How Does Opioids Cause Respiratory Depression
Imagine a calm evening, a loved one settling down for a restful night after a long day. But as silence descends, their breathing becomes shallow, almost imperceptible. A wave of panic washes over you as you realize something is terribly wrong. This is the terrifying reality of opioid-induced respiratory depression, a silent threat lurking beneath the surface of pain relief.
At the heart of this critical issue lies a fundamental question: How exactly do opioids, powerful medications designed to alleviate pain, trigger such a life-threatening suppression of breathing? Understanding the intricate mechanisms behind this phenomenon is crucial for both those who prescribe and those who use these medications, as well as for the families and communities affected by the opioid crisis.
Opioids have been used for centuries for their analgesic properties. They are derived from opium or synthetically produced to mimic the effects of natural opiates. Drugs like morphine, codeine, oxycodone, and fentanyl fall into this category, each with varying degrees of potency and efficacy.
The foundation of their pain-relieving ability lies in their interaction with specific receptors in the brain and spinal cord known as opioid receptors. These receptors, including mu (μ), delta (δ), and kappa (κ) receptors, are part of the body's natural pain management system.
When an opioid binds to these receptors, it initiates a cascade of events that ultimately reduce the perception of pain. This occurs by blocking pain signals from reaching the brain and by releasing dopamine, a neurotransmitter associated with pleasure and reward.
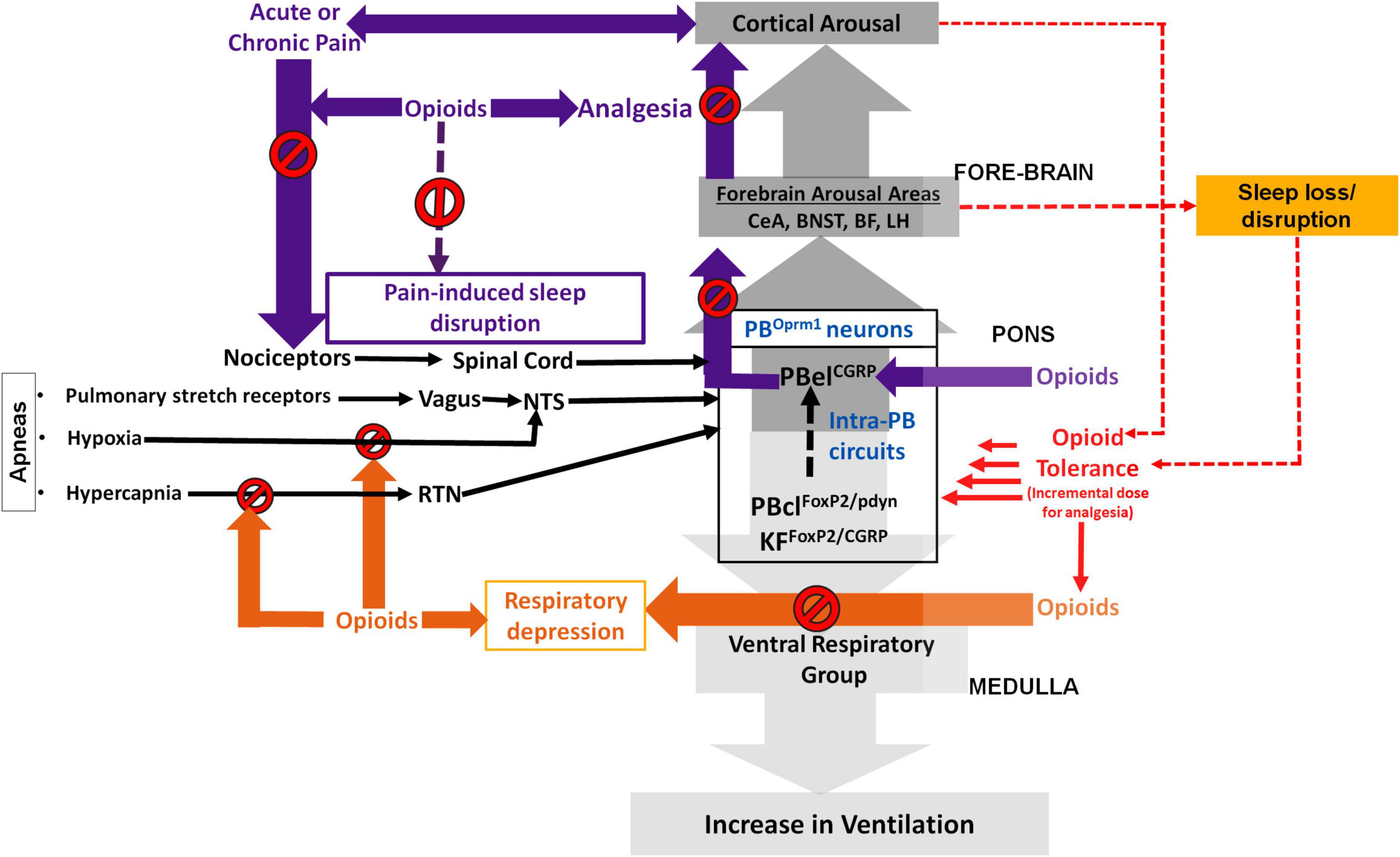
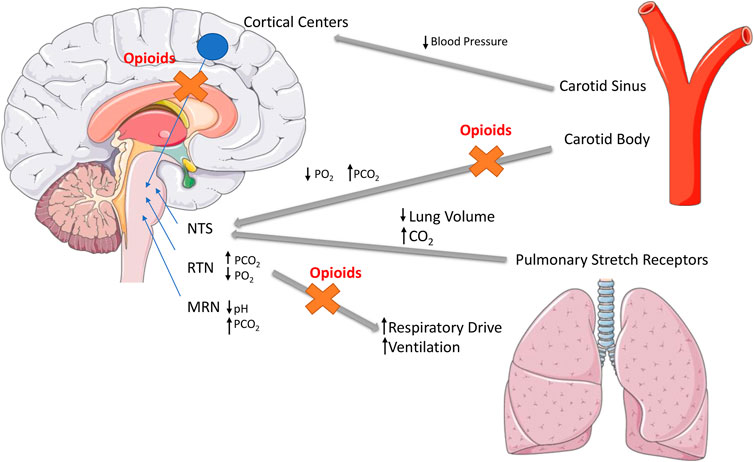
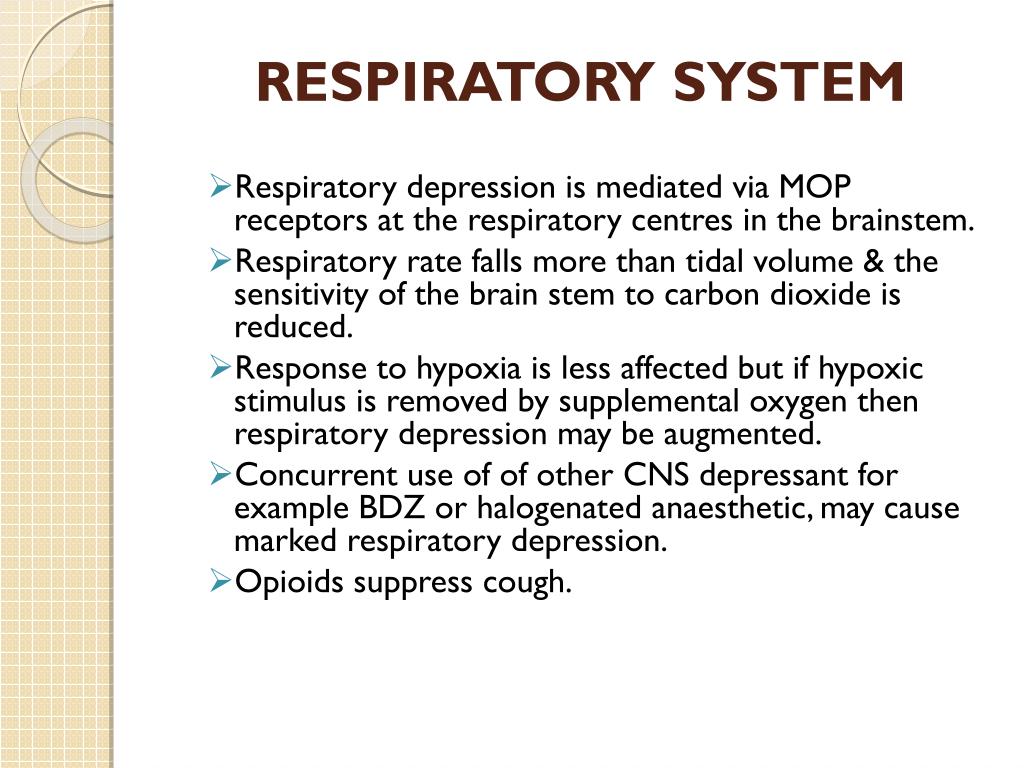
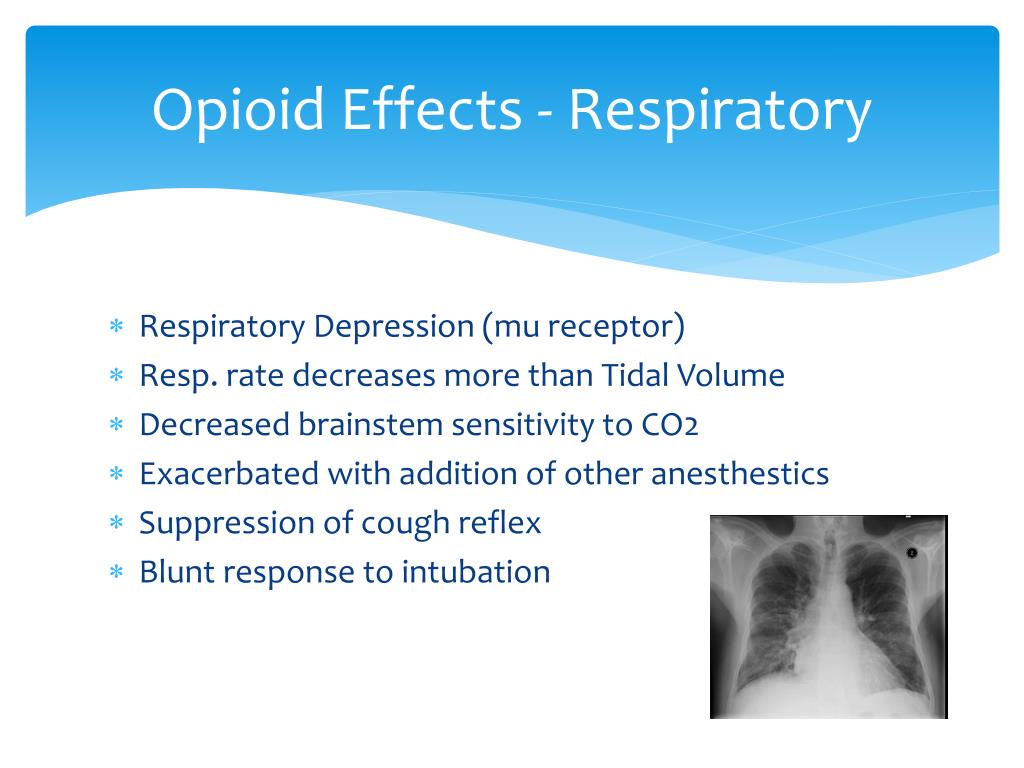
However, these same receptors are also found in brain regions that control breathing, particularly in the brainstem's respiratory center. This area is responsible for regulating the rate and depth of our breaths, ensuring a constant supply of oxygen to the body.
Respiratory depression occurs when opioids bind to the mu receptors in the brainstem, disrupting the normal function of the respiratory center. This disruption leads to a decrease in the rate and depth of breathing, reducing the amount of oxygen entering the body and increasing the buildup of carbon dioxide.
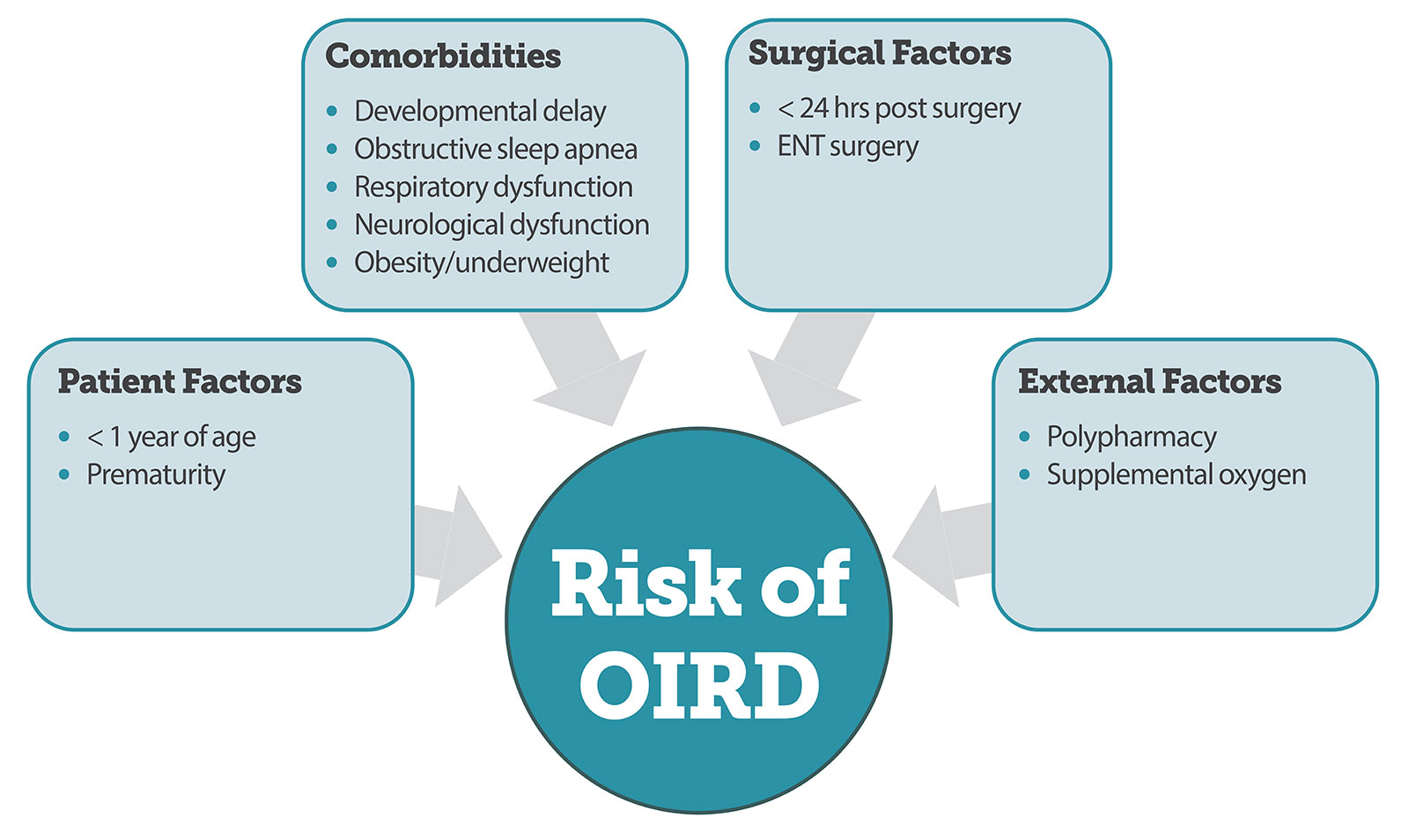
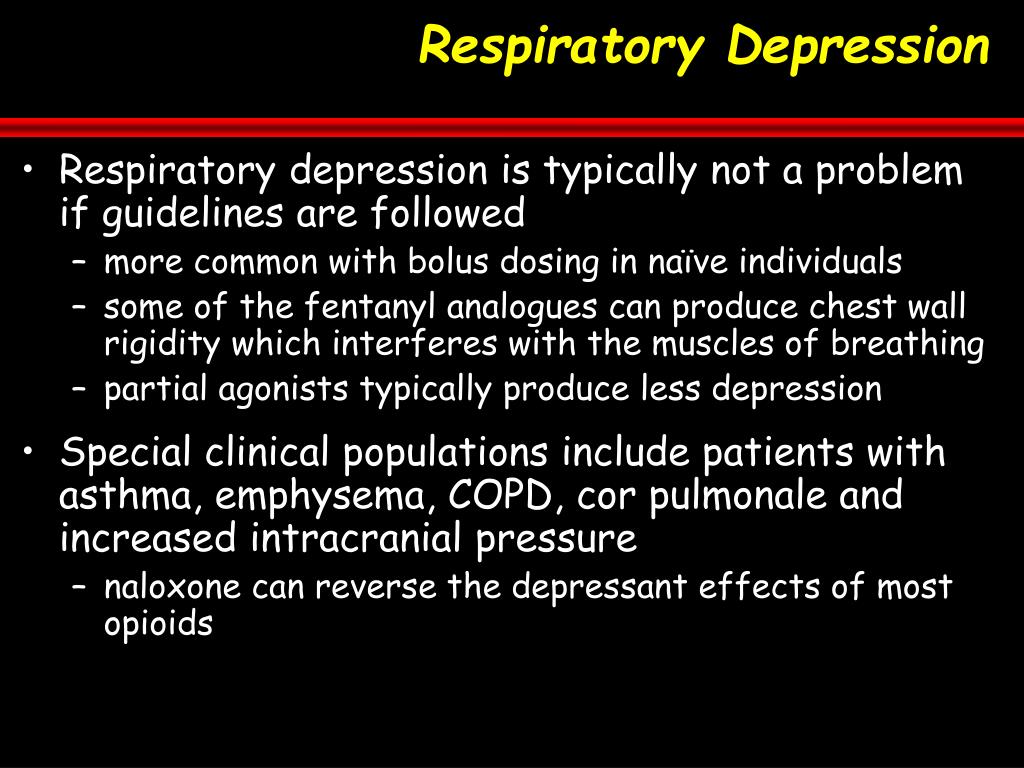
The degree of respiratory depression depends on several factors, including the type of opioid, the dosage, and the individual's sensitivity to the drug. Higher doses of more potent opioids, like fentanyl, are more likely to cause significant respiratory depression.
Individuals with pre-existing respiratory conditions, such as chronic obstructive pulmonary disease (COPD) or sleep apnea, are at higher risk. Similarly, those who are elderly, frail, or have impaired kidney or liver function are more susceptible due to reduced ability to process and eliminate the drug from their system.
Concurrent use of other central nervous system depressants, such as alcohol or benzodiazepines, significantly increases the risk of respiratory depression. These substances amplify the effects of opioids, further suppressing the respiratory center.
Recognizing the signs of opioid-induced respiratory depression is crucial for timely intervention. These signs include slow or shallow breathing, pinpoint pupils, confusion, drowsiness, and unresponsiveness.
In severe cases, respiratory depression can lead to hypoxia (lack of oxygen), brain damage, and ultimately death. It's a grim reminder of the potent effects these medications have on the central nervous system.
Fortunately, there is a life-saving antidote: naloxone. This medication rapidly reverses the effects of opioids by blocking them from binding to the receptors. It can be administered via injection or nasal spray and can restore normal breathing within minutes.
Naloxone is now widely available to first responders, healthcare professionals, and even the general public. Increased accessibility to naloxone has undoubtedly saved countless lives and is a critical component of harm reduction strategies.
Prevention, however, remains the most effective strategy. This begins with responsible prescribing practices, ensuring that opioids are only used when necessary and at the lowest effective dose. Education plays a vital role, both for patients and prescribers.
Patients need to be fully informed about the risks associated with opioids, including the potential for respiratory depression and the importance of adhering to prescribed dosages. They should also be educated on how to recognize the signs of overdose and how to administer naloxone.
Prescribers need to carefully evaluate patients for risk factors, such as pre-existing respiratory conditions or concurrent use of other central nervous system depressants. They should also consider alternative pain management strategies, such as physical therapy, acupuncture, or non-opioid medications.
Efforts to combat the opioid crisis extend beyond medical interventions. Addressing the underlying factors that contribute to opioid use, such as poverty, mental health issues, and lack of access to healthcare, is essential.
Effective treatment for opioid use disorder, including medication-assisted treatment (MAT) with medications like buprenorphine or methadone, can significantly reduce the risk of overdose and respiratory depression. These medications help manage withdrawal symptoms and cravings, allowing individuals to focus on recovery.
The opioid crisis is a complex and multifaceted problem, but understanding the mechanisms behind opioid-induced respiratory depression is a vital piece of the puzzle. By raising awareness, promoting responsible prescribing practices, and ensuring access to naloxone and treatment, we can prevent future tragedies and save lives.
As we move forward, a collaborative effort involving healthcare professionals, policymakers, and community members is crucial. It's about fostering a culture of compassion, understanding, and evidence-based solutions to address this pervasive public health challenge. The key is to transform the narrative, emphasizing hope and healing while acknowledging the gravity of the situation. We all have a part to play in creating a safer and healthier future.