Delivering Health Care In America: A Systems Approach

The American healthcare system, often described as a complex web of interconnected entities, is undergoing increased scrutiny as stakeholders grapple with rising costs, uneven access, and persistent health disparities. A systems-based approach, aiming to understand the interplay of various components and optimize overall performance, is gaining traction as a potential pathway to meaningful reform.
This article explores the concept of a systems approach to healthcare delivery in the United States, examining its potential benefits, challenges, and practical implications for patients, providers, and policymakers. The analysis draws from recent reports, expert opinions, and ongoing initiatives focused on improving the efficiency, equity, and effectiveness of the nation's healthcare infrastructure.
Understanding the Systems Approach
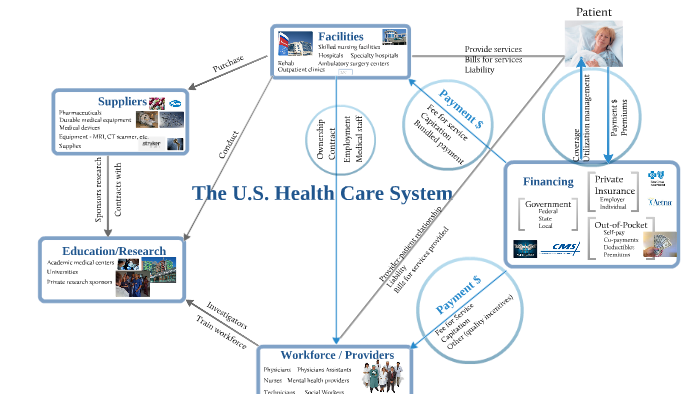
A systems approach views healthcare not as a collection of isolated transactions but as an integrated network of individuals, organizations, and resources. It emphasizes the interdependence of these elements and seeks to optimize the flow of information, resources, and patients across the system.
This holistic perspective acknowledges that changes in one area can have cascading effects elsewhere. Therefore, interventions must be carefully designed and implemented to avoid unintended consequences. The focus shifts from individual components to the overall system performance, measured by metrics like access, quality, cost, and patient satisfaction.
Key Components of a Healthcare System
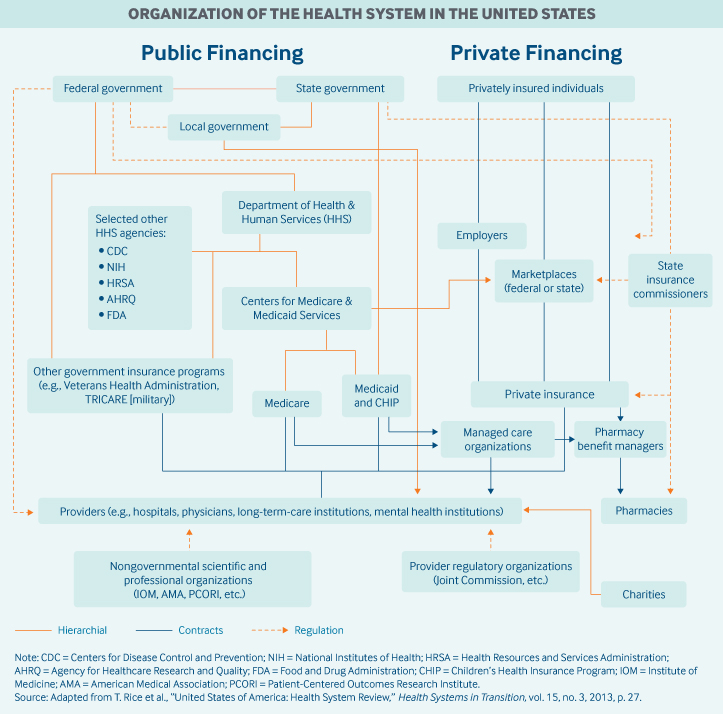
The American healthcare system comprises numerous interconnected components. This includes patients, providers (physicians, nurses, specialists), hospitals, clinics, insurance companies, pharmaceutical companies, regulatory agencies, and public health organizations.
Each component plays a specific role, and their interactions determine the overall performance of the system. A systems approach recognizes the importance of aligning incentives, fostering collaboration, and streamlining processes to improve the efficiency and effectiveness of these interactions. For example, coordinated care models, like Accountable Care Organizations (ACOs), seek to integrate providers across different settings to improve care coordination and reduce fragmentation.
Benefits of a Systems Perspective
Adopting a systems approach offers several potential benefits for healthcare delivery in the United States. By understanding the complex interactions within the system, policymakers and healthcare leaders can identify bottlenecks, inefficiencies, and areas for improvement.
One key benefit is the potential for improved care coordination. By fostering collaboration among providers and integrating different aspects of care, a systems approach can reduce duplication, minimize errors, and enhance the patient experience. For instance, electronic health records (EHRs) can facilitate the seamless sharing of information among providers, enabling more informed decision-making.
Furthermore, a systems approach can help address health disparities. By examining the social determinants of health – such as poverty, education, and access to healthy food – within the context of the broader healthcare system, interventions can be tailored to meet the specific needs of vulnerable populations.
Improved efficiency and cost containment are also potential outcomes. By identifying and eliminating waste, streamlining processes, and promoting preventive care, a systems approach can help reduce healthcare spending without compromising quality. This can be achieved through initiatives such as value-based care models, which incentivize providers to deliver high-quality, cost-effective care.
Challenges to Implementation
Despite its potential benefits, implementing a systems approach to healthcare delivery faces significant challenges. The sheer complexity of the American healthcare system, with its diverse stakeholders and competing interests, makes it difficult to implement comprehensive reforms.
One major obstacle is the lack of data interoperability. Many healthcare providers still rely on outdated systems that are not compatible with each other, hindering the seamless exchange of information. Addressing this requires significant investments in technology infrastructure and the adoption of standardized data formats.
Another challenge is the fragmented payment system. Fee-for-service models, which reward providers for the volume of services rather than the value they deliver, can create disincentives for coordination and prevention. Shifting towards value-based payment models requires a fundamental change in the way healthcare is financed.
Resistance to change from various stakeholders can also impede progress. Providers, insurers, and pharmaceutical companies may be reluctant to embrace reforms that could impact their bottom lines. Overcoming this resistance requires strong leadership, effective communication, and a clear articulation of the benefits of a systems approach.
Examples of Systems-Based Initiatives
Several initiatives across the United States are already incorporating elements of a systems approach to healthcare delivery. These include ACOs, patient-centered medical homes (PCMHs), and state-level health information exchanges (HIEs).
ACOs are groups of doctors, hospitals, and other healthcare providers who voluntarily come together to provide coordinated, high-quality care to their Medicare patients. The goal of an ACO is to deliver seamless, coordinated care, ultimately improving the quality and efficiency of healthcare.
PCMHs focus on providing comprehensive, coordinated, and patient-centered care. They emphasize a team-based approach, with a primary care physician serving as the central point of contact for all of the patient's healthcare needs.
HIEs facilitate the electronic exchange of health information among providers, enabling them to access a more complete picture of a patient's medical history. This can improve care coordination, reduce medical errors, and enhance patient safety.
Moving Forward
Delivering healthcare in America through a systems approach requires a fundamental shift in mindset, embracing collaboration, data-driven decision-making, and a focus on patient-centered care. While the challenges are significant, the potential benefits for improving access, quality, and affordability are substantial. Stakeholders must work together to overcome obstacles and create a more integrated and effective healthcare system. This includes investing in infrastructure, reforming payment models, and fostering a culture of continuous improvement.
The ultimate goal is to create a healthcare system that is not only efficient and cost-effective but also equitable and responsive to the needs of all Americans. Achieving this vision requires a sustained commitment to systems thinking and a willingness to embrace innovation and change. The health and well-being of the nation depend on it.




![Delivering Health Care In America: A Systems Approach [PDF] Delivering Health Care in America: A Systems Approach full](https://www.yumpu.com/en/image/facebook/63468672.jpg)
![Delivering Health Care In America: A Systems Approach [DOWNLOAD] Delivering Health Care in America: A Systems Approach full free](https://www.yumpu.com/en/image/facebook/66499298.jpg)