How Often Does Barrett's Esophagus Turn To Cancer

The diagnosis of Barrett's esophagus can be a chilling moment, a stark reminder of the body's fragility. For many, the immediate question that follows is fraught with anxiety: How likely is this to become cancer? This fear is understandable, as the condition is a known precursor to esophageal adenocarcinoma, a particularly aggressive form of cancer.
While the connection is undeniable, the actual risk of progression is far more nuanced than most realize. This article delves into the true rate of malignant transformation, examines the factors influencing that risk, and explores what individuals diagnosed with Barrett's esophagus can do to manage their condition and minimize their chances of developing cancer.
Understanding Barrett's Esophagus and its Cancer Risk
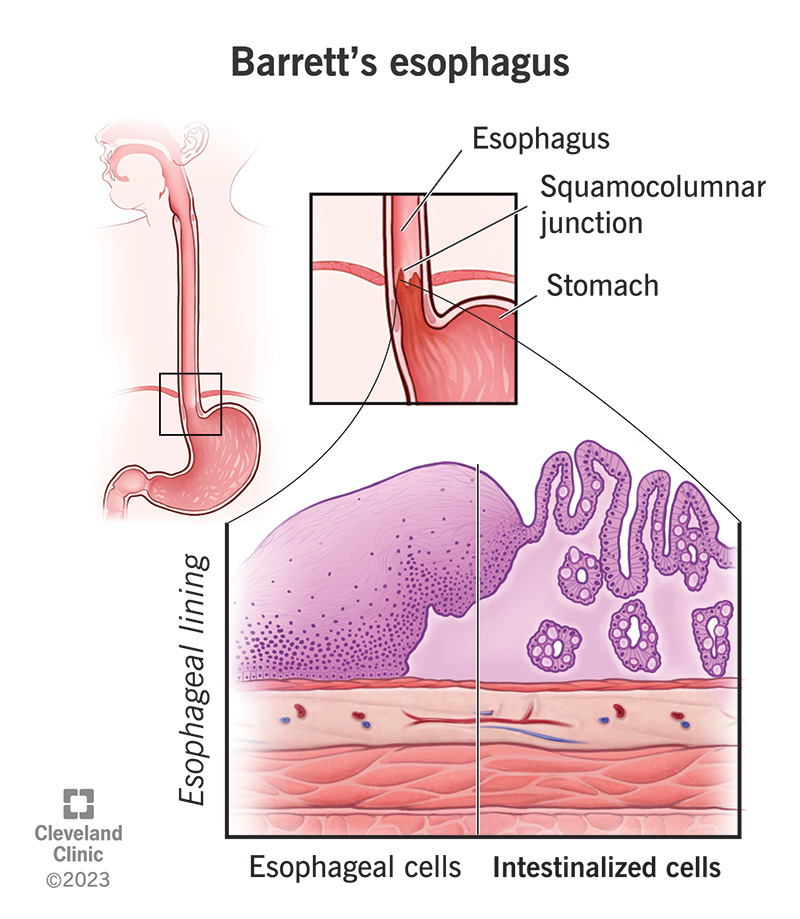
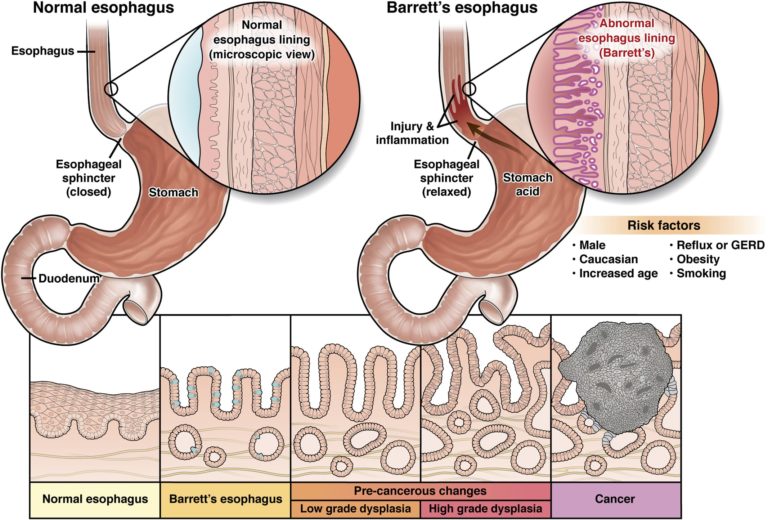
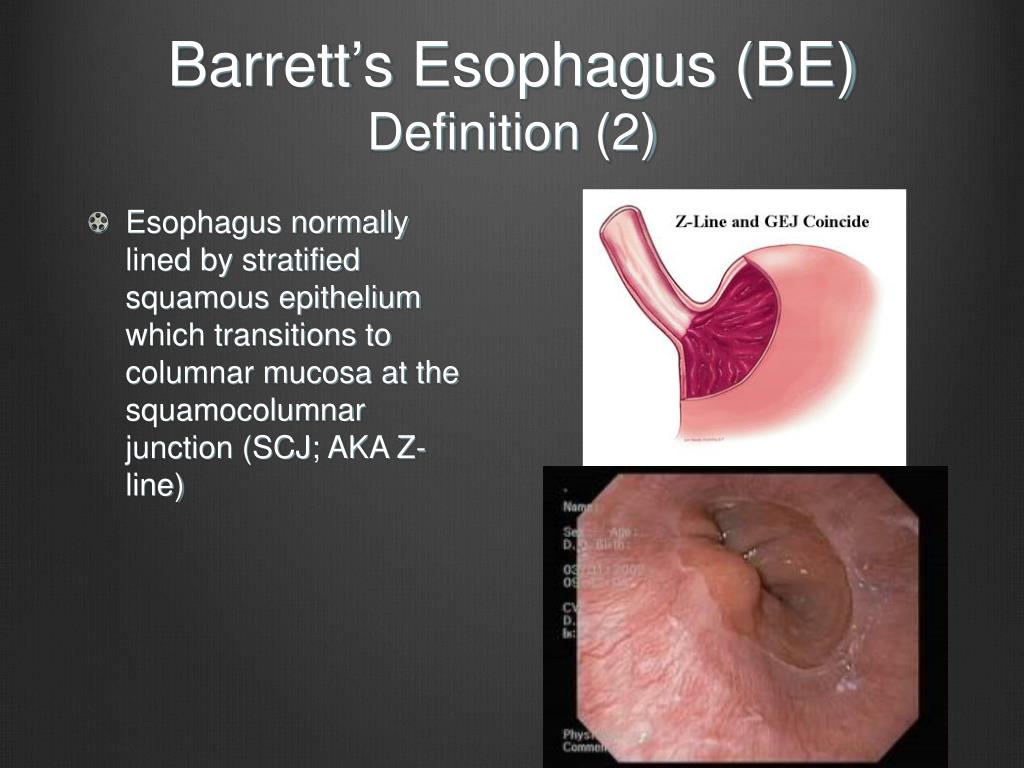
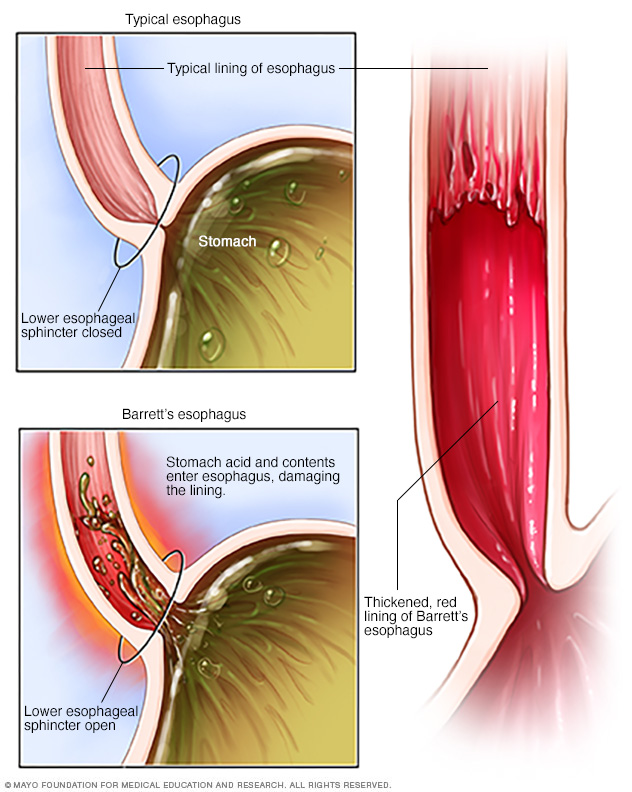
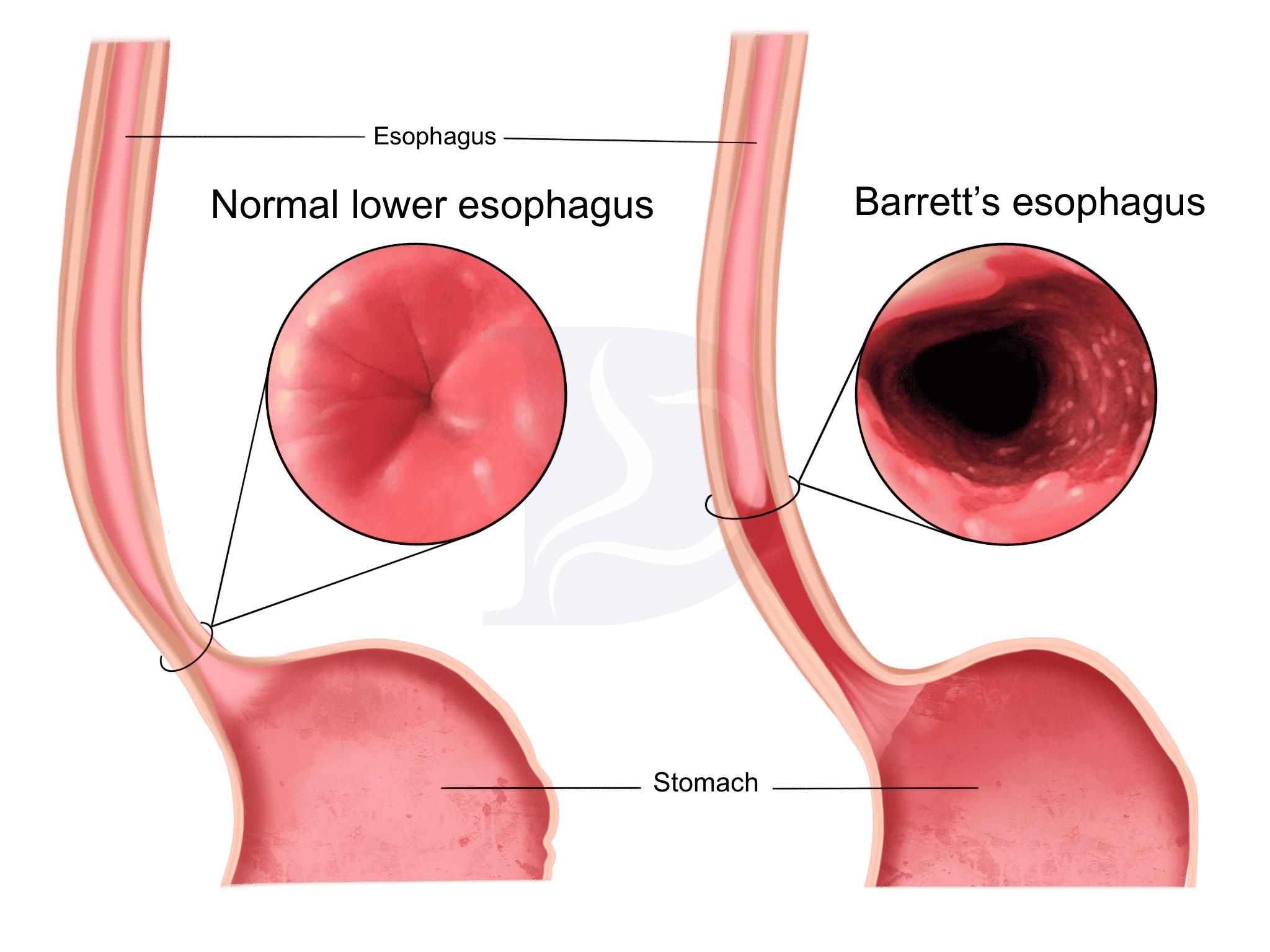
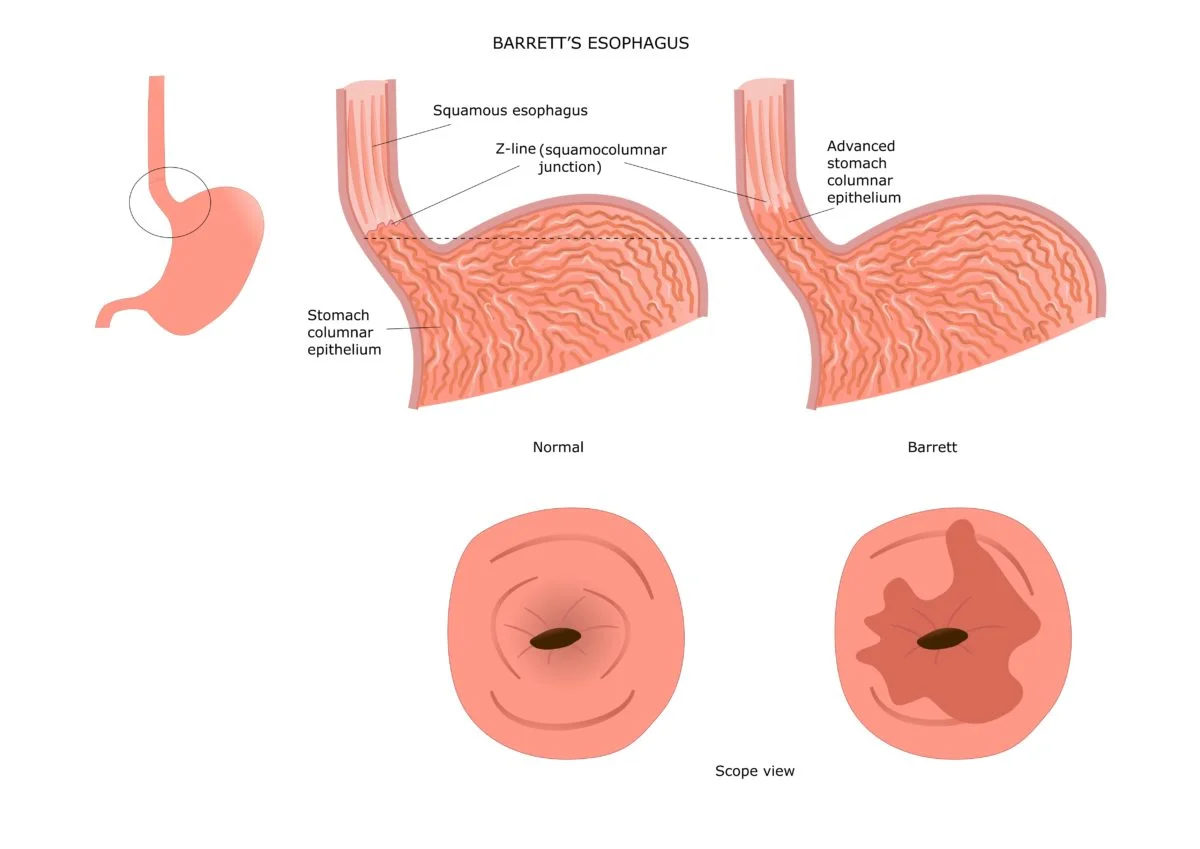
Barrett's esophagus is a condition in which the normal lining of the esophagus, the tube that carries food from the mouth to the stomach, is replaced by tissue similar to that found in the intestine. This change, known as intestinal metaplasia, is typically caused by chronic exposure to stomach acid, most often due to gastroesophageal reflux disease (GERD).
The presence of Barrett's esophagus itself doesn't automatically mean cancer. It simply indicates an increased risk of developing esophageal adenocarcinoma. The key question revolves around the actual magnitude of that increased risk.
Studies have consistently shown that the risk of Barrett's esophagus progressing to cancer is lower than initially perceived. The American Gastroenterological Association, for example, emphasizes that the annual risk of cancer development in individuals with Barrett's esophagus is relatively low, typically ranging from 0.1% to 0.5% per year.
Factors Influencing Cancer Progression
Several factors can influence the likelihood of Barrett's esophagus progressing to esophageal adenocarcinoma. These factors include the presence and degree of dysplasia, the length of the Barrett's segment, and lifestyle choices.
Dysplasia: A Critical Marker
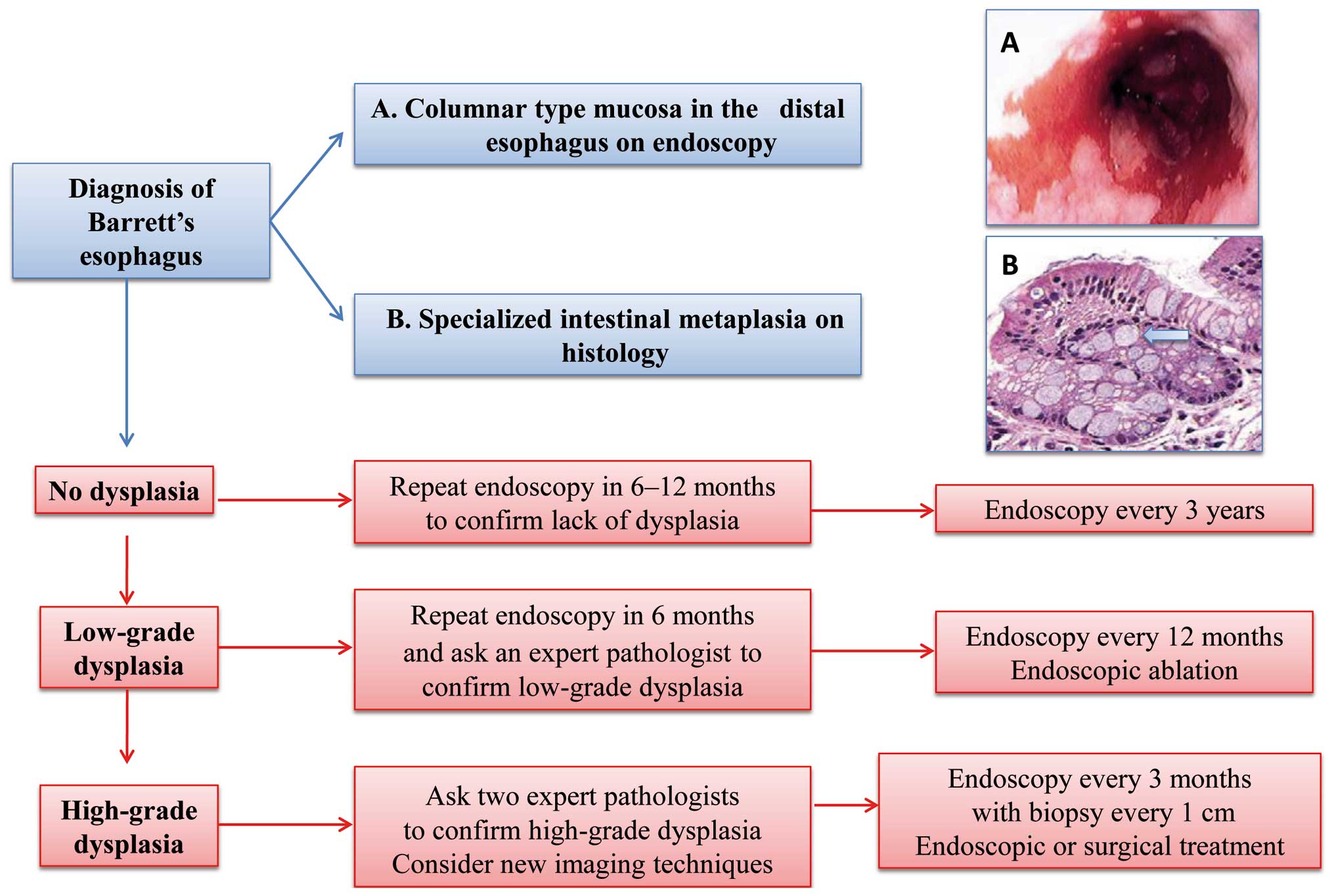
Dysplasia refers to abnormal cell growth within the Barrett's tissue. It's categorized as either low-grade dysplasia or high-grade dysplasia, with the latter carrying a significantly higher risk of progressing to cancer.
Patients with high-grade dysplasia are often recommended to undergo more aggressive treatment options, such as endoscopic ablation or even esophagectomy, to prevent cancer development. The absence of dysplasia is reassuring, though continued surveillance remains crucial.
Segment Length Matters
The length of the Barrett's esophagus segment is another important consideration. Longer segments are generally associated with a higher risk of cancer progression compared to shorter segments.
This is because longer segments provide a larger area for abnormal cells to develop and potentially progress to dysplasia and ultimately cancer. Regular endoscopic surveillance is particularly important for individuals with longer segments.
Lifestyle and Environmental Factors
Certain lifestyle and environmental factors can also influence the risk of cancer development in individuals with Barrett's esophagus. Smoking, obesity, and a diet low in fruits and vegetables have been linked to an increased risk.
Conversely, maintaining a healthy weight, avoiding smoking, and consuming a diet rich in fruits and vegetables may help to reduce the risk. Management of GERD is also crucial to minimize further damage to the esophagus.
Surveillance and Management Strategies
Regular endoscopic surveillance is the cornerstone of managing Barrett's esophagus. This involves periodic endoscopies with biopsies to monitor the esophageal lining for any signs of dysplasia or cancer.
The frequency of surveillance depends on the individual's risk factors and the presence or absence of dysplasia. The American College of Gastroenterology recommends surveillance every 3-5 years for patients without dysplasia.
Endoscopic ablation techniques, such as radiofrequency ablation (RFA), are often used to eradicate Barrett's esophagus tissue, particularly in patients with dysplasia. This procedure uses heat energy to destroy the abnormal cells, reducing the risk of cancer development.
The Patient Perspective and Future Directions
Living with Barrett's esophagus can be emotionally challenging, and knowledge is empowering. Open communication with a gastroenterologist is essential for understanding the individual's risk profile and developing an appropriate management plan.
Research continues to advance our understanding of Barrett's esophagus and its progression to cancer. New biomarkers and imaging techniques are being developed to better identify individuals at high risk and to improve early detection of cancer.
Furthermore, studies are exploring chemopreventive agents that may help to reduce the risk of cancer development in individuals with Barrett's esophagus. These advances offer hope for even more effective prevention and treatment strategies in the future.
Conclusion
While the diagnosis of Barrett's esophagus warrants careful attention, it's important to remember that the risk of cancer progression is relatively low for most individuals. Regular surveillance, appropriate management of GERD, and healthy lifestyle choices can significantly reduce the risk.
By staying informed, actively participating in their care, and working closely with their healthcare providers, individuals with Barrett's esophagus can effectively manage their condition and live long, healthy lives. Fear can be replaced by proactive management and hope for a future free from esophageal cancer.








.png)
