Weighing the Options
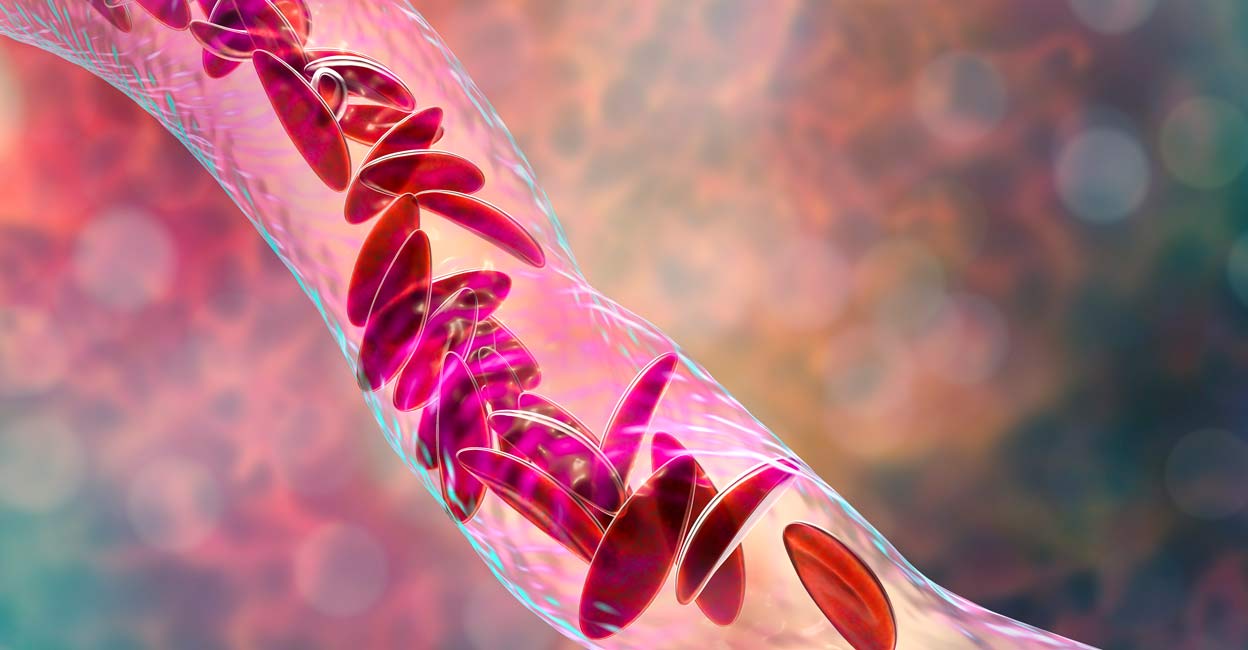
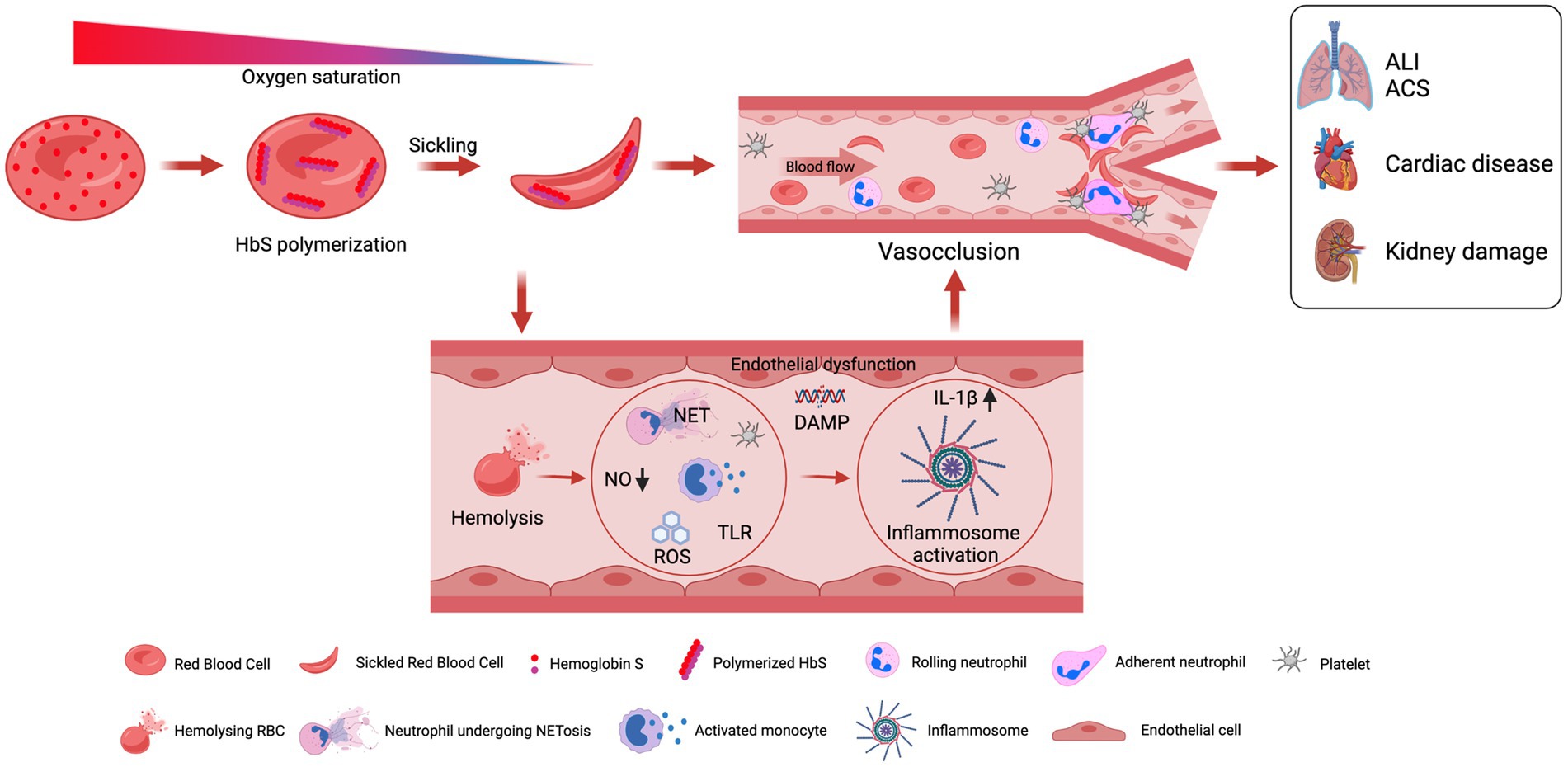
The primary benefit of BMT for SCD is the potential for a cure. Successful BMT can eliminate the need for chronic blood transfusions, reduce the risk of vaso-occlusive crises (painful episodes caused by sickled red blood cells blocking blood flow), and prevent organ damage associated with SCD.
However, BMT is not without risks. The conditioning therapy can cause significant side effects, including nausea, vomiting, fatigue, and increased susceptibility to infections.
A major complication is graft-versus-host disease (GVHD), where the donor's immune cells attack the recipient's tissues. GVHD can range from mild to life-threatening and requires immunosuppressive medications to manage.
Long-Term Outcomes: A Mixed Bag
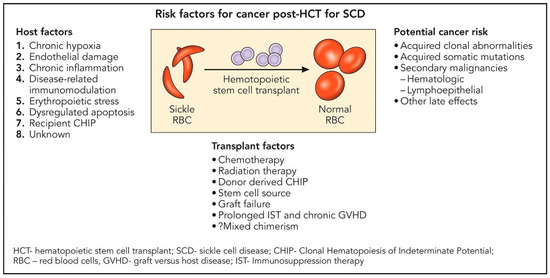
Long-term outcomes after BMT for SCD vary depending on factors such as the patient's age, the severity of their disease, the degree of HLA matching, and the development of complications like GVHD. Studies have shown that BMT can lead to long-term disease-free survival in a significant proportion of patients.
A study published in the journal Blood followed patients who underwent BMT for SCD for over 10 years. It found that approximately 85% of patients experienced long-term disease-free survival.
Despite these promising results, long-term follow-up is essential to monitor for potential late complications, such as secondary cancers and organ damage. Patients who undergo BMT require ongoing medical care and monitoring for the rest of their lives.
The Future of Bone Marrow Transplant for Sickle Cell Disease
Researchers are actively exploring ways to improve the safety and effectiveness of BMT for SCD. One promising area of research is haploidentical transplant, which involves using stem cells from a partially matched donor, such as a parent or half-sibling.
Another area of focus is gene therapy. Gene therapy involves modifying the patient's own stem cells to correct the genetic defect that causes SCD. These modified cells are then transplanted back into the patient, eliminating the need for a donor.
"Gene therapy holds immense promise for SCD patients who lack a matched donor or are not eligible for traditional BMT," explains Dr. David Williams, a leading researcher in gene therapy for SCD at Boston Children's Hospital.
Reduced-intensity conditioning regimens are also being investigated to minimize the toxic effects of chemotherapy. These regimens use lower doses of chemotherapy, reducing the risk of side effects and making BMT a more viable option for older patients or those with pre-existing health conditions.
The journey of bone marrow transplant in treating sickle cell disease is a testament to medical innovation and the unwavering pursuit of a cure. As research continues to unfold, the hope for a future free from the burden of SCD becomes increasingly tangible, offering new possibilities for affected individuals and their families.