Humira For Ankylosing Spondylitis Reviews
For individuals grappling with the relentless pain and stiffness of ankylosing spondylitis (AS), finding effective treatment can feel like a Sisyphean task. Amidst the landscape of available therapies, Humira (adalimumab), a TNF inhibitor, has emerged as a frequently discussed and prescribed option. But what do real-world experiences and clinical data reveal about its efficacy and impact on the lives of those living with AS?
This article delves into a comprehensive review of Humira's use in treating ankylosing spondylitis, drawing upon clinical trial results, patient reviews, and expert opinions. It aims to provide a balanced perspective on the drug's benefits, potential side effects, and overall value as a therapeutic intervention for this chronic inflammatory condition.
Understanding Humira and Ankylosing Spondylitis
Humira is a biologic medication that belongs to a class of drugs known as TNF inhibitors. These medications work by blocking the action of tumor necrosis factor (TNF), a protein in the body that promotes inflammation. In ankylosing spondylitis, TNF contributes to the inflammation of the spine and other joints, leading to pain, stiffness, and potential structural damage.
Ankylosing spondylitis is a chronic inflammatory disease primarily affecting the spine. Over time, it can cause vertebrae to fuse, resulting in decreased mobility and a hunched posture. The condition can also affect other joints, such as the hips, shoulders, and knees.
Clinical Trial Evidence: Efficacy and Outcomes
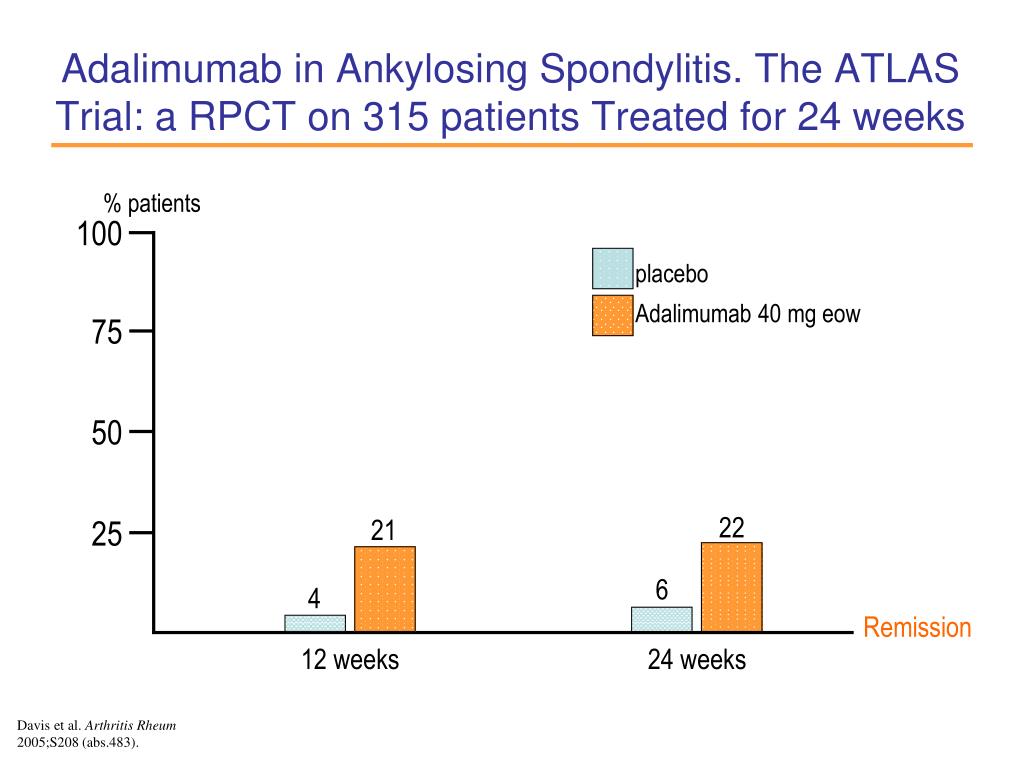
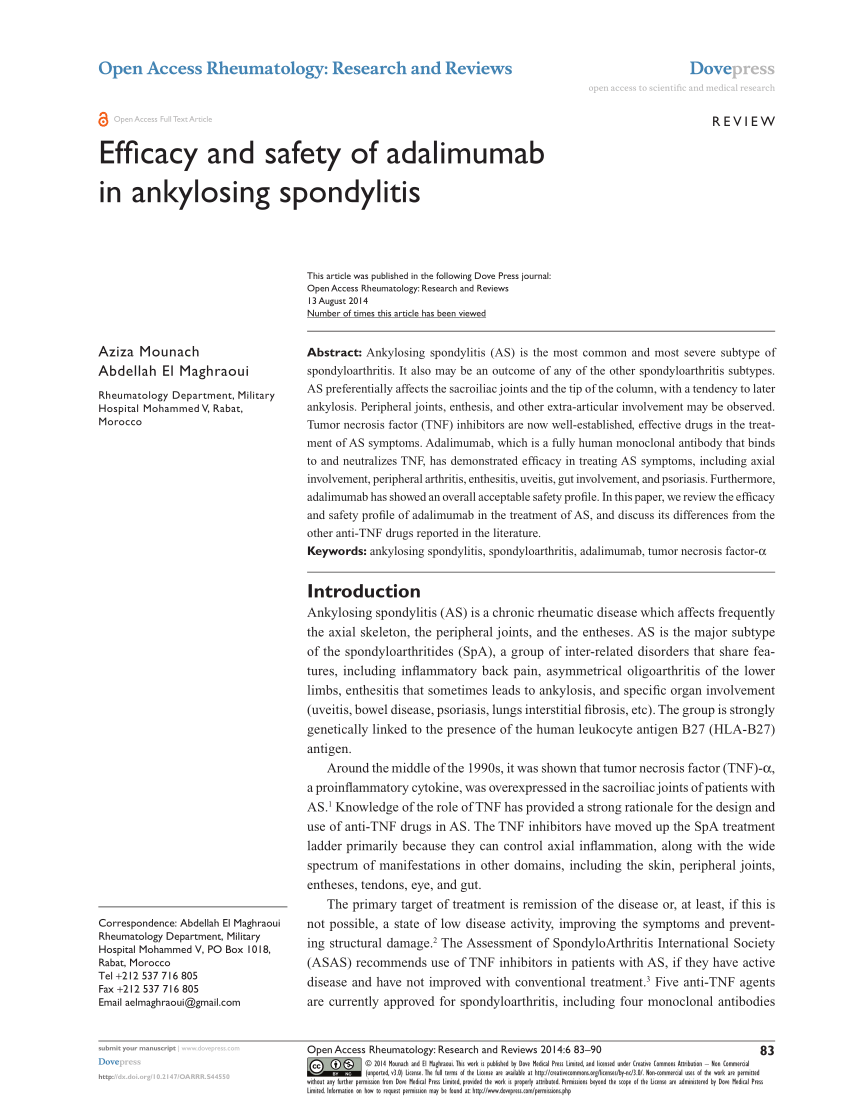
Numerous clinical trials have investigated the efficacy of Humira in treating ankylosing spondylitis. These studies generally show that Humira can significantly reduce symptoms and improve physical function in patients with AS compared to placebo.
One pivotal trial, published in Arthritis & Rheumatology, demonstrated that Humira significantly improved the signs and symptoms of AS, as measured by the Assessment of SpondyloArthritis international Society (ASAS) criteria. Patients receiving Humira experienced greater reductions in pain, stiffness, and inflammation compared to those receiving placebo.
Furthermore, some studies suggest that Humira may slow the progression of structural damage in the spine, although this is an area of ongoing research. The long-term impact on disease modification requires further investigation.
Patient Reviews and Real-World Experiences
While clinical trials provide valuable data, patient reviews offer insights into the real-world experience of using Humira for AS. Many patients report significant improvements in their quality of life, with reduced pain, increased mobility, and improved sleep.
However, it's crucial to acknowledge that experiences can vary. Some patients may not respond as well to Humira, while others may experience bothersome side effects. Individual responses to the medication can be influenced by factors such as disease severity, genetics, and lifestyle.
Online forums and support groups dedicated to ankylosing spondylitis often feature discussions about Humira. These platforms provide a space for patients to share their experiences, ask questions, and offer support to one another.
Potential Side Effects and Risks
Like all medications, Humira carries the risk of side effects. Common side effects include injection site reactions (redness, swelling, pain), upper respiratory infections, and headaches.
More serious, but less common, side effects include an increased risk of infections, such as tuberculosis and fungal infections. Humira can also increase the risk of certain types of cancer, such as lymphoma. It's crucial for patients to discuss the potential risks and benefits of Humira with their healthcare provider.
Regular monitoring by a physician is essential to detect and manage any potential side effects. Patients should report any unusual symptoms or concerns to their doctor promptly.
Alternative Treatments and Considerations
Humira is not the only treatment option available for ankylosing spondylitis. Other TNF inhibitors, such as Enbrel (etanercept) and Remicade (infliximab), are also commonly used. Additionally, non-biologic DMARDs (disease-modifying antirheumatic drugs) like sulfasalazine may be prescribed, particularly for peripheral joint involvement.
Non-pharmacological approaches, such as physical therapy, exercise, and lifestyle modifications, also play a vital role in managing AS. These interventions can help improve mobility, reduce pain, and enhance overall well-being.
The choice of treatment should be individualized based on the patient's specific needs and preferences, as well as the severity of their condition and the presence of any other health issues. A rheumatologist can help guide patients in making informed decisions about their treatment plan.
The Future of Ankylosing Spondylitis Treatment
Research into new and improved treatments for ankylosing spondylitis is ongoing. New biologic therapies, such as IL-17 inhibitors, have emerged as promising options for patients who do not respond adequately to TNF inhibitors.
Furthermore, researchers are exploring novel approaches to target specific pathways involved in the pathogenesis of AS. The ultimate goal is to develop treatments that can not only alleviate symptoms but also prevent or reverse structural damage.
Ultimately, Humira remains a significant therapeutic option for many individuals living with ankylosing spondylitis. While individual experiences may vary, the clinical evidence and patient reports suggest that it can provide substantial relief from symptoms and improve quality of life. Continued research and the development of new therapies offer hope for even better outcomes in the future. Consulting with a rheumatologist to explore all available treatment options is essential for personalized and effective care.