Fluid And Electrolyte Imbalance Nursing Diagnosis

In the hushed corridors of hospitals and clinics, an unseen battle is waged daily: the fight against fluid and electrolyte imbalance. This silent disruptor, often overshadowed by more visible ailments, can swiftly turn critical, pushing patients from a state of delicate equilibrium into life-threatening crisis.
From subtle fatigue to cardiac arrest, the consequences of disrupted hydration and electrolyte levels underscore the urgency of precise diagnosis and prompt intervention. Ignoring this subtle condition is not an option.
Understanding the Fluid and Electrolyte Imbalance Nursing Diagnosis
The fluid and electrolyte imbalance nursing diagnosis signifies a state where the body's fluid volume or electrolyte concentrations deviate from normal ranges, jeopardizing physiological functions. This condition isn't a disease in itself, but rather a consequence of underlying medical conditions, treatments, or lifestyle factors.
It is critical for nurses to accurately identify and address these imbalances to prevent severe complications.
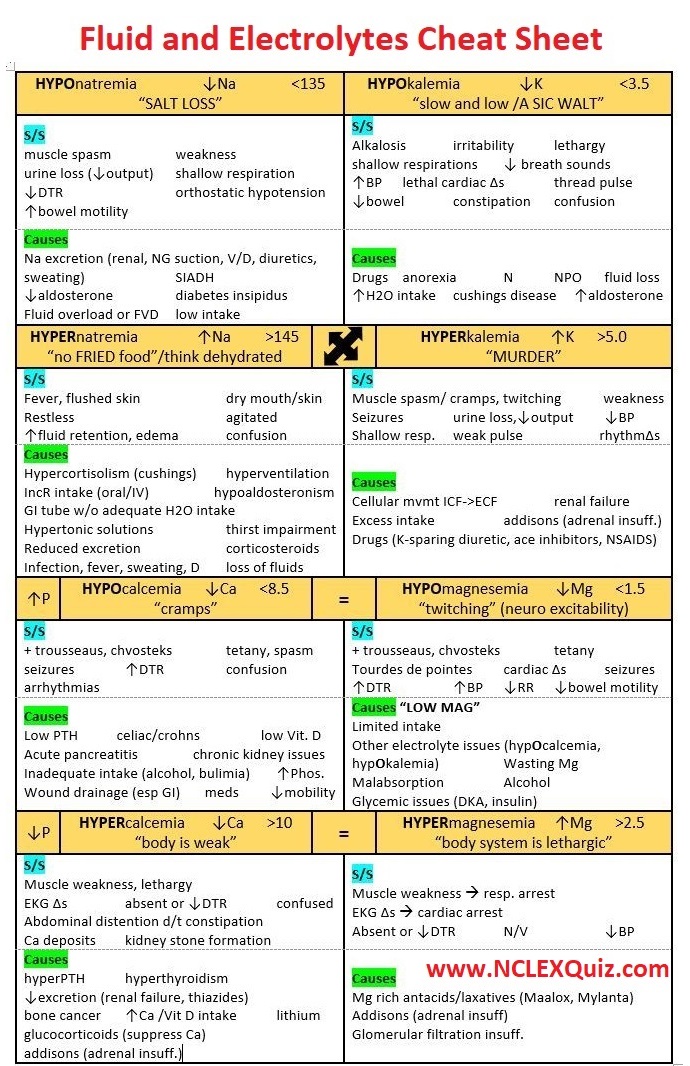
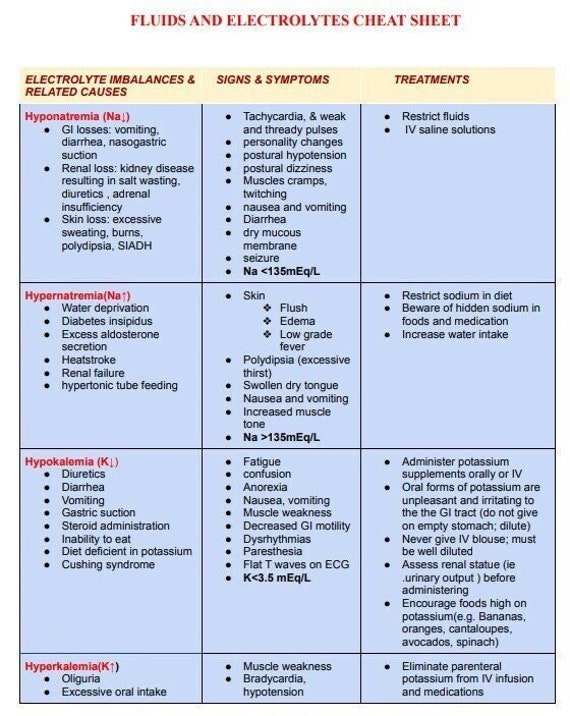
At its core, this diagnosis encompasses several specific imbalances, including:
- Fluid Volume Deficit (Hypovolemia): A decrease in intravascular, interstitial, and/or intracellular fluid.
- Fluid Volume Excess (Hypervolemia): An increase in fluid retention and edema.
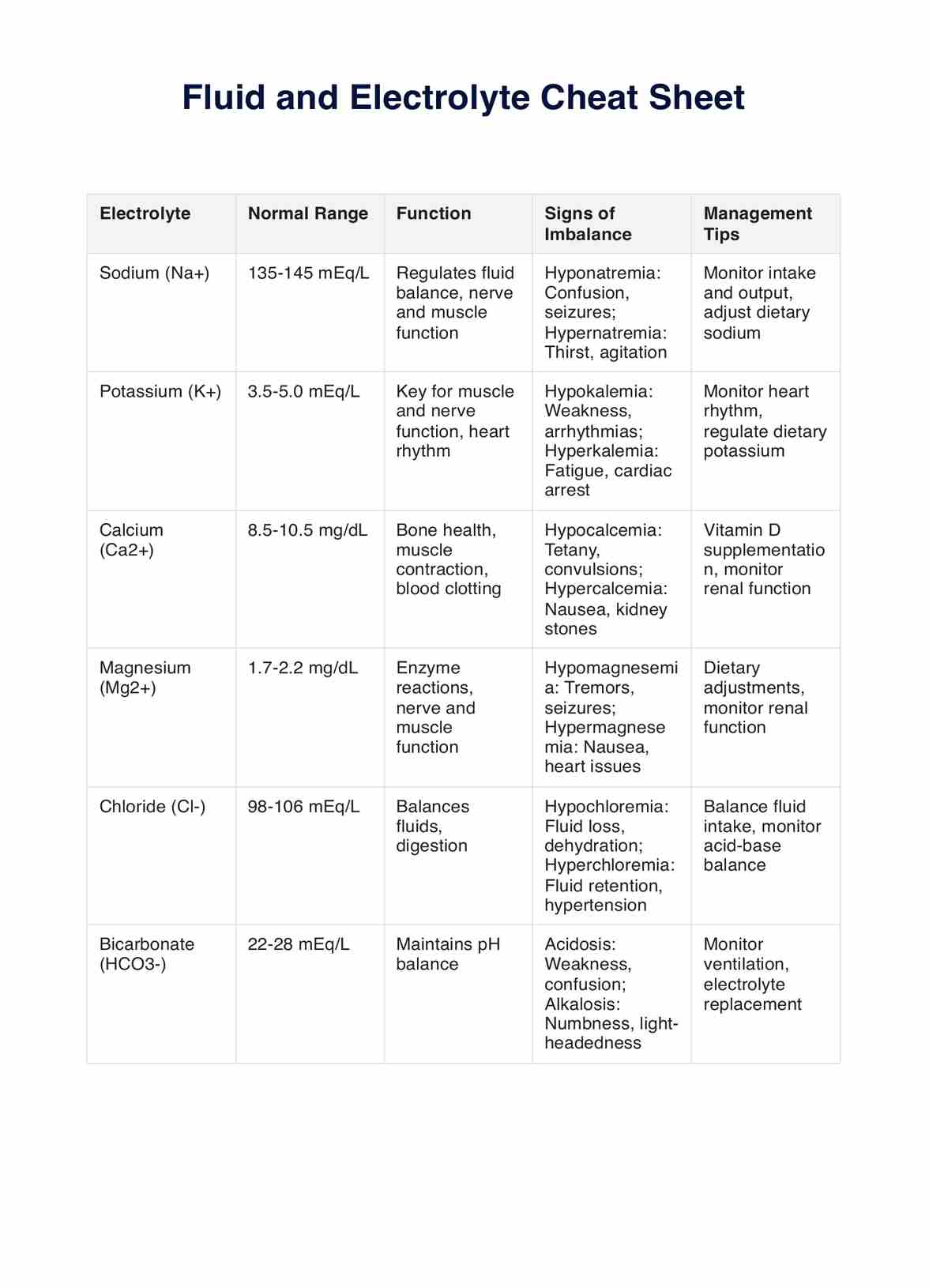
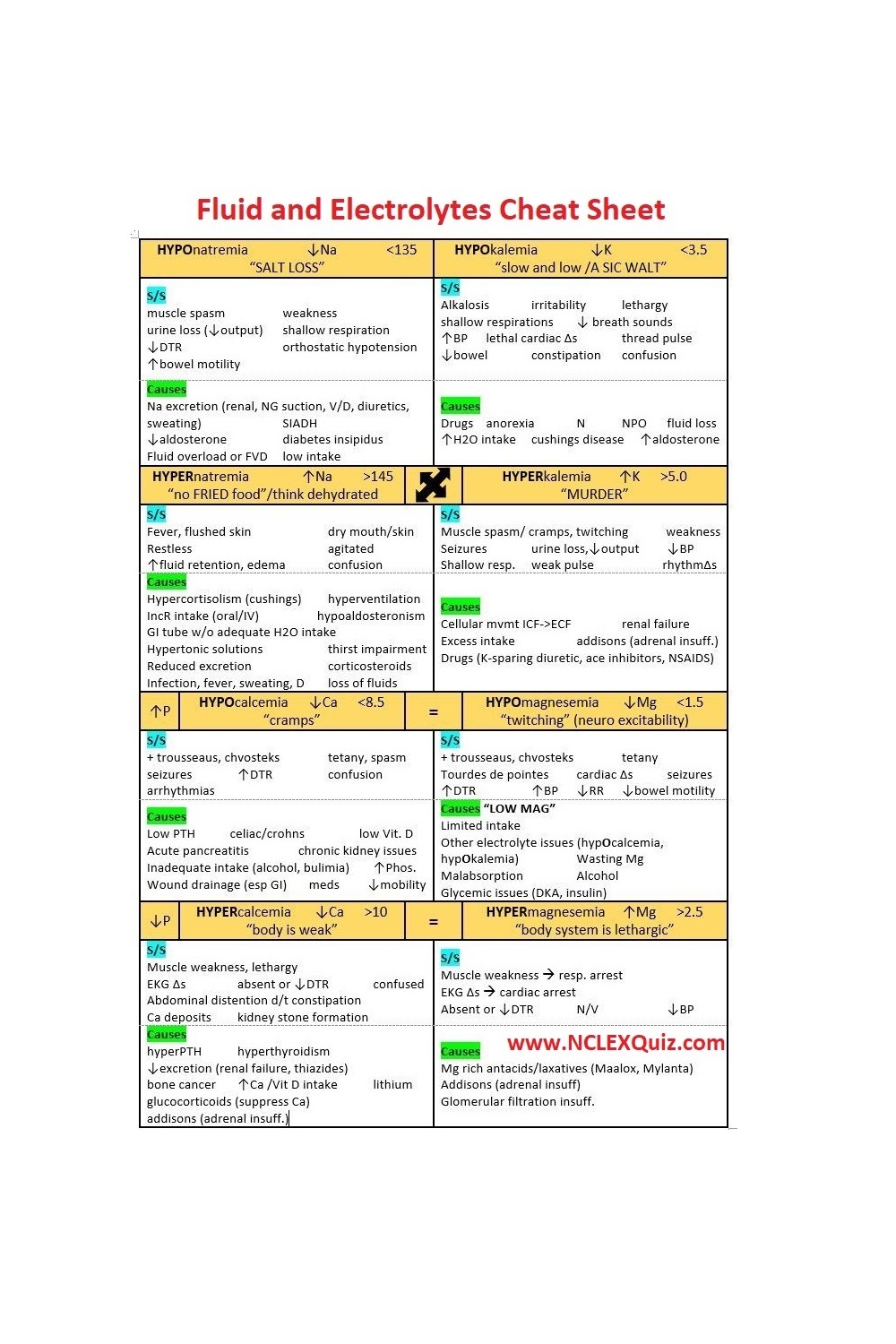
- Electrolyte Imbalances: Disruptions in the serum levels of electrolytes such as sodium, potassium, calcium, and magnesium.
Each of these imbalances manifests differently and requires tailored interventions.
Causes and Risk Factors
A multitude of factors can trigger fluid and electrolyte imbalances, making accurate diagnosis a complex puzzle. Healthcare providers must be attentive.
Underlying medical conditions play a significant role. For example, renal failure directly impairs the body's ability to regulate fluid and electrolyte excretion.
Likewise, heart failure can lead to fluid overload due to compromised cardiac output and subsequent activation of compensatory mechanisms.
Certain medications, notably diuretics, can inadvertently deplete electrolytes, especially potassium and sodium. Vomiting and diarrhea are common culprits, leading to rapid fluid and electrolyte losses.
Severe burns damage the skin's protective barrier, causing significant fluid shifts. It’s crucial to be vigilant.
Age is also a major risk factor. Infants and young children are more susceptible to dehydration due to their higher metabolic rates and immature kidneys. Elderly individuals often experience reduced thirst sensation and decreased kidney function, increasing their vulnerability.
Signs and Symptoms: Recognizing the Imbalance
Early recognition of fluid and electrolyte imbalances hinges on careful assessment of clinical signs and symptoms. These can vary widely depending on the specific imbalance and its severity.
Fluid Volume Deficit
Common indicators of dehydration include:
- Thirst
- Dry mucous membranes
- Decreased urine output
- Rapid heart rate
- Low blood pressure
- Dizziness
Fluid Volume Excess
Conversely, fluid overload may present with:
- Edema (swelling) in the extremities
- Weight gain
- Shortness of breath
- Increased blood pressure
- Jugular vein distention
Electrolyte Imbalances
Electrolyte imbalances can manifest in a variety of ways, including:
- Sodium Imbalances: Confusion, seizures, muscle weakness.
- Potassium Imbalances: Cardiac arrhythmias, muscle cramps, fatigue.
- Calcium Imbalances: Muscle spasms, numbness, tingling.
- Magnesium Imbalances: Tremors, seizures, cardiac arrhythmias.
The severity and specific presentation of symptoms necessitate meticulous monitoring and targeted laboratory investigations.
Diagnostic Tools and Laboratory Findings
While clinical assessment provides initial clues, definitive diagnosis relies on laboratory investigations. Blood tests are paramount in assessing electrolyte levels, renal function, and acid-base balance.
Serum electrolyte panels reveal the concentrations of sodium, potassium, chloride, bicarbonate, calcium, and magnesium. Renal function tests, such as blood urea nitrogen (BUN) and creatinine, offer insights into kidney function and hydration status.
Urine analysis can also provide valuable information. Measuring urine specific gravity helps assess the concentration of urine, indicating the body's hydration status.
Urine electrolyte levels can assist in identifying the underlying cause of electrolyte imbalances. In some cases, electrocardiograms (ECGs) are used to detect cardiac abnormalities associated with electrolyte disturbances, particularly potassium and calcium imbalances.
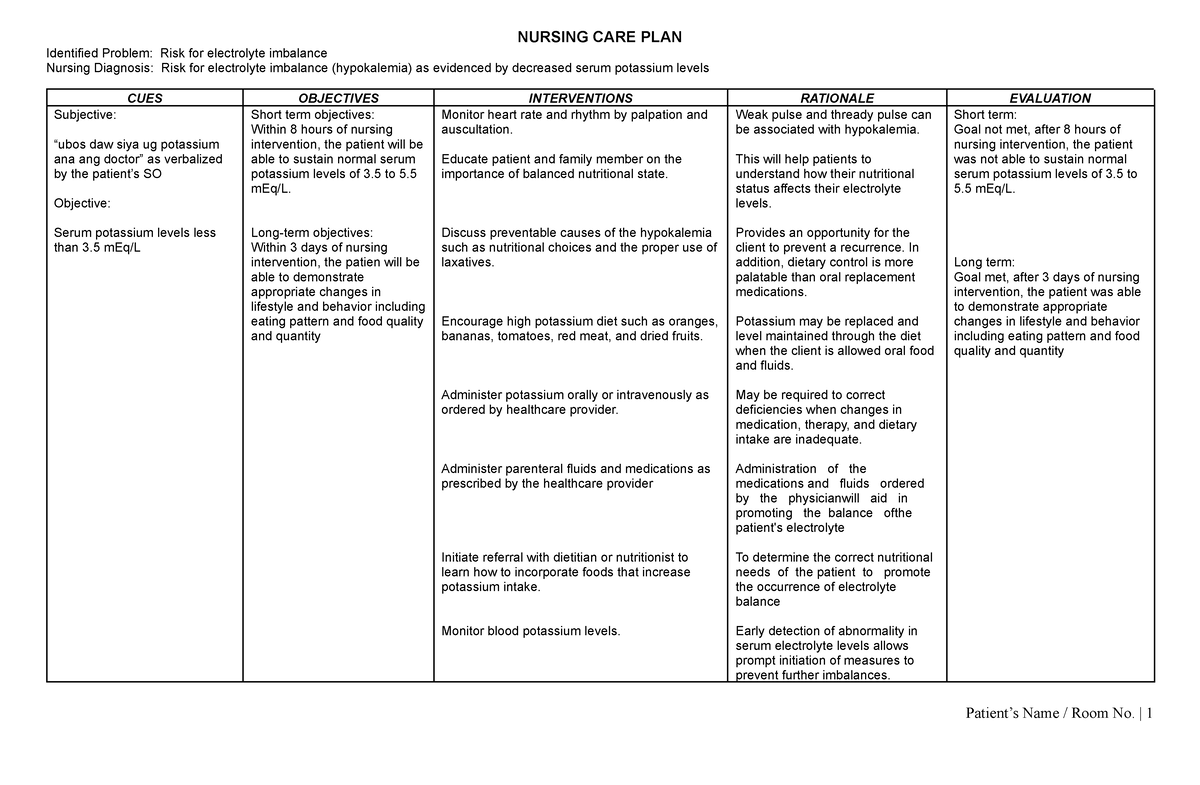
Nursing Interventions and Management
Effective management of fluid and electrolyte imbalances involves a multifaceted approach encompassing:
- Fluid replacement therapy
- Electrolyte replacement
- Dietary modifications
- Medication management
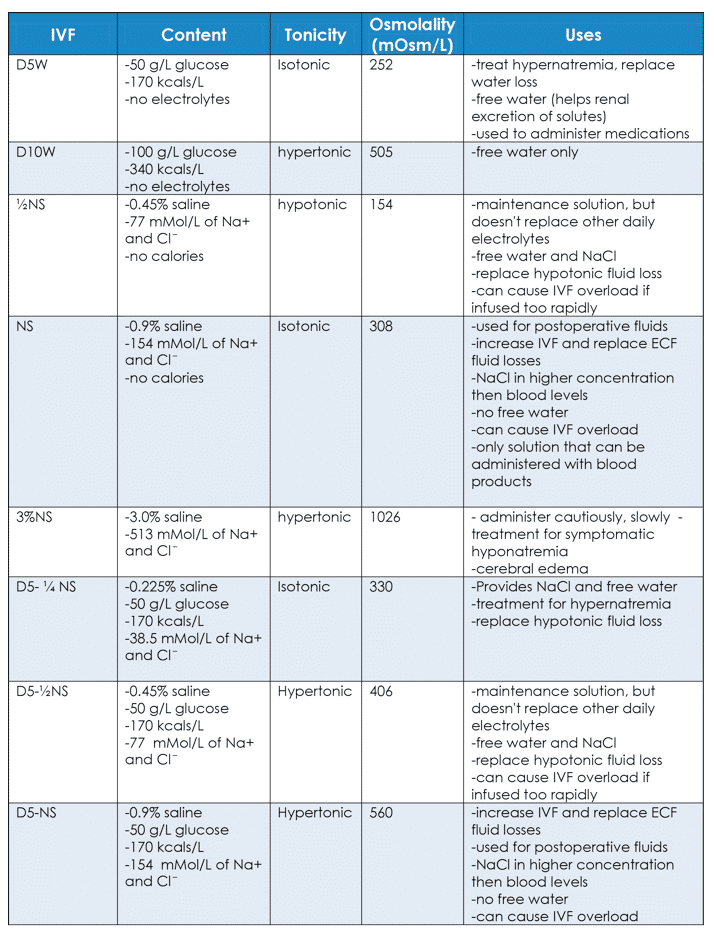
Fluid replacement is crucial for correcting dehydration, typically achieved through oral or intravenous administration of fluids. The type and rate of fluid administration depend on the severity of dehydration and the patient's underlying medical conditions.
Electrolyte imbalances are addressed through targeted replacement strategies. Potassium, sodium, calcium, or magnesium may be administered orally or intravenously, depending on the specific deficiency and the patient's tolerance.
Dietary modifications play a supportive role in maintaining electrolyte balance. Encouraging patients to consume potassium-rich foods, such as bananas and oranges, can help prevent hypokalemia. Limiting sodium intake can assist in managing fluid overload.
Careful medication management is essential to avoid drug-induced imbalances. Diuretics must be used judiciously and with close monitoring of electrolyte levels. Certain medications, such as ACE inhibitors, can affect potassium levels, requiring careful attention.
Prevention Strategies
Preventing fluid and electrolyte imbalances is often more effective than treating them. Education is key.
Individuals at risk, such as the elderly and those with chronic conditions, should be educated about the importance of adequate fluid intake, especially during hot weather or periods of increased physical activity. Monitoring fluid balance by tracking daily weight and urine output can help detect early signs of imbalance.
Dietary modifications can also play a preventative role. Consuming a balanced diet rich in electrolytes can help maintain normal electrolyte levels. Individuals taking diuretics should be educated about potential electrolyte losses and the importance of potassium-rich foods.
Regular monitoring of electrolyte levels is crucial for individuals at high risk, such as those with kidney disease or heart failure. Early detection and intervention can prevent severe complications.
The Future of Fluid and Electrolyte Management
Advancements in technology and research are shaping the future of fluid and electrolyte management. Continuous monitoring devices are being developed to provide real-time assessment of fluid and electrolyte status, allowing for more timely interventions.
Personalized medicine approaches are tailoring fluid and electrolyte management strategies to individual patient needs, taking into account genetic factors, medical history, and lifestyle.
Furthermore, ongoing research is exploring novel therapies for preventing and treating fluid and electrolyte imbalances, such as targeted electrolyte replacement and innovative fluid management strategies.
By embracing these advancements and fostering a culture of vigilance, healthcare professionals can continue to improve patient outcomes and minimize the risks associated with these critical imbalances. The key is always prevention, close monitoring and the right diagnosis.