How To Treat Bv And Uti Together

For many women, the discomfort of a urinary tract infection (UTI) or bacterial vaginosis (BV) is a frustratingly familiar experience. But what happens when these two common conditions occur simultaneously? The overlapping symptoms can make diagnosis tricky, and the need for tailored treatment strategies becomes paramount. Navigating this dual infection requires understanding the nuances of each condition and consulting with healthcare professionals to ensure effective and safe management.
This article delves into the complexities of co-occurring BV and UTIs, providing insights into diagnosis, treatment options, and preventive measures. Understanding the distinct nature of each infection is crucial for effective treatment. We aim to equip readers with the knowledge necessary to address these conditions and seek appropriate medical care.
Understanding the Conditions
Bacterial Vaginosis (BV)
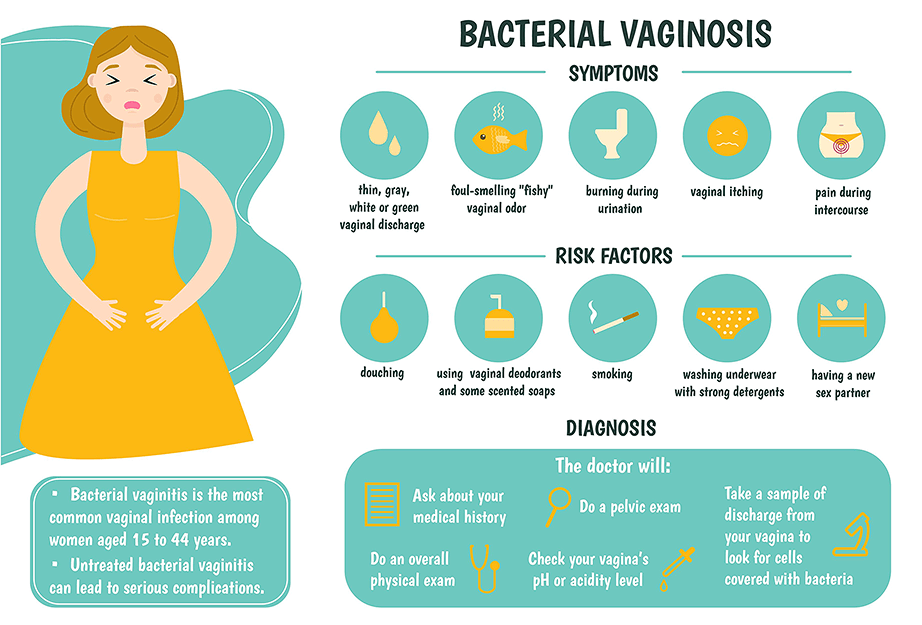
Bacterial vaginosis is a common vaginal infection caused by an imbalance of bacteria. Typically, lactobacilli dominate the vaginal flora, maintaining an acidic environment that inhibits the growth of other bacteria. When this balance is disrupted, other bacteria, such as Gardnerella vaginalis, can overgrow, leading to BV.
Symptoms often include a thin, grayish-white discharge, a fishy odor, and sometimes itching or burning. However, many women with BV experience no symptoms at all. Diagnosis is typically made via pelvic exam, assessment of vaginal discharge, and pH testing.
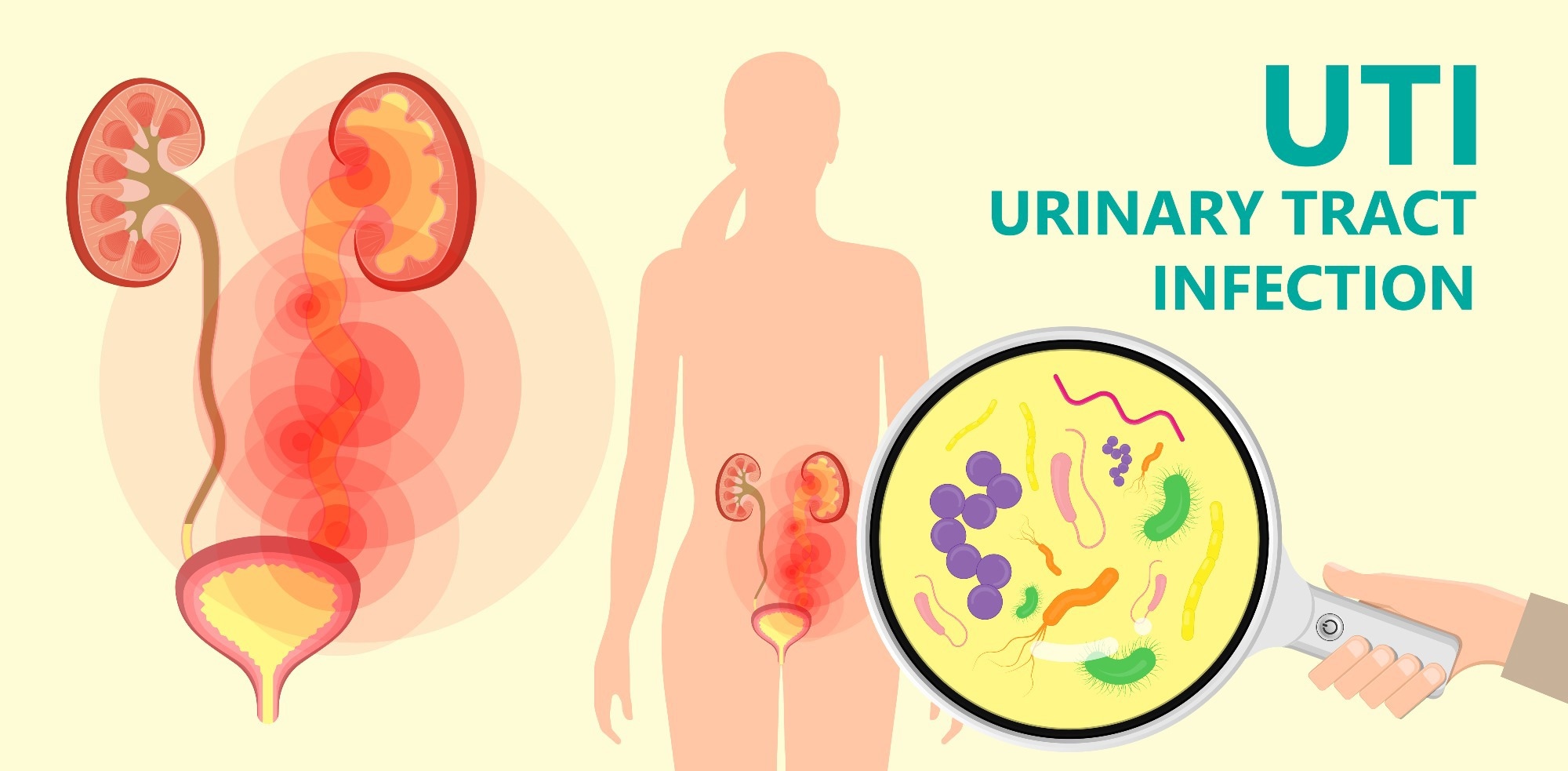
Urinary Tract Infection (UTI)
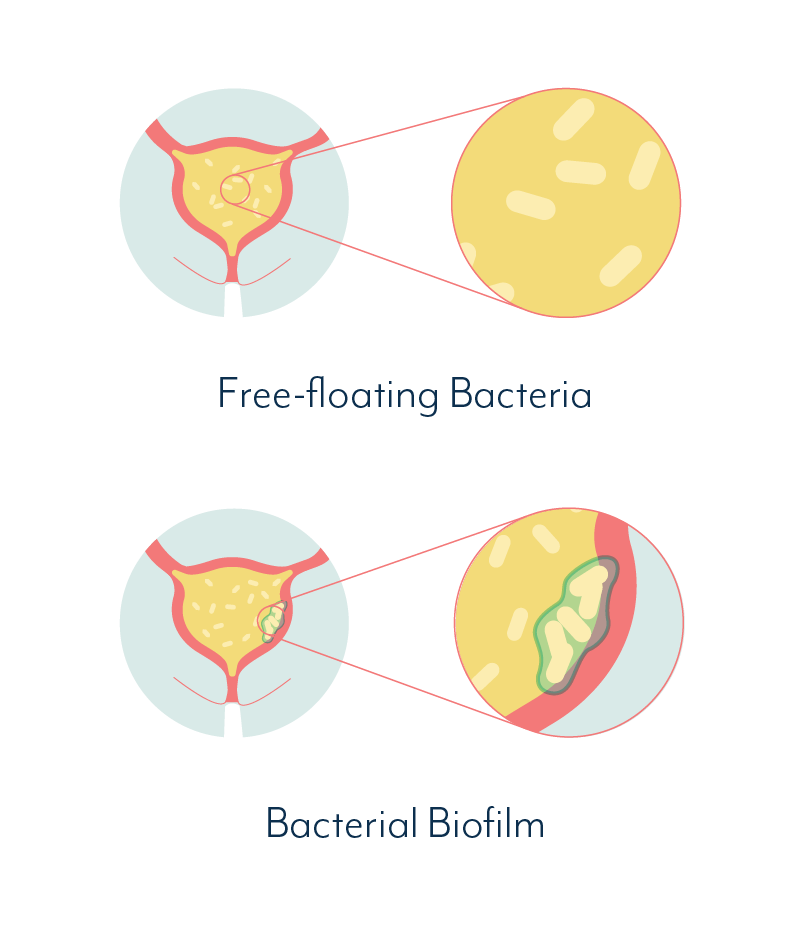
A UTI is an infection in any part of the urinary system, which includes the kidneys, ureters, bladder, and urethra. Most UTIs involve the lower urinary tract (bladder and urethra). Escherichia coli (E. coli) is the most common culprit, but other bacteria can also cause UTIs.
Common symptoms include a persistent urge to urinate, a burning sensation during urination, frequent urination, cloudy urine, and pelvic pain. More severe UTIs can involve kidney infection, characterized by back pain, fever, and chills. A urine test confirms the presence of bacteria and white blood cells, indicating infection.
Co-occurrence and Overlapping Symptoms
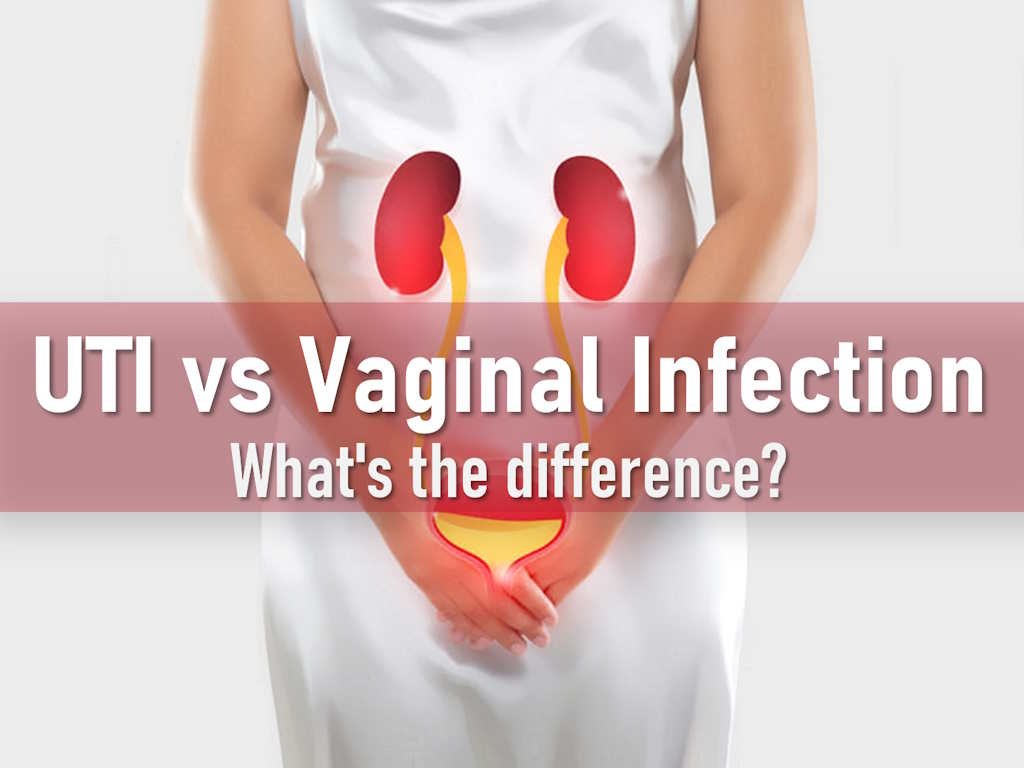
While BV and UTIs are distinct infections, their symptoms can sometimes overlap or be confused. Both conditions can cause pelvic discomfort and an increased urge to urinate. This overlap can lead to misdiagnosis or delayed treatment.
Furthermore, having BV can potentially increase the risk of developing a UTI, although the exact mechanisms are still being researched. Changes in the vaginal flora can disrupt the natural defenses against bacteria ascending into the urinary tract.
Diagnosis: Differentiating BV and UTI
Accurate diagnosis is critical for effective treatment. A healthcare provider will typically perform a pelvic exam and collect samples for testing. This allows for the differentiation between BV and a UTI.
For BV, the doctor will analyze the vaginal discharge to identify the type and amount of bacteria present, perform a pH test and possibly a whiff test (assessing odor after adding potassium hydroxide). A urine sample is analyzed to check for bacteria, white blood cells, and red blood cells for UTIs.
Treatment Approaches
Treating BV
BV is typically treated with antibiotics prescribed by a doctor. Metronidazole and clindamycin are the most commonly prescribed antibiotics, available in oral or topical forms. It’s crucial to complete the full course of antibiotics, even if symptoms improve, to prevent recurrence.
Over-the-counter treatments may alleviate some symptoms, but they do not cure BV. Probiotics can also be used to restore the balance of bacteria in the vagina, but their effectiveness in treating active BV infections is still under investigation.
Treating UTI
UTIs are also treated with antibiotics. The specific antibiotic prescribed depends on the type of bacteria causing the infection and its sensitivity to various medications. Common antibiotics used to treat UTIs include trimethoprim-sulfamethoxazole (Bactrim), nitrofurantoin (Macrobid), and ciprofloxacin (Cipro). As with BV treatment, it is crucial to complete the full course of antibiotics.
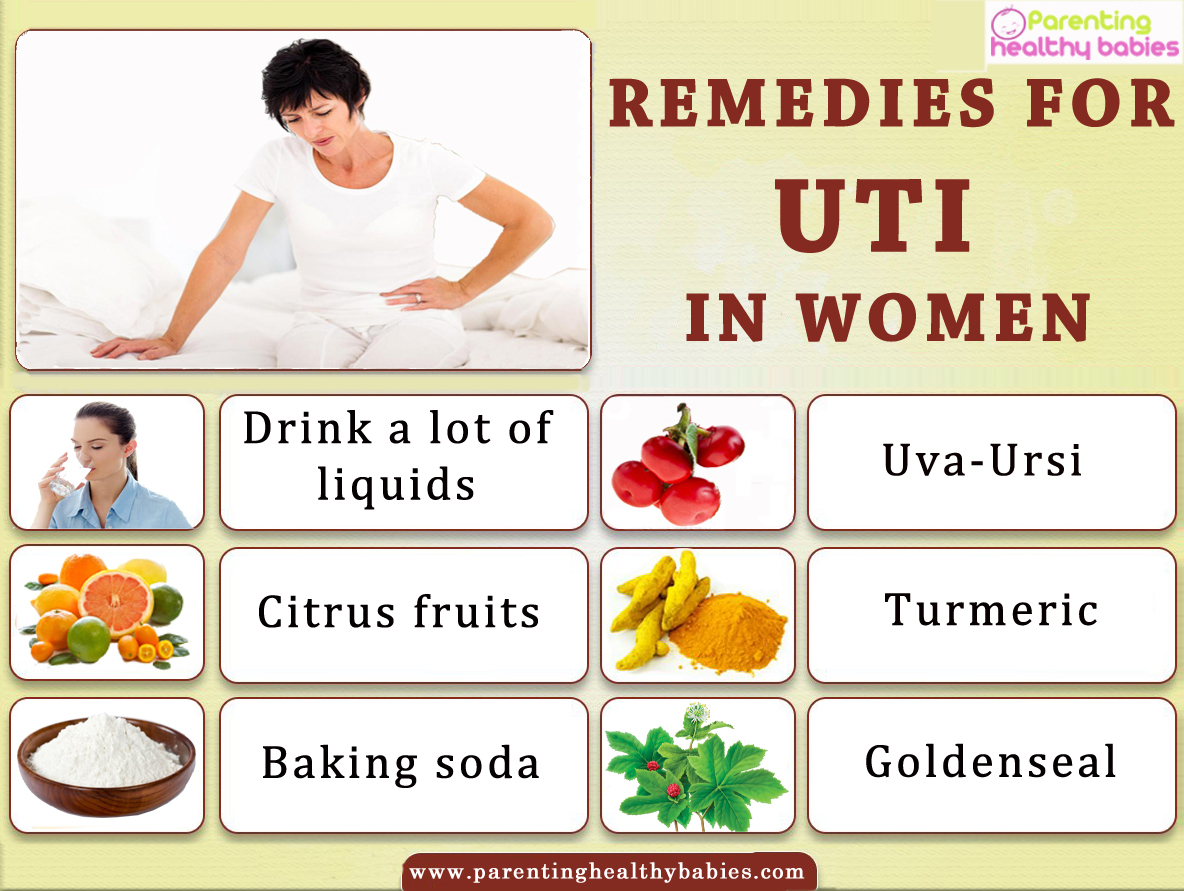
Increasing fluid intake, especially water, can help flush bacteria out of the urinary system. Over-the-counter pain relievers, like phenazopyridine (Pyridium), can help alleviate pain and burning during urination, but they do not treat the infection itself.
Combined Treatment Strategies
When BV and a UTI occur simultaneously, healthcare providers may prescribe antibiotics to target both infections. This could involve taking two different antibiotics concurrently, or selecting a broad-spectrum antibiotic effective against both bacterial types. It is crucial to inform your doctor about all symptoms, including vaginal discharge and urinary symptoms.
Probiotics may be recommended after completing antibiotic courses to help restore the natural balance of bacteria in both the vagina and the urinary tract. Always discuss any potential interactions between medications with your doctor or pharmacist.
Prevention Strategies
Preventing BV
Several steps can be taken to reduce the risk of developing BV. Avoid douching, as it disrupts the natural vaginal flora. Use unscented soaps and detergents. Limit the number of sexual partners, and use condoms consistently.
Preventing UTI
Drinking plenty of water is crucial for preventing UTIs. Urinate frequently and after sexual activity. Wipe from front to back after using the toilet. Consider cranberry products, although their effectiveness is still debated, as they may help prevent bacteria from adhering to the urinary tract walls. Avoid irritating feminine products.
Seeking Professional Help
It is crucial to consult with a healthcare provider for any symptoms suggestive of BV or a UTI. Self-treating can lead to complications and antibiotic resistance. An accurate diagnosis ensures appropriate treatment and prevents the recurrence of infections.
If you experience recurrent UTIs or BV infections, your doctor may recommend further testing to identify underlying causes and develop a long-term management plan. Don't hesitate to seek medical advice if you have concerns or questions about your sexual or urinary health.
Conclusion
Treating BV and UTIs simultaneously requires a comprehensive approach that addresses the unique characteristics of each infection. Accurate diagnosis through medical examination and laboratory testing is essential. Adhering to prescribed antibiotic regimens and adopting preventive measures can significantly improve outcomes. Empowering women with knowledge and encouraging proactive healthcare-seeking behavior are key to managing these common yet uncomfortable conditions effectively and improving overall well-being. Continued research into the interplay between vaginal and urinary health promises to refine treatment strategies and ultimately enhance women’s health.












:max_bytes(150000):strip_icc()/urinary-tract-infections-prevention-3520513-Final-97d8fcb9b123490c852ad3480b982792.png)
