Cell Signaling How Is Glucose Taken Up By Cells
The intricate dance between glucose and our cells, a fundamental process powering life itself, relies on a sophisticated cell signaling network. Understanding how cells absorb glucose is crucial for comprehending energy metabolism, and malfunctions in this process are implicated in diseases like diabetes.
This article explores the mechanisms behind glucose uptake, the key players involved in the signaling cascade, and the implications for health and disease.
The Glucose Gateway: GLUT Transporters
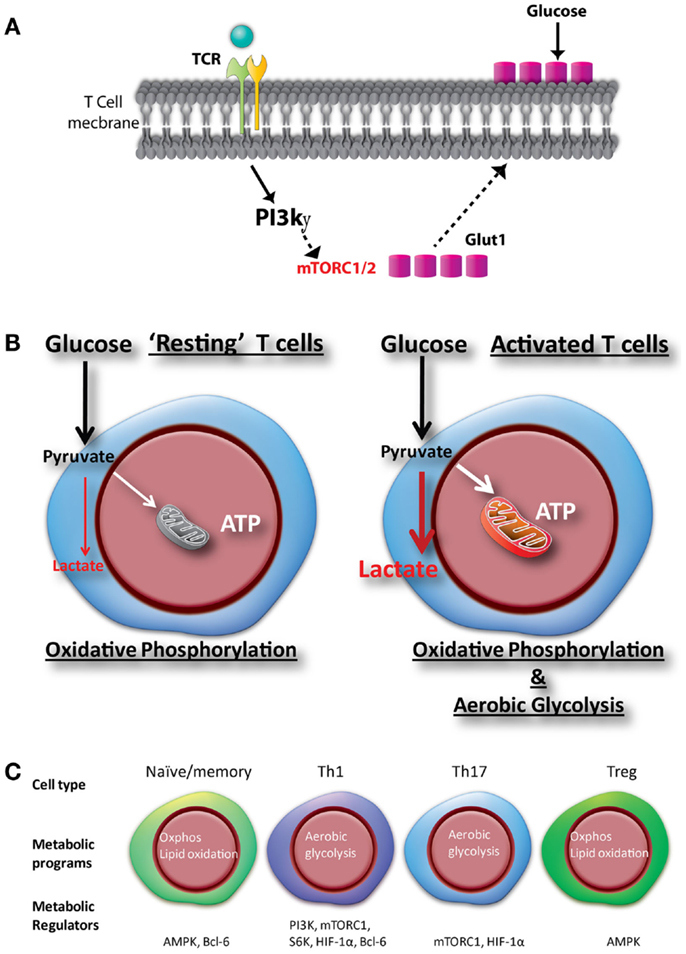
Glucose, the primary energy source for many cells, cannot simply diffuse across the cell membrane.
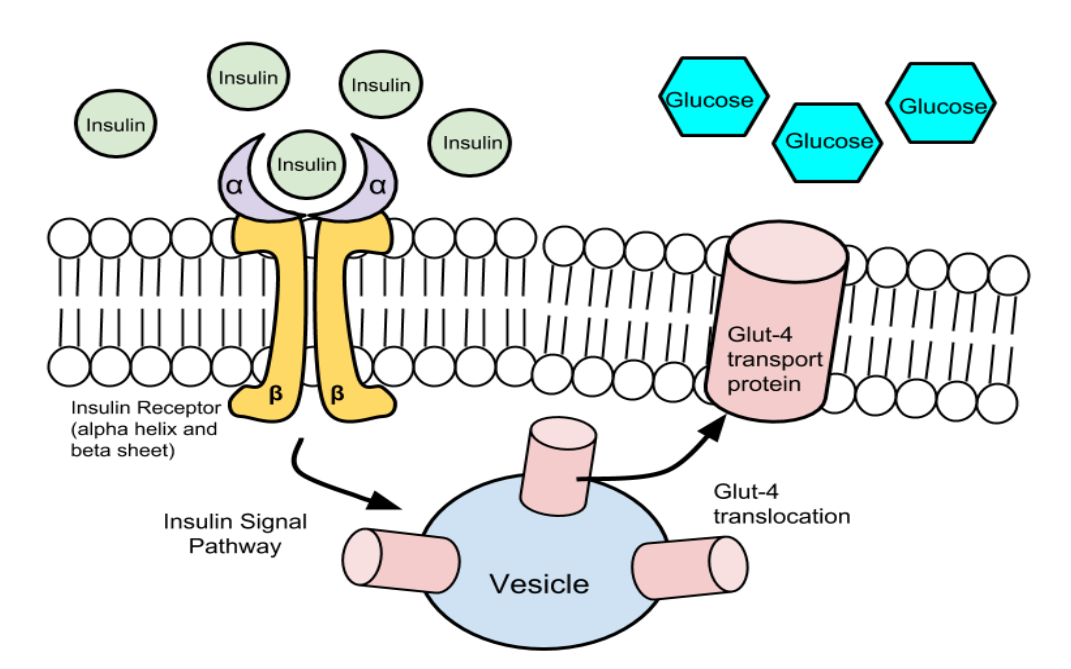
Instead, it requires specialized protein transporters called GLUTs (Glucose Transporters) to facilitate its entry.
Different GLUT isoforms exist, each with varying affinities for glucose and tissue-specific expression patterns.
For instance, GLUT4, predominantly found in muscle and fat cells, plays a vital role in insulin-regulated glucose uptake.
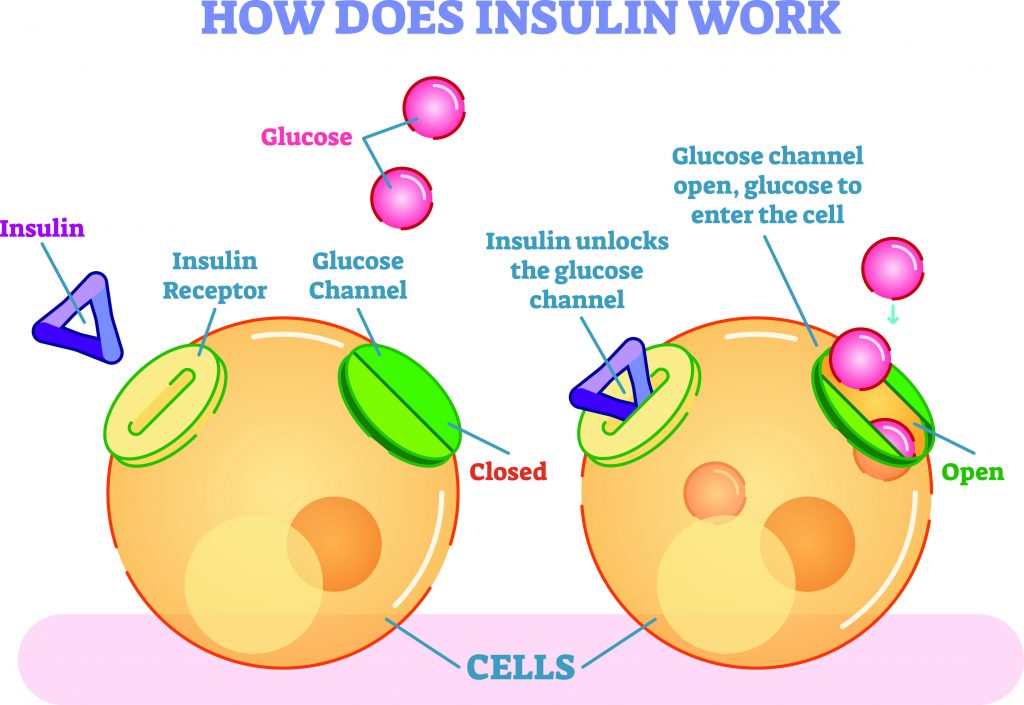
Insulin's Role: A Key Regulator
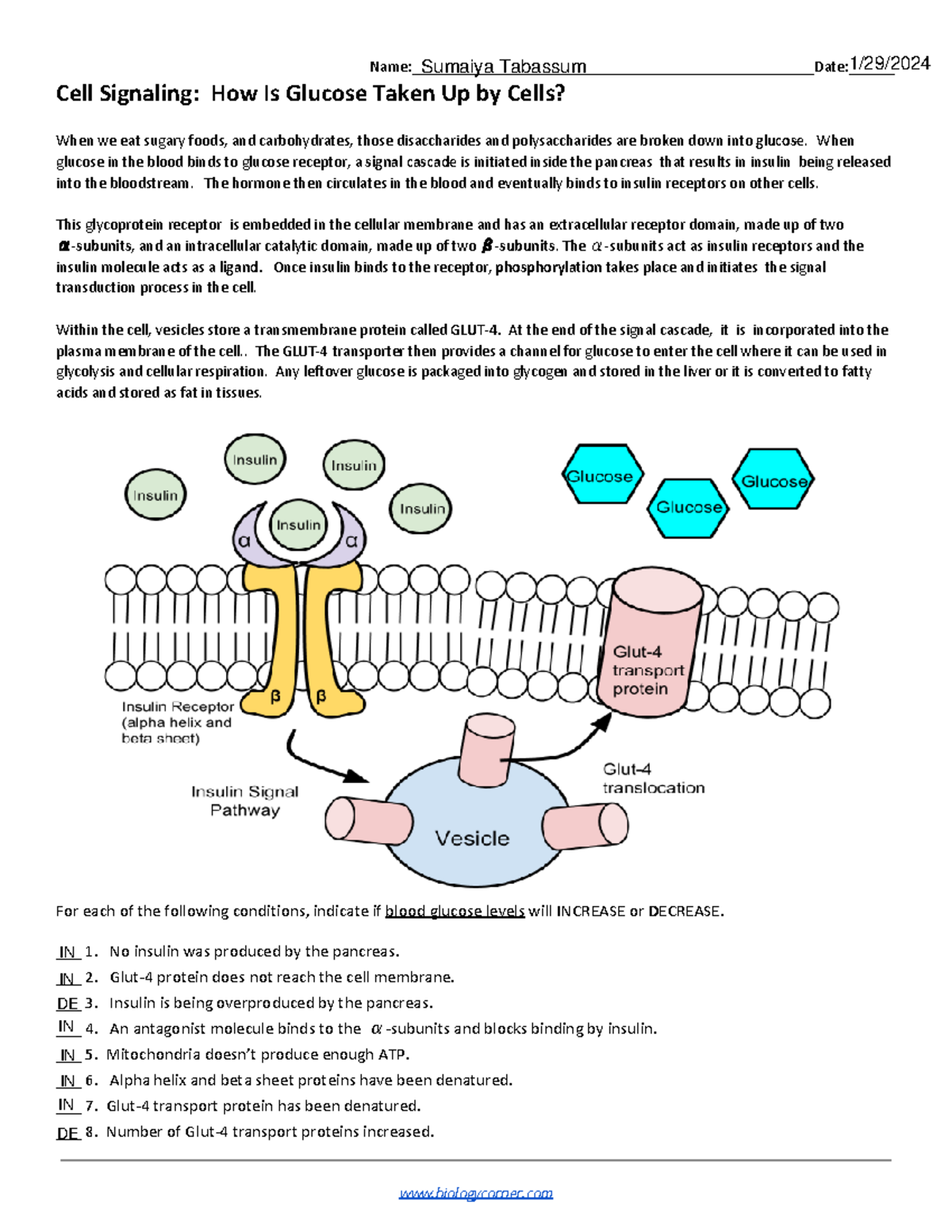
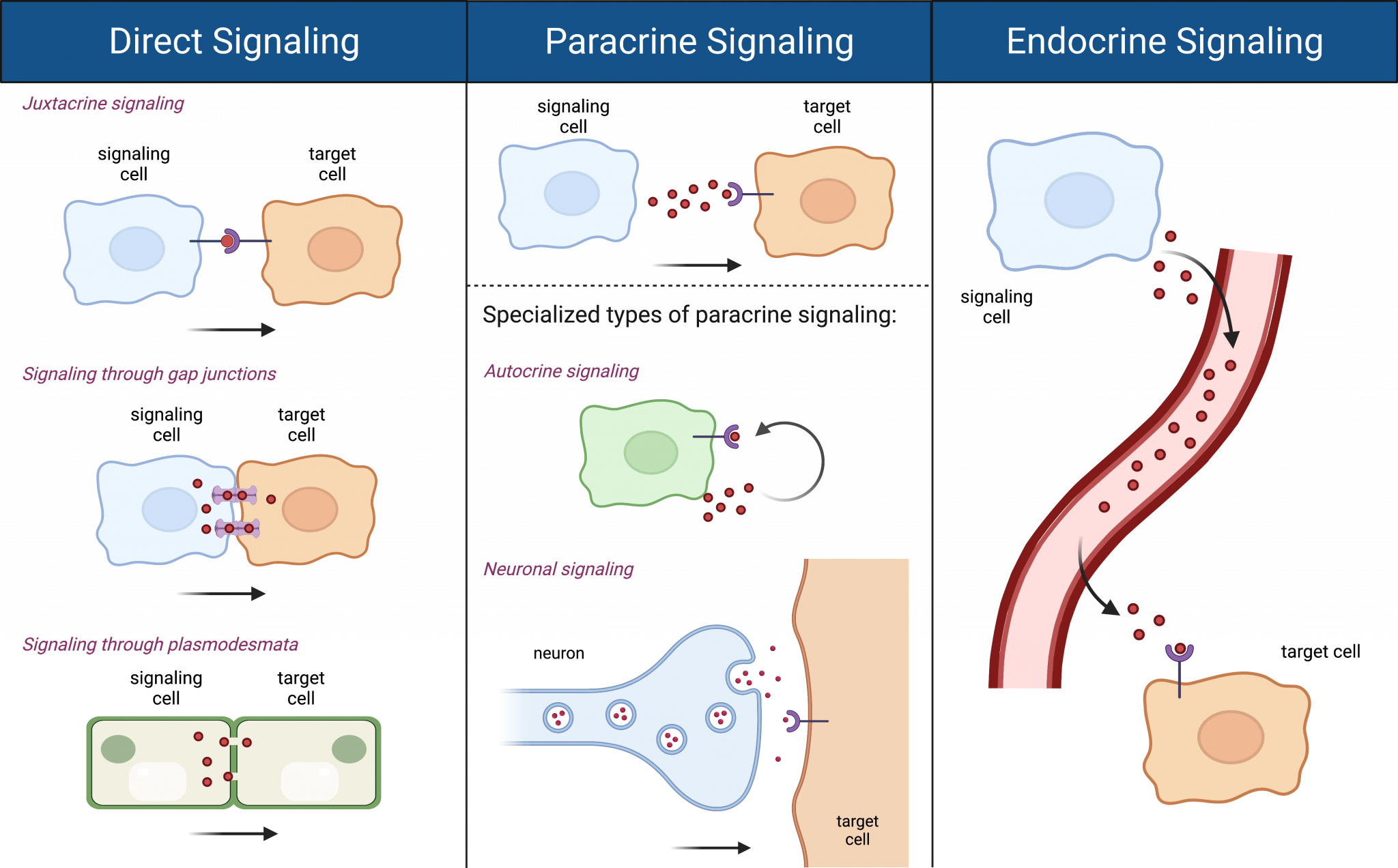
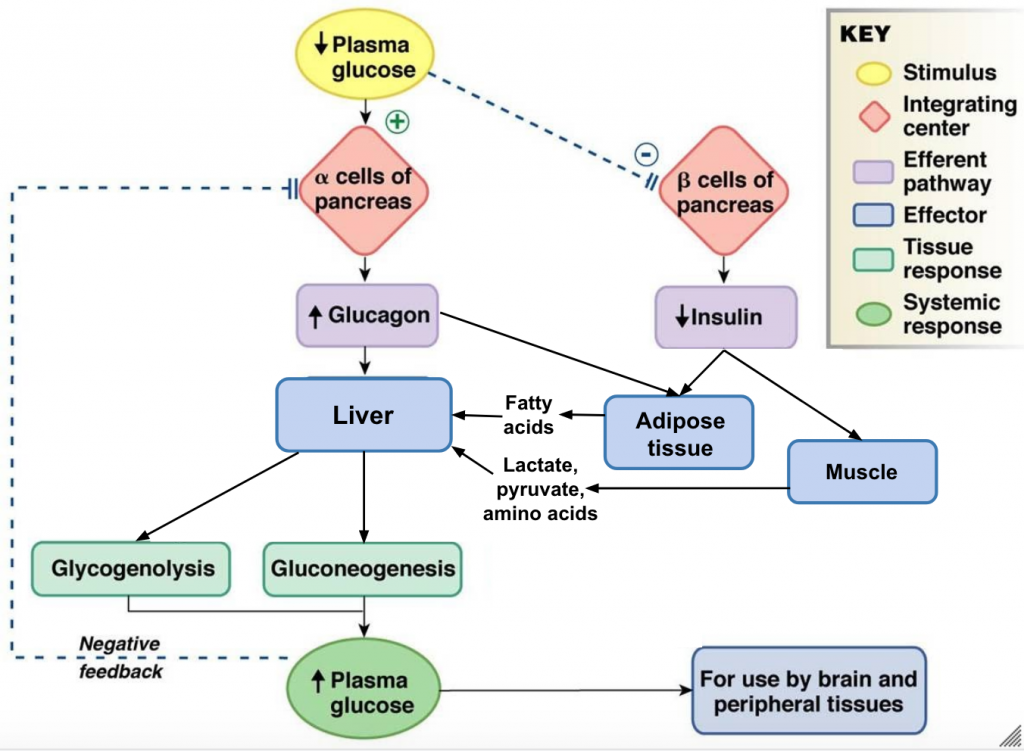
Insulin, a hormone secreted by the pancreas in response to elevated blood glucose levels, acts as a master regulator of glucose uptake.
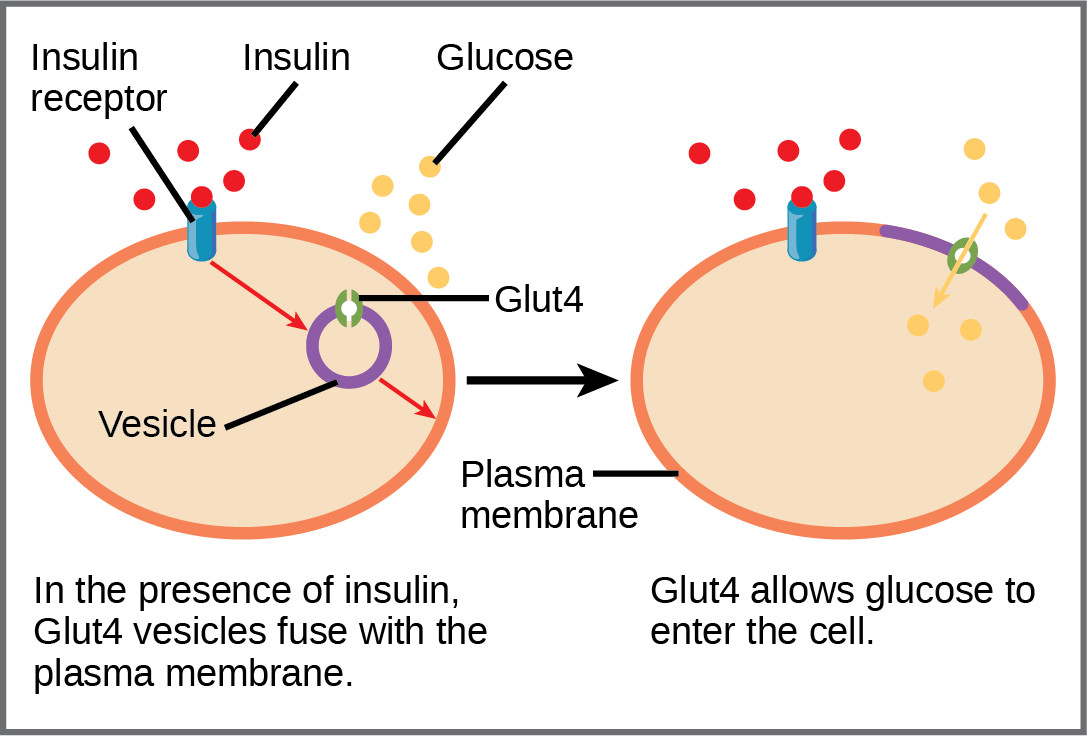
When insulin binds to its receptor on the cell surface, it triggers a cascade of intracellular signaling events.
This insulin signaling pathway ultimately leads to the translocation of GLUT4 transporters from intracellular vesicles to the cell membrane.
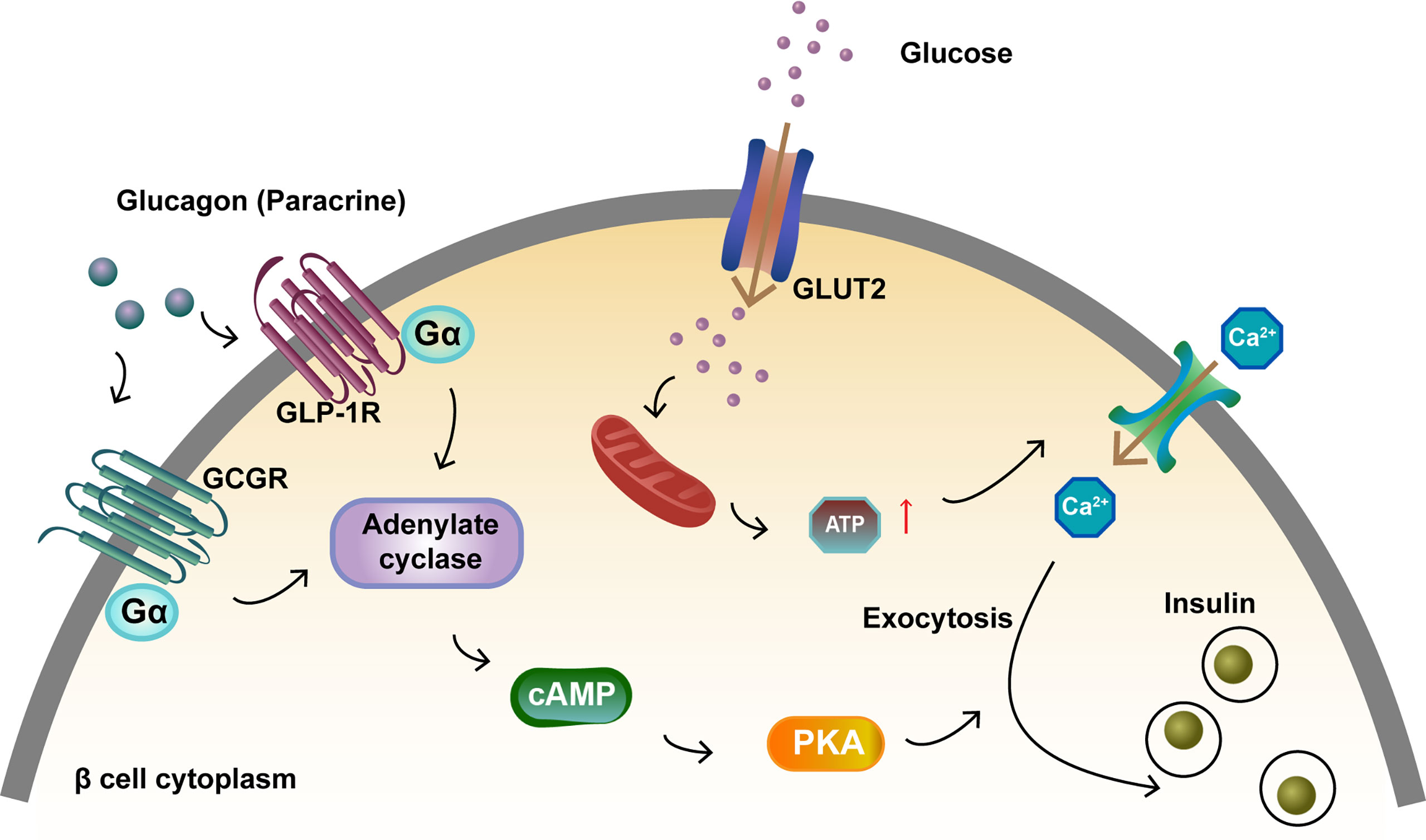
The Insulin Signaling Cascade
The insulin receptor is a tyrosine kinase, meaning it phosphorylates proteins upon activation.
Insulin binding causes the receptor to autophosphorylate, initiating a chain reaction.
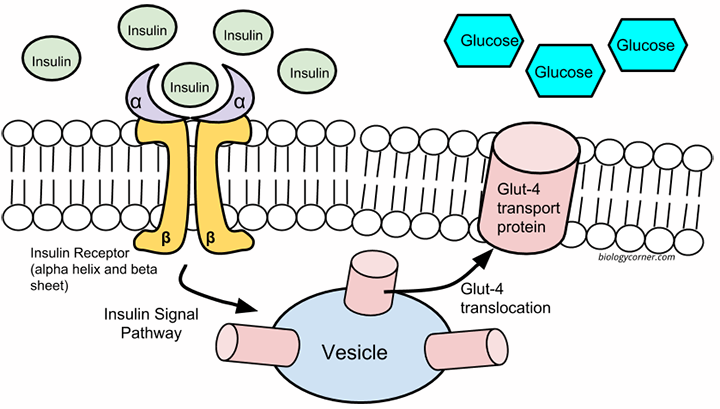
This phosphorylation cascade involves adaptor proteins like IRS (Insulin Receptor Substrate) and signaling molecules like PI3K (Phosphatidylinositol 3-Kinase) and Akt (also known as Protein Kinase B).
PI3K phosphorylates membrane lipids, creating docking sites for Akt.
Once activated, Akt phosphorylates a number of downstream targets, ultimately promoting GLUT4 translocation.
One key target is AS160 (Akt Substrate of 160 kDa), a protein that, when phosphorylated by Akt, releases its inhibitory effect on GLUT4 trafficking.
GLUT4 Translocation: Bringing Glucose Inside
The precise mechanisms by which GLUT4 vesicles move to and fuse with the plasma membrane are still being investigated, but several proteins are known to be involved.
These include SNARE proteins, which mediate membrane fusion events.
Once GLUT4 is inserted into the plasma membrane, it facilitates the transport of glucose into the cell down its concentration gradient.
Dysfunctional Signaling: Diabetes and Beyond
Disruptions in insulin signaling and GLUT4 translocation are hallmarks of type 2 diabetes.
Insulin resistance, a condition in which cells fail to respond properly to insulin, can arise from various factors, including genetic predisposition, obesity, and physical inactivity.
This resistance impairs GLUT4 translocation, leading to elevated blood glucose levels.
Furthermore, problems with other components of the signaling cascade, such as defects in the insulin receptor or downstream signaling molecules, can also contribute to impaired glucose uptake.
Beyond Insulin: Other Regulatory Pathways
While insulin is the primary regulator of GLUT4-mediated glucose uptake, other factors can also influence the process.
Muscle contraction, for example, stimulates glucose uptake independently of insulin, through pathways involving AMPK (AMP-activated protein kinase).
This explains why exercise is beneficial for improving glucose control, even in individuals with insulin resistance.
Other hormones and signaling molecules, such as adipokines (hormones secreted by fat tissue), can also modulate glucose uptake in various tissues.
The Future of Glucose Uptake Research
Ongoing research continues to unravel the complexities of glucose uptake and its regulation.
Scientists are exploring new therapeutic targets for improving insulin sensitivity and promoting GLUT4 translocation in individuals with diabetes.
Understanding the intricate details of cell signaling in glucose uptake holds immense potential for developing novel strategies to combat metabolic diseases and improve overall health.
“Further research is crucial to fully elucidate the intricate mechanisms governing glucose uptake,” says Dr. Emily Carter, a leading researcher in the field of metabolic signaling at the National Institutes of Health. “A comprehensive understanding will pave the way for targeted therapies to address insulin resistance and improve glucose homeostasis.”
By continuing to investigate the intricate processes of cell signaling and glucose uptake, scientists hope to develop new and effective strategies for preventing and treating diabetes and other related metabolic disorders, ultimately improving the health and well-being of millions worldwide.