How To Know If You Metabolize Medication Too Fast
Imagine taking a medication prescribed to alleviate pain, manage a chronic condition, or even save your life, only to find it doesn't work as expected. This isn't always due to the wrong drug or dosage; sometimes, your body processes the medication too quickly, rendering it ineffective. Knowing how to identify rapid metabolism is crucial for effective treatment and improved health outcomes.
This article delves into the critical issue of rapid drug metabolism, explaining how to recognize the signs, understand the underlying causes, and what steps to take if you suspect your body is processing medications too fast. We will explore the genetic factors, lifestyle influences, and potential solutions that healthcare providers can employ to optimize treatment for individuals with this metabolic trait. Understanding rapid metabolism is essential for ensuring that medications work as intended and for minimizing potential health risks.
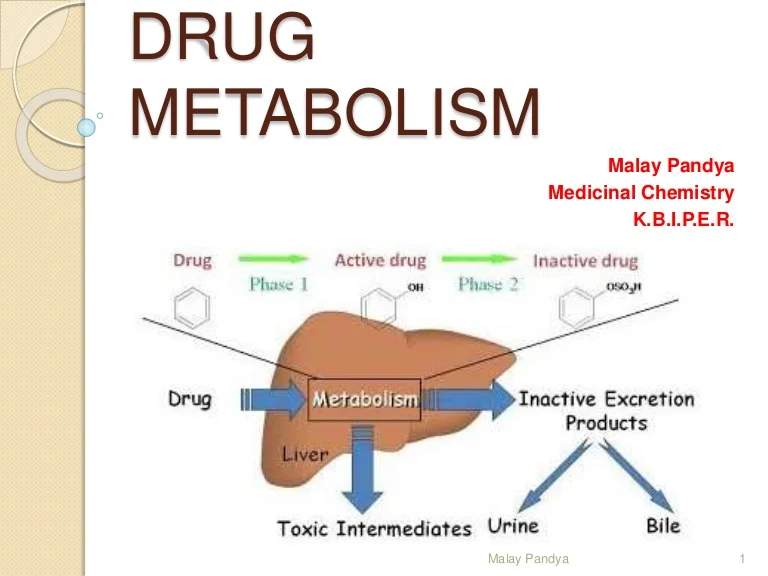
Understanding Drug Metabolism
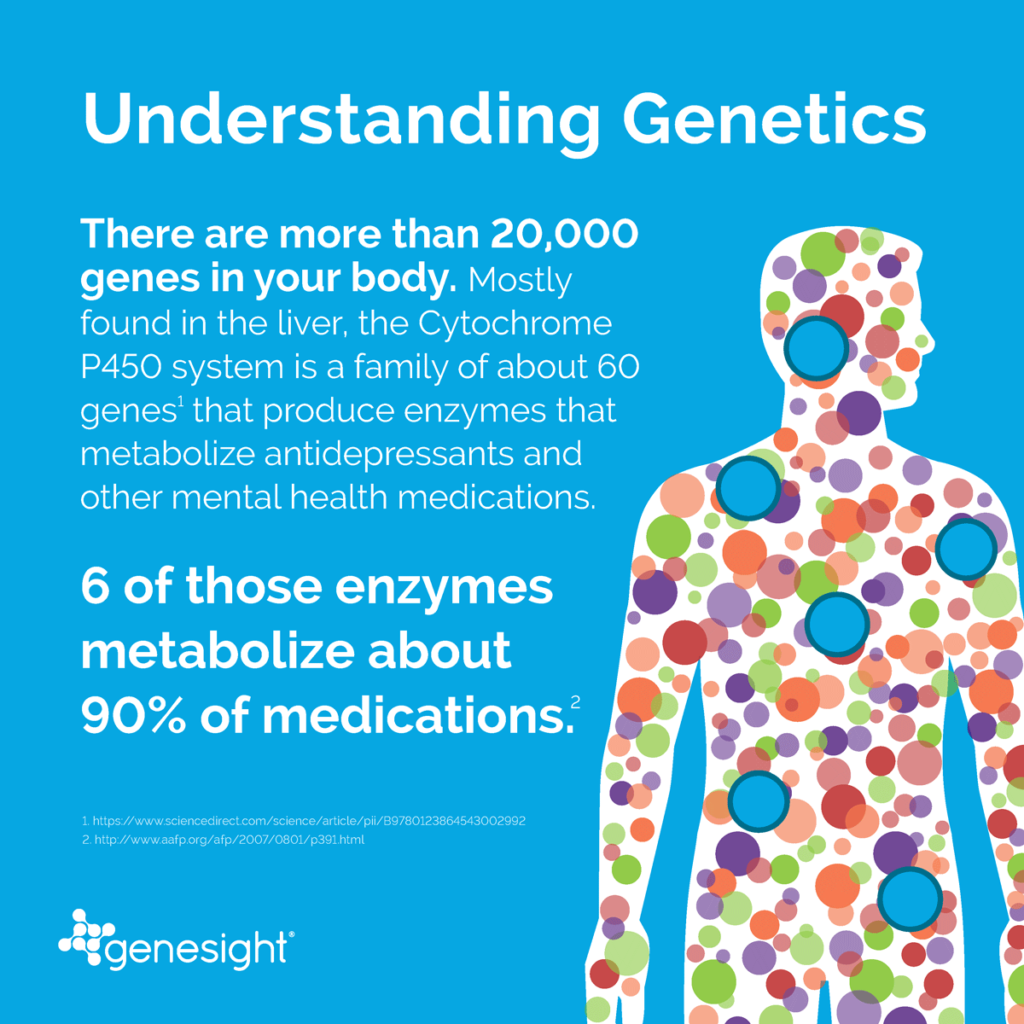
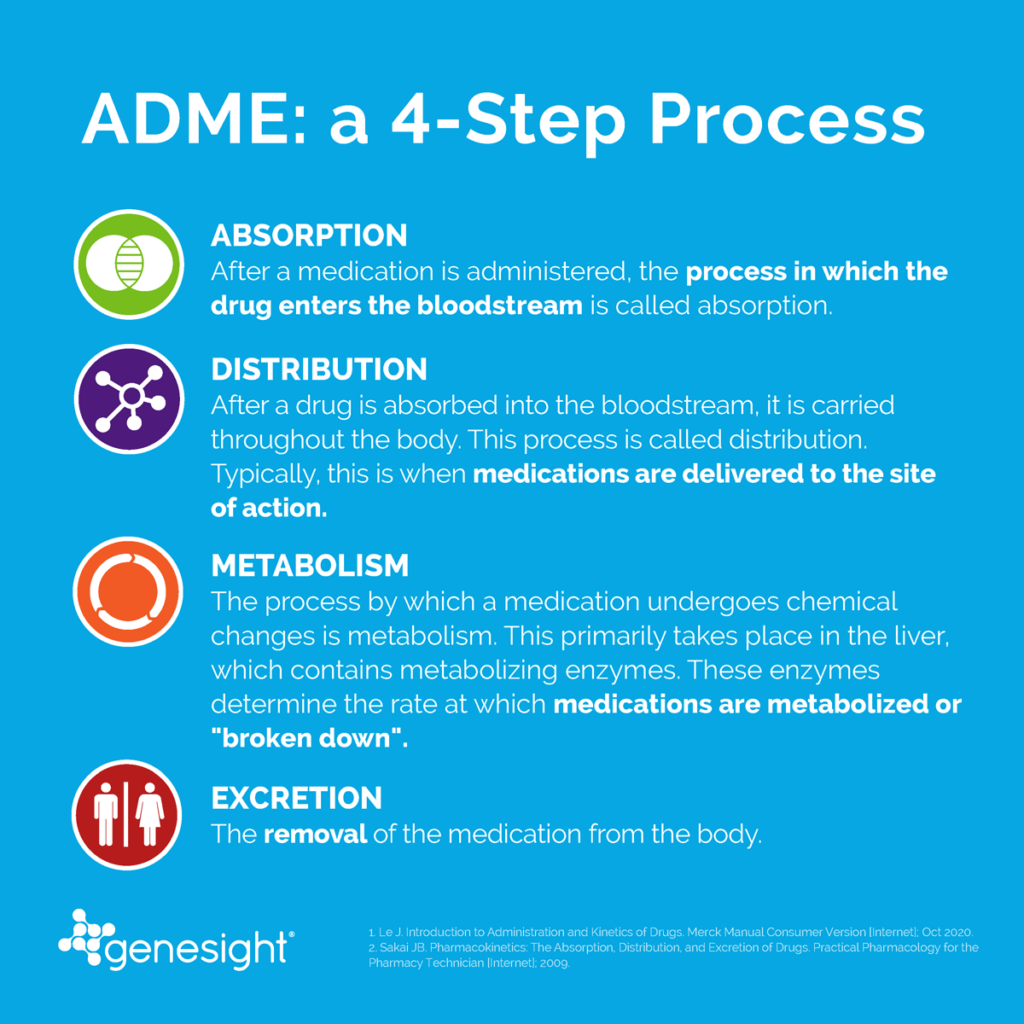
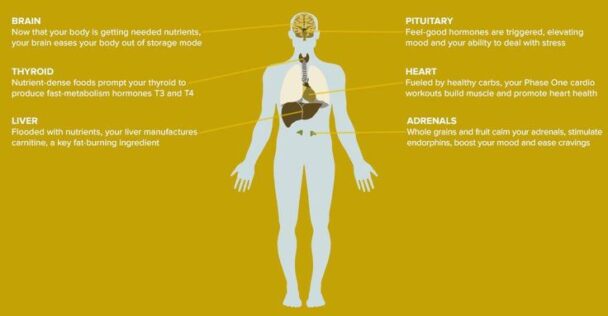
Drug metabolism, also known as biotransformation, is the process by which the body breaks down and eliminates medications. This process primarily occurs in the liver, where enzymes, particularly the cytochrome P450 (CYP450) enzyme family, play a crucial role. These enzymes transform drugs into metabolites, which are often easier for the body to excrete.
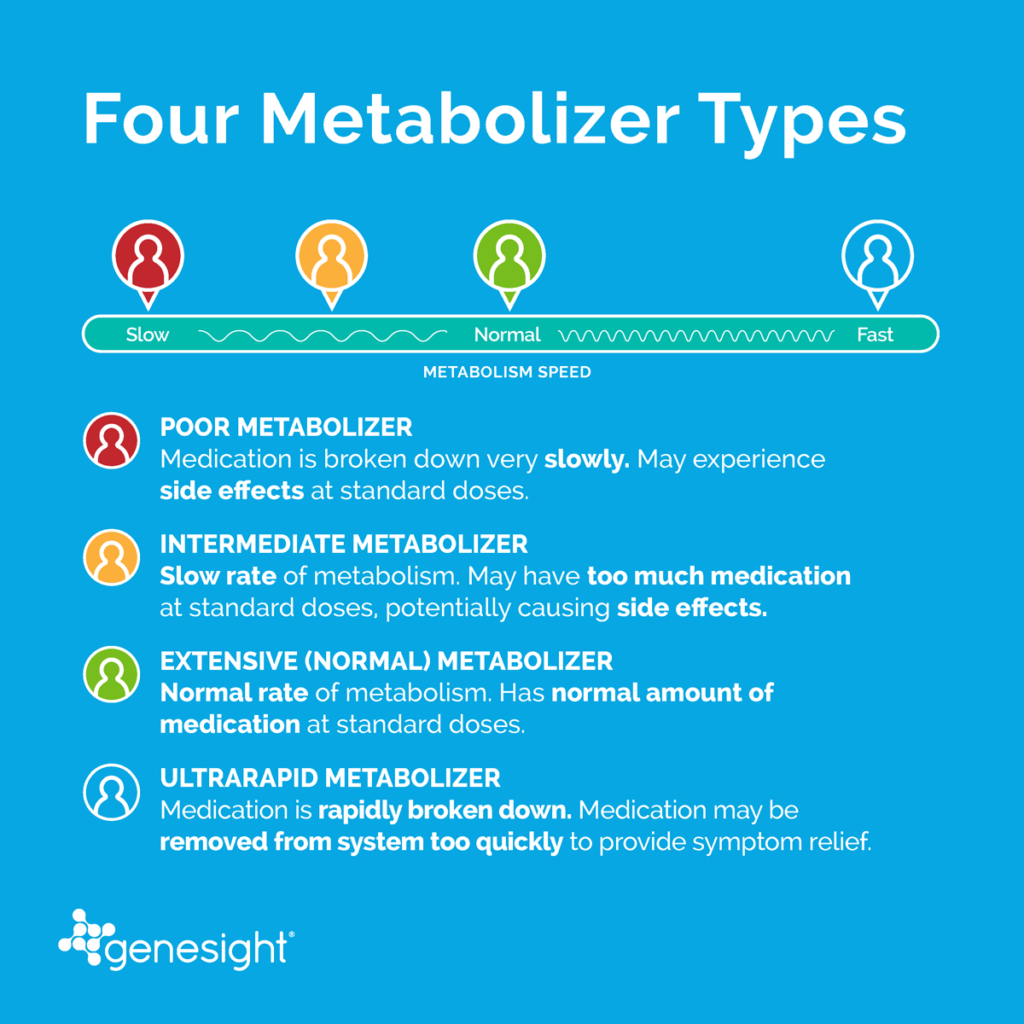
The rate at which individuals metabolize drugs varies significantly due to factors like genetics, age, sex, liver function, diet, and other medications. Some people are extensive metabolizers, processing drugs at a normal rate. Others are either slow metabolizers, leading to drug accumulation and potential side effects, or rapid metabolizers, which can result in subtherapeutic drug levels.
Identifying the Signs of Rapid Metabolism
Recognizing the signs of rapid drug metabolism can be challenging, as symptoms often mimic a lack of response to the medication. A key indicator is the medication not providing the expected therapeutic effect, even when taken at the prescribed dose and frequency. This might manifest as persistent pain despite taking painkillers, continued anxiety despite anti-anxiety medication, or breakthrough seizures despite anti-epileptic drugs.
Another sign is the drug seeming to wear off much sooner than expected. For instance, a painkiller meant to last six hours might only provide relief for three or four. Observing the frequency and severity of symptoms returning prematurely is critical.
It's also important to consider if higher-than-usual doses are needed to achieve the desired effect. If a doctor consistently needs to increase the dosage of a medication to get it to work, rapid metabolism could be the reason.
Factors Contributing to Rapid Metabolism
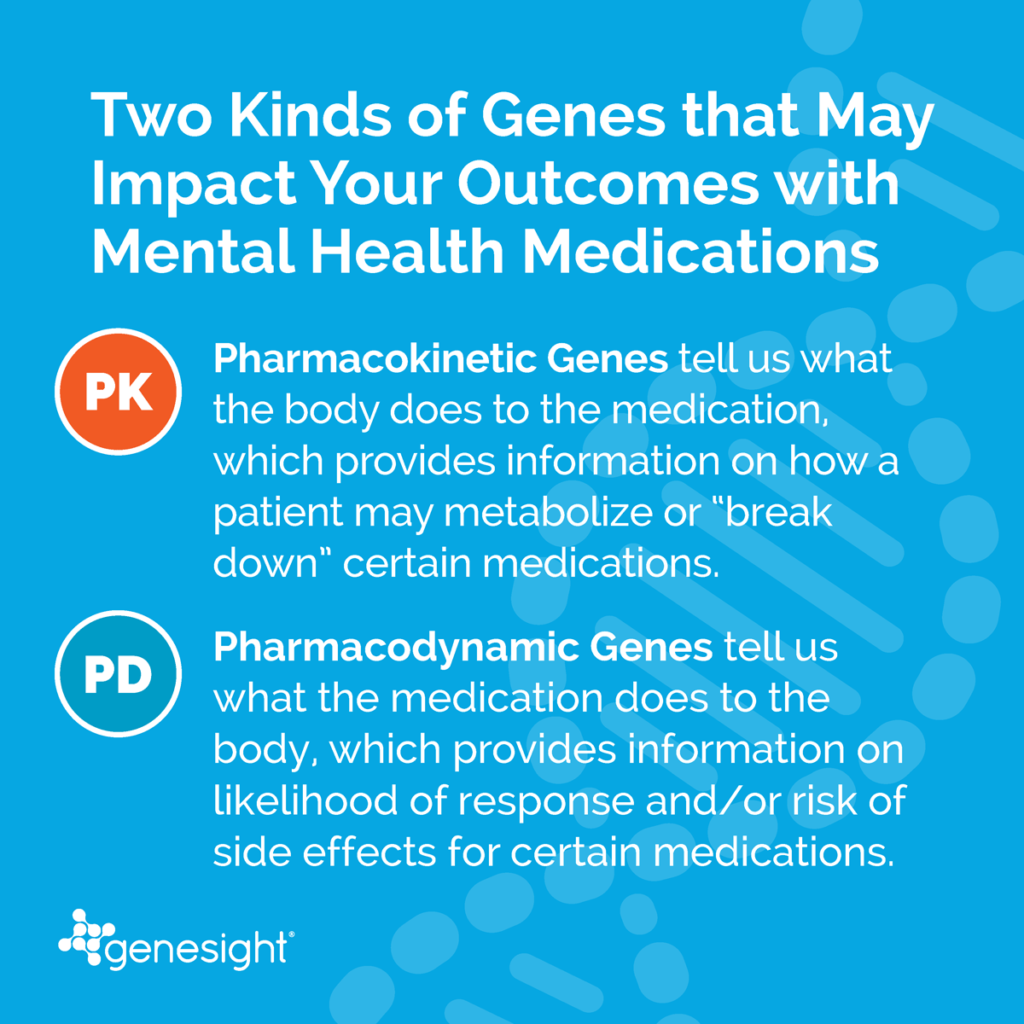
Genetics is a primary driver of drug metabolism rates. Variations in genes encoding CYP450 enzymes can significantly affect their activity. Individuals with gene variants that increase enzyme activity are more likely to be rapid metabolizers.
CYP450 enzymes exhibit genetic polymorphism, meaning different individuals possess different versions of the genes that code for these enzymes. Some versions lead to enhanced enzymatic activity. Pharmacogenetic testing can identify these variants and predict an individual's metabolic capacity.
Certain substances can induce the activity of CYP450 enzymes, leading to faster drug metabolism. Examples include St. John's Wort, a herbal supplement, and certain foods like charbroiled meats and cruciferous vegetables. These substances can accelerate the breakdown of drugs, potentially reducing their effectiveness.
Certain medications can also induce the activity of CYP450 enzymes, leading to faster drug metabolism. For example, Rifampin, an antibiotic used to treat tuberculosis, is a known inducer of several CYP450 enzymes.
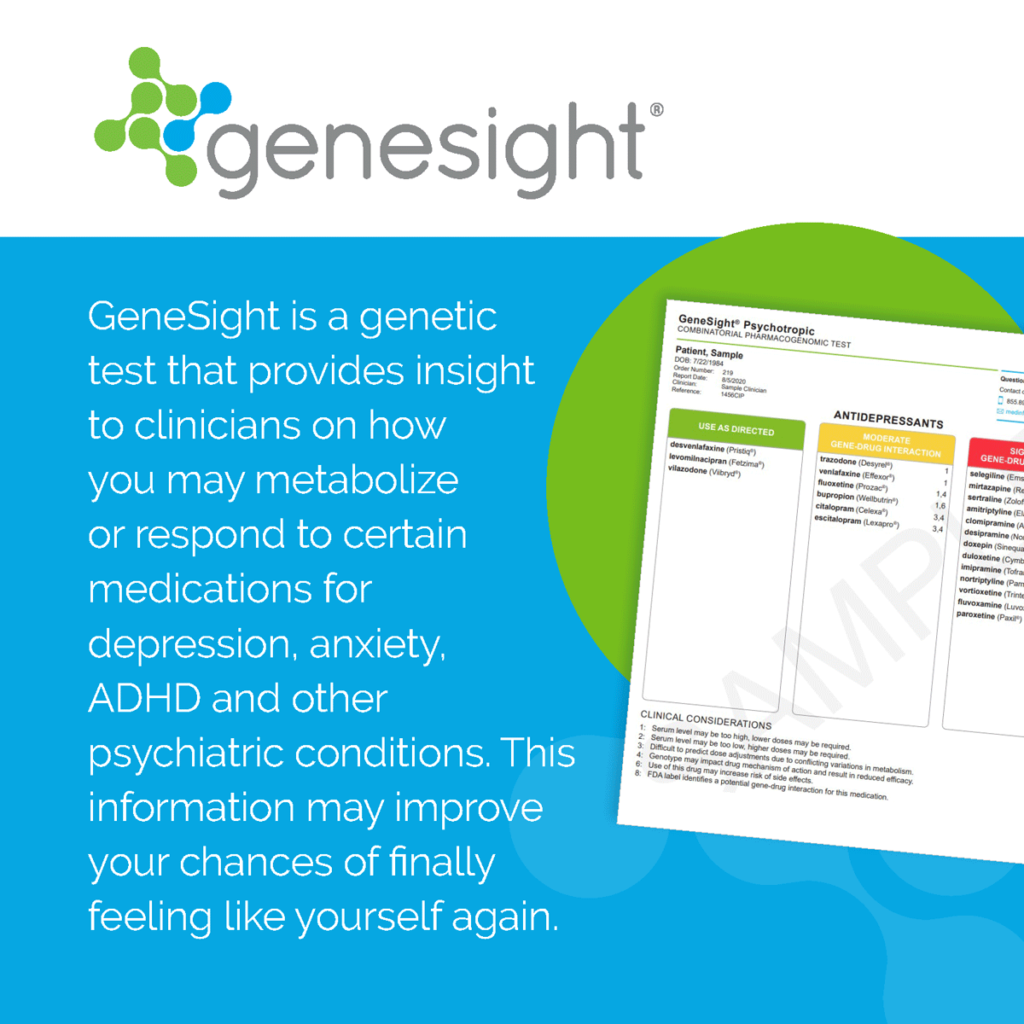
The Role of Pharmacogenetic Testing
Pharmacogenetic testing analyzes a person's genes to predict how they will respond to certain medications. This information can help healthcare providers choose the right drug and dosage, minimizing the risk of ineffectiveness or adverse effects.
A pharmacogenetic test usually involves a simple blood or saliva sample. The sample is analyzed to identify specific gene variants that affect drug metabolism. The results provide insights into whether an individual is a slow, normal, or rapid metabolizer for particular drugs.
By knowing a patient's metabolic profile, healthcare providers can tailor treatment plans to optimize drug effectiveness and safety. This personalized approach to medicine can significantly improve patient outcomes.
What To Do If You Suspect Rapid Metabolism
If you suspect you are metabolizing medications too quickly, the first step is to consult with your healthcare provider. Be prepared to provide detailed information about your symptoms, medications, dosages, and any other relevant health information.
Request a pharmacogenetic test. If rapid metabolism is suspected, this test can confirm the diagnosis and guide treatment decisions.
Work with your doctor to adjust your medication regimen. This might involve increasing the dosage, switching to a different medication that is not affected by rapid metabolism, or using a formulation with a longer duration of action.
Adjusting Medication Strategies
For rapid metabolizers, healthcare providers have several strategies to ensure medication effectiveness. One approach is to increase the dosage of the medication, but this needs to be carefully monitored to avoid potential side effects.
Another strategy is to switch to a different medication that is not metabolized by the same enzymes or is less susceptible to rapid metabolism. This might involve trying a different drug within the same class of medications.
Extended-release formulations can also be beneficial. These formulations release the drug slowly over time, maintaining a more consistent blood level and potentially overcoming the effects of rapid metabolism.
The Future of Personalized Medicine
Understanding and addressing rapid drug metabolism is a key aspect of personalized medicine. As genetic testing becomes more accessible and affordable, it will play an increasingly important role in optimizing medication therapy.
The future of medicine will likely involve routine pharmacogenetic testing before prescribing certain medications. This proactive approach will allow healthcare providers to tailor treatment plans to individual genetic profiles, improving outcomes and reducing the risk of adverse effects.
Ongoing research is also focused on developing new drugs that are less susceptible to metabolic variations. These innovations will further enhance our ability to personalize treatment and improve patient care.
In conclusion, recognizing the signs of rapid drug metabolism and taking proactive steps to address it is essential for effective medication management. By understanding the underlying factors, utilizing pharmacogenetic testing, and collaborating with healthcare providers, individuals can ensure that their medications work as intended, leading to improved health and well-being. Empowering yourself with knowledge is the first step towards optimizing your treatment and achieving the best possible health outcomes.