Erythema Multiforme And Stevens Johnson Syndrome

A rare but serious spectrum of skin and mucous membrane disorders, ranging from Erythema Multiforme (EM) to Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN), continues to pose diagnostic and therapeutic challenges for healthcare professionals worldwide. Understanding the nuances of these conditions is crucial for prompt identification and effective management.
This article provides an overview of EM and SJS/TEN, exploring their causes, symptoms, diagnosis, and treatment options. It also highlights the importance of early detection and the potential long-term effects these conditions can have on affected individuals.
Understanding the Spectrum
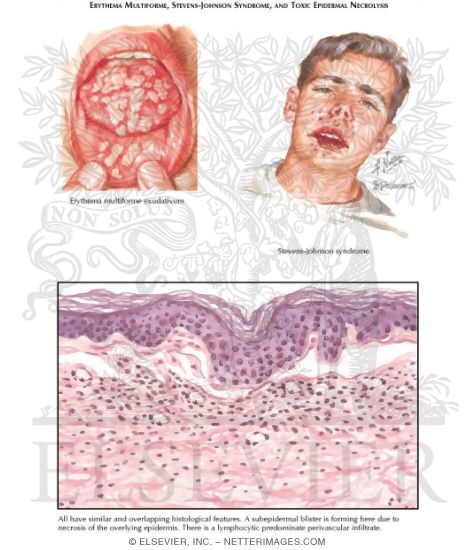
Erythema Multiforme, SJS, and TEN are considered a spectrum of reactions, with EM being the mildest form and TEN the most severe. The primary difference lies in the extent of skin detachment.
In EM, less than 10% of the body surface area (BSA) is affected. SJS involves 1-10% BSA detachment, while TEN involves more than 30%. SJS/TEN overlap refers to cases with 10-30% BSA detachment.
Causes and Risk Factors
The most common cause of Erythema Multiforme is infection, particularly the herpes simplex virus (HSV). Medications are less frequently implicated in EM compared to SJS/TEN.
SJS and TEN are most commonly triggered by medications. According to the National Institutes of Health (NIH), drugs known to increase the risk include certain antibiotics (e.g., sulfonamides), anticonvulsants (e.g., lamotrigine, phenytoin), and nonsteroidal anti-inflammatory drugs (NSAIDs).
Certain populations may be at higher risk. Individuals with compromised immune systems, such as those with HIV infection or autoimmune diseases, might be more susceptible. Genetic factors can also play a role, particularly with certain drug-induced reactions.
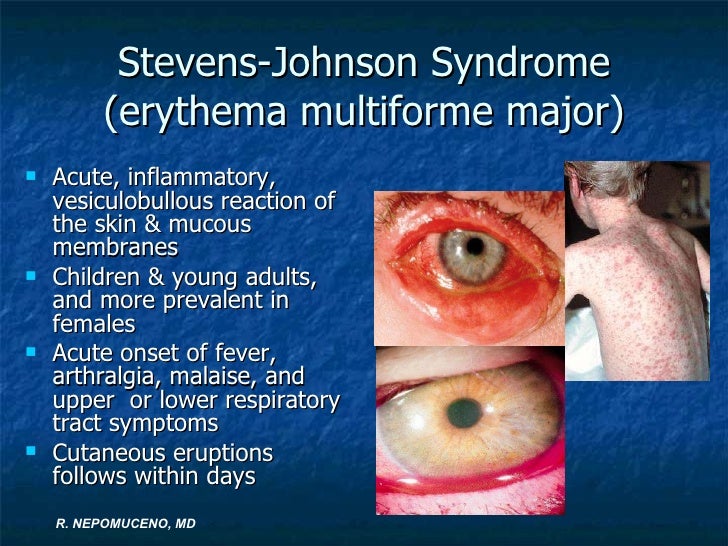
Signs and Symptoms
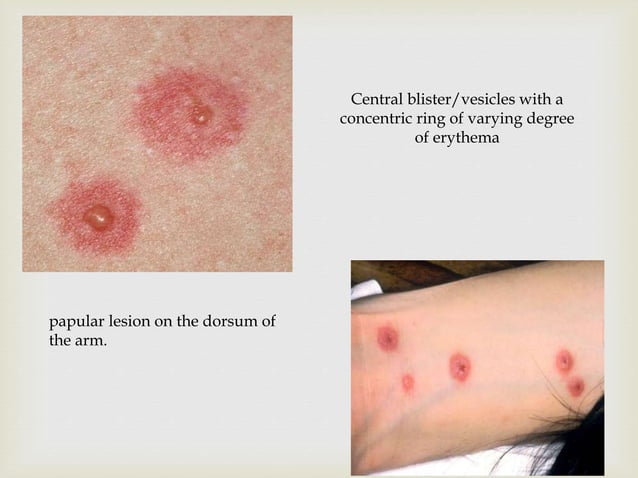
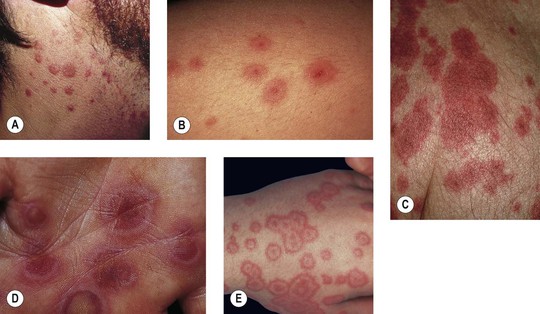
Erythema Multiforme typically presents with target-like lesions on the skin. These lesions are often symmetrical and can appear on the extremities, face, and trunk. Itching is a common symptom.
SJS/TEN manifests with flu-like symptoms, such as fever, sore throat, and fatigue, followed by a widespread rash. The rash progresses to blisters and skin detachment, leading to raw, exposed areas similar to burns. Mucous membrane involvement, including the mouth, eyes, and genitals, is a hallmark of SJS/TEN.
Complications of SJS/TEN can be severe and life-threatening. These include skin infections, sepsis, dehydration, electrolyte imbalances, and respiratory distress. Long-term complications may involve scarring, pigmentation changes, and eye problems.
Diagnosis and Treatment
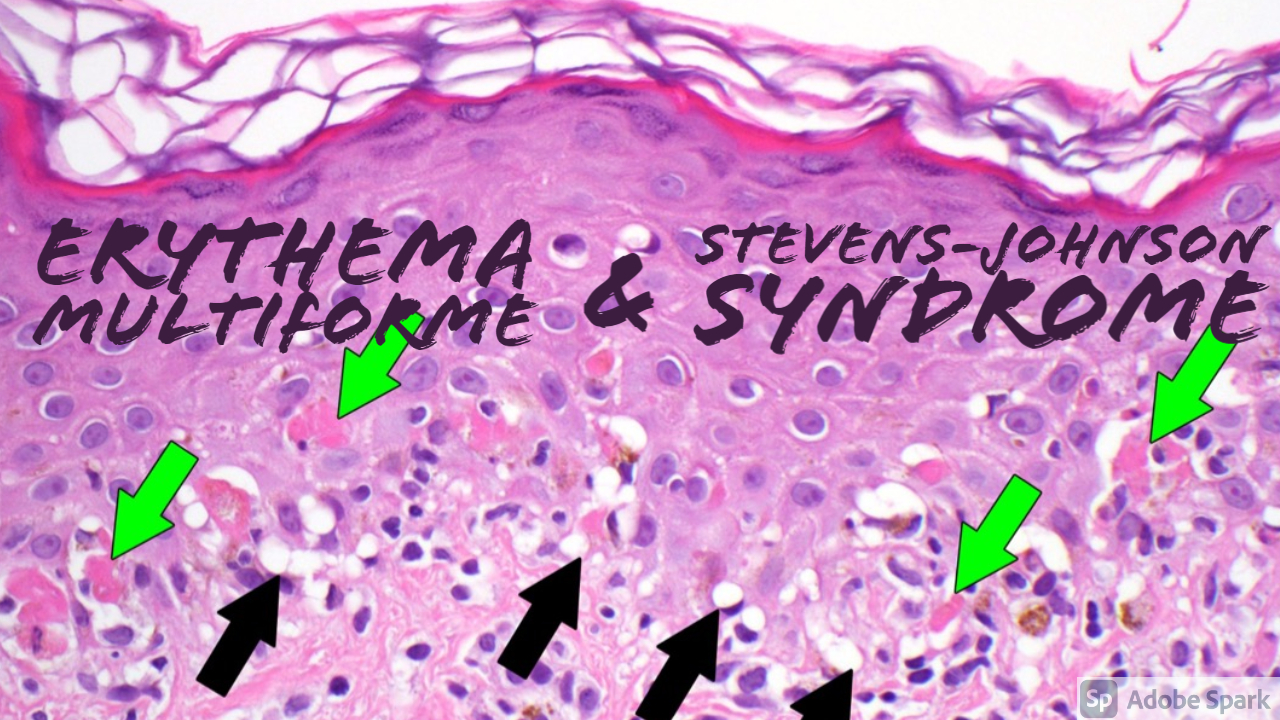
Diagnosis is primarily based on clinical presentation and a thorough medical history, including medication use. A skin biopsy may be performed to confirm the diagnosis and rule out other conditions.
Treatment focuses on stopping the offending medication (if applicable), providing supportive care, and managing complications. This often requires hospitalization, ideally in a burn unit or specialized dermatology unit.
Supportive care includes fluid and electrolyte replacement, pain management, wound care, and infection control. Immunosuppressive therapies, such as corticosteroids or intravenous immunoglobulin (IVIG), may be considered in some cases, although their efficacy remains a subject of ongoing research.
The Importance of Early Detection
Early detection and prompt treatment are crucial for improving outcomes and minimizing the risk of complications. Patients who experience a suspicious rash, especially if accompanied by fever or mucous membrane involvement, should seek immediate medical attention.
Healthcare providers should maintain a high index of suspicion for SJS/TEN, particularly in patients taking medications known to be associated with these reactions. Careful medication history and awareness of potential drug interactions are essential.
Public Health Implications
While rare, SJS/TEN represents a significant public health concern due to its severity and potential for long-term morbidity. Increased awareness among healthcare professionals and the public is vital for early recognition and appropriate management.
Reporting suspected drug-induced cases to regulatory agencies, such as the Food and Drug Administration (FDA), is essential for identifying and mitigating potential risks associated with medications.
Further research is needed to better understand the underlying mechanisms of these conditions and to develop more effective treatment strategies. This includes identifying genetic markers that may predict susceptibility to drug-induced SJS/TEN.
The emotional toll of SJS/TEN on patients and their families can be significant. Support groups and counseling services can provide valuable assistance in coping with the physical and psychological challenges associated with these conditions.
The SJS Foundation, for example, offers resources and support for individuals affected by SJS/TEN and their caregivers. These resources include information about the condition, coping strategies, and opportunities to connect with others who have similar experiences.
Erythema Multiforme and Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis, while rare, underscore the importance of vigilance regarding potential adverse drug reactions and the need for prompt medical attention when suspicious symptoms arise. Continued research, education, and awareness are essential to improve outcomes and support those affected by these challenging conditions.




![Erythema Multiforme And Stevens Johnson Syndrome [PDF] Case of Erythema Multiforme/Stevens–Johnson Syndrome: An Unusual](https://d3i71xaburhd42.cloudfront.net/a4d05c94ec2adc38a9896d6e8ed9f1ac6c84dd66/2-Figure3-1.png)