Imbalanced Nutrition Less Than Body Requirements Care Plan

Malnutrition, a condition where the body doesn't receive enough nutrients, can significantly impact health and recovery. Often addressed through a comprehensive "Imbalanced Nutrition Less Than Body Requirements" care plan, healthcare professionals strive to restore and maintain optimal nutritional status for their patients.
This article examines the crucial components of such a care plan, shedding light on its significance, implementation, and impact on patient outcomes. It aims to provide a clear understanding of this vital aspect of healthcare.
Understanding the Care Plan
The "Imbalanced Nutrition Less Than Body Requirements" care plan is a structured, individualized approach designed to address nutritional deficits. These deficits can arise from a variety of causes, including illness, surgery, age-related changes, or socioeconomic factors.
At its core, the plan aims to identify the root causes of malnutrition, calculate the patient's specific nutritional needs, and implement strategies to meet those needs effectively. This process is collaborative, involving doctors, nurses, registered dietitians, and the patient themselves.
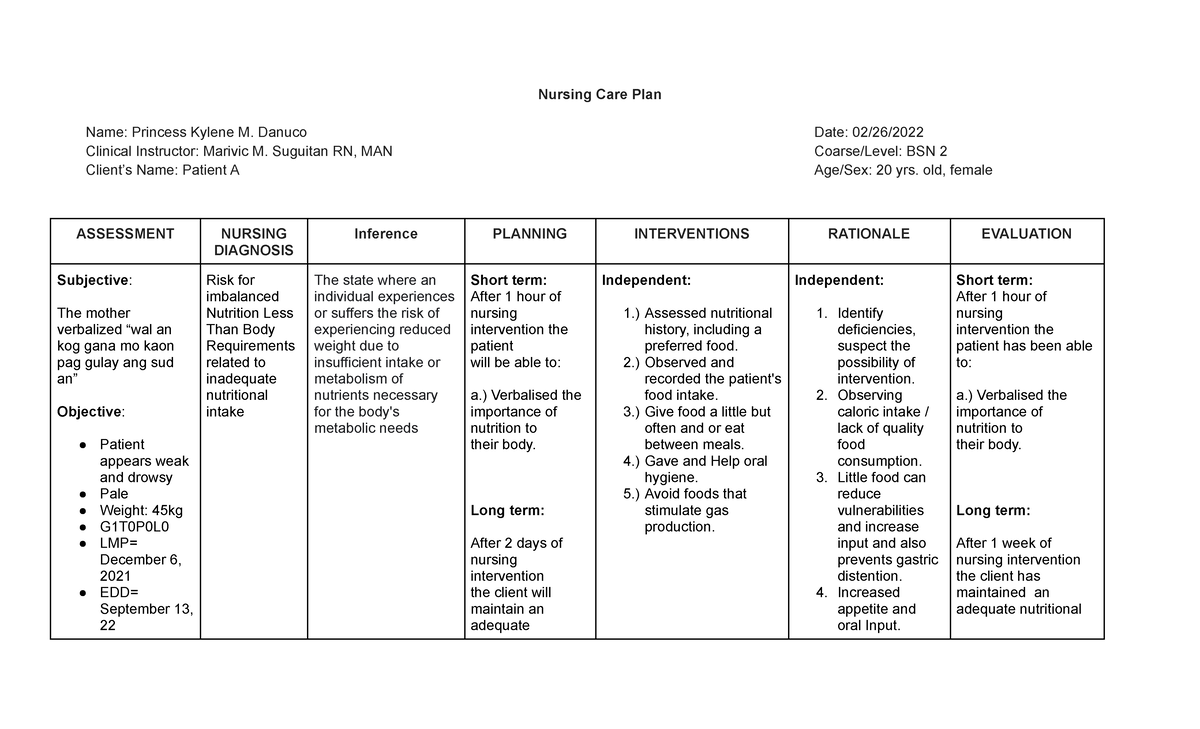
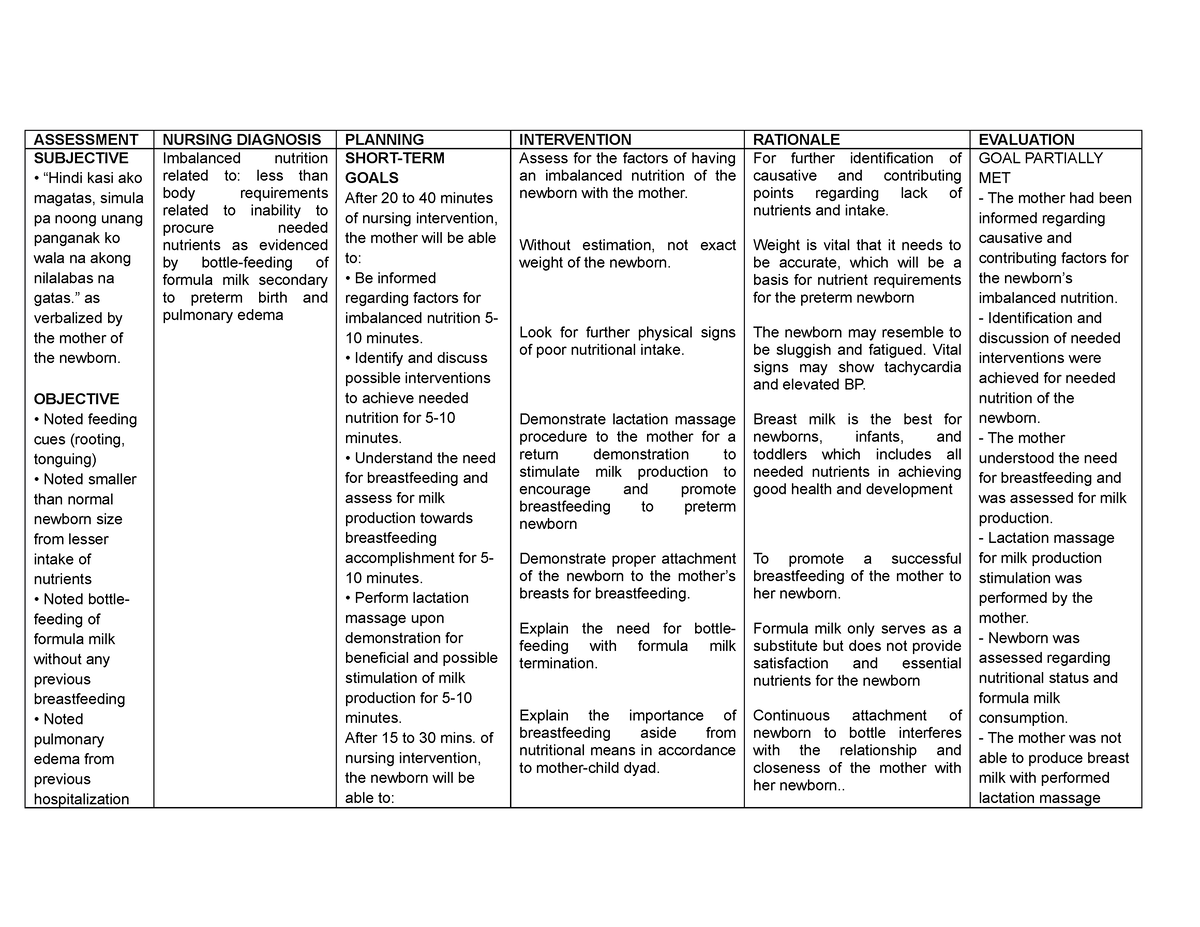
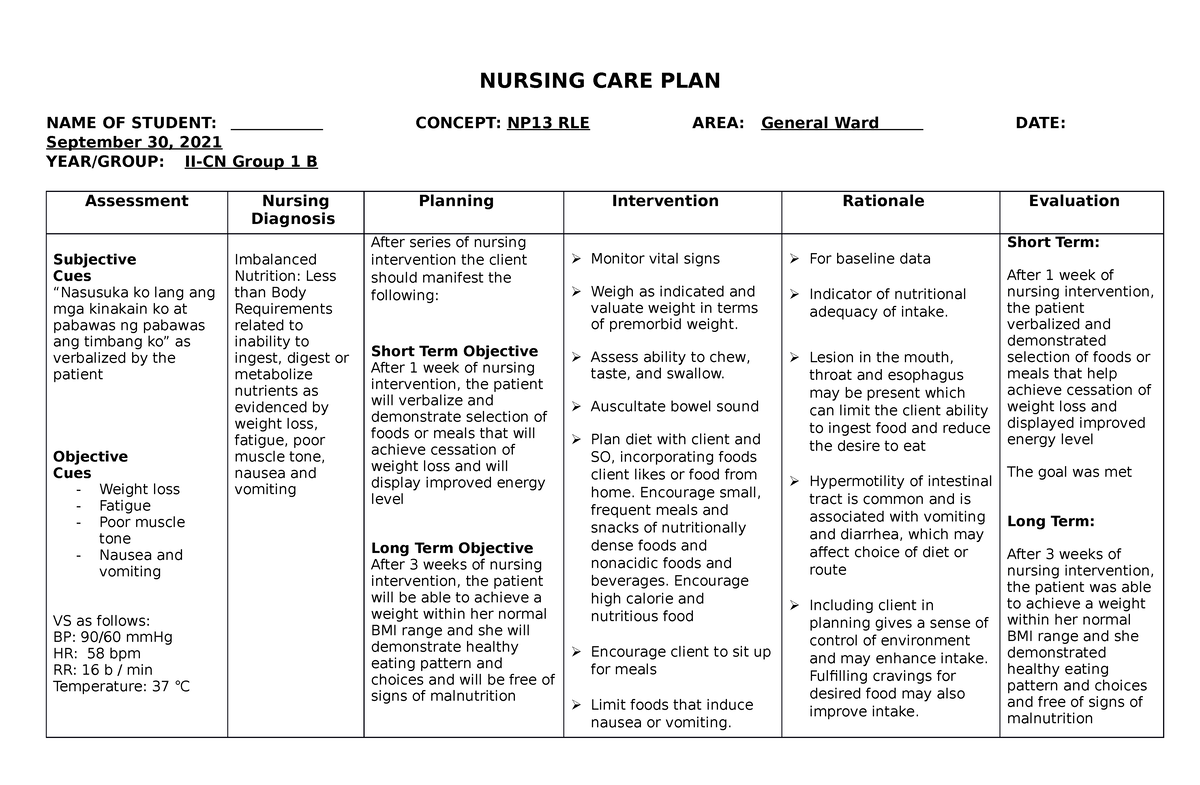
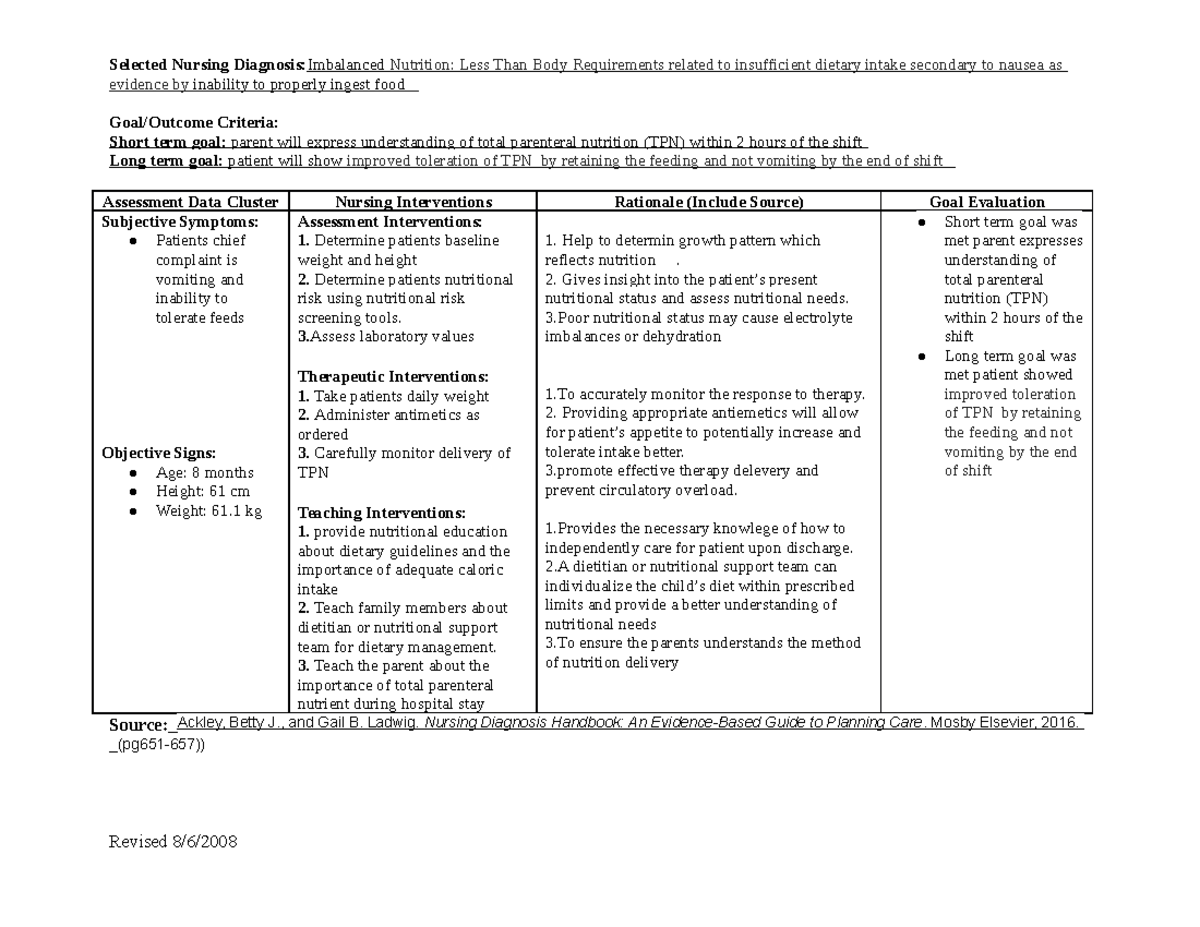
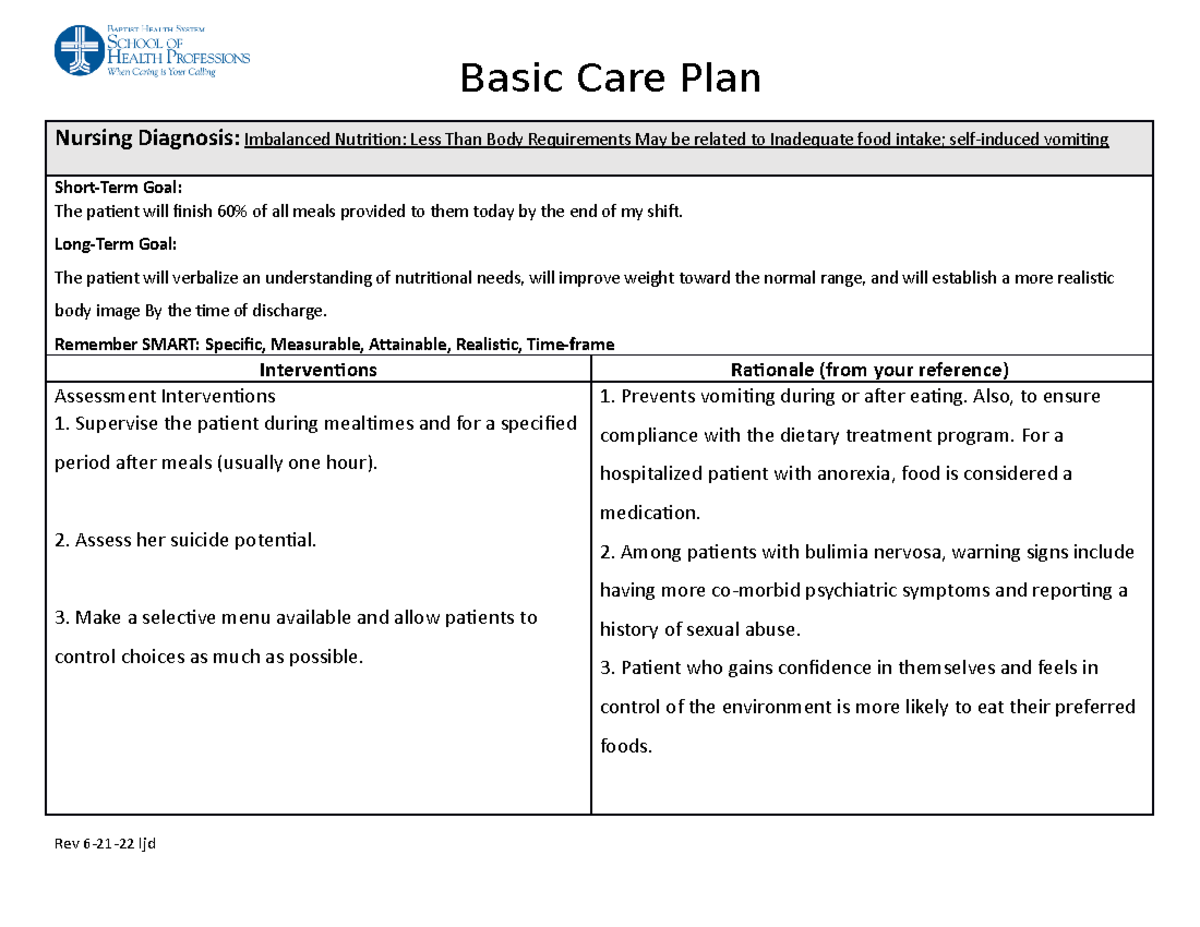
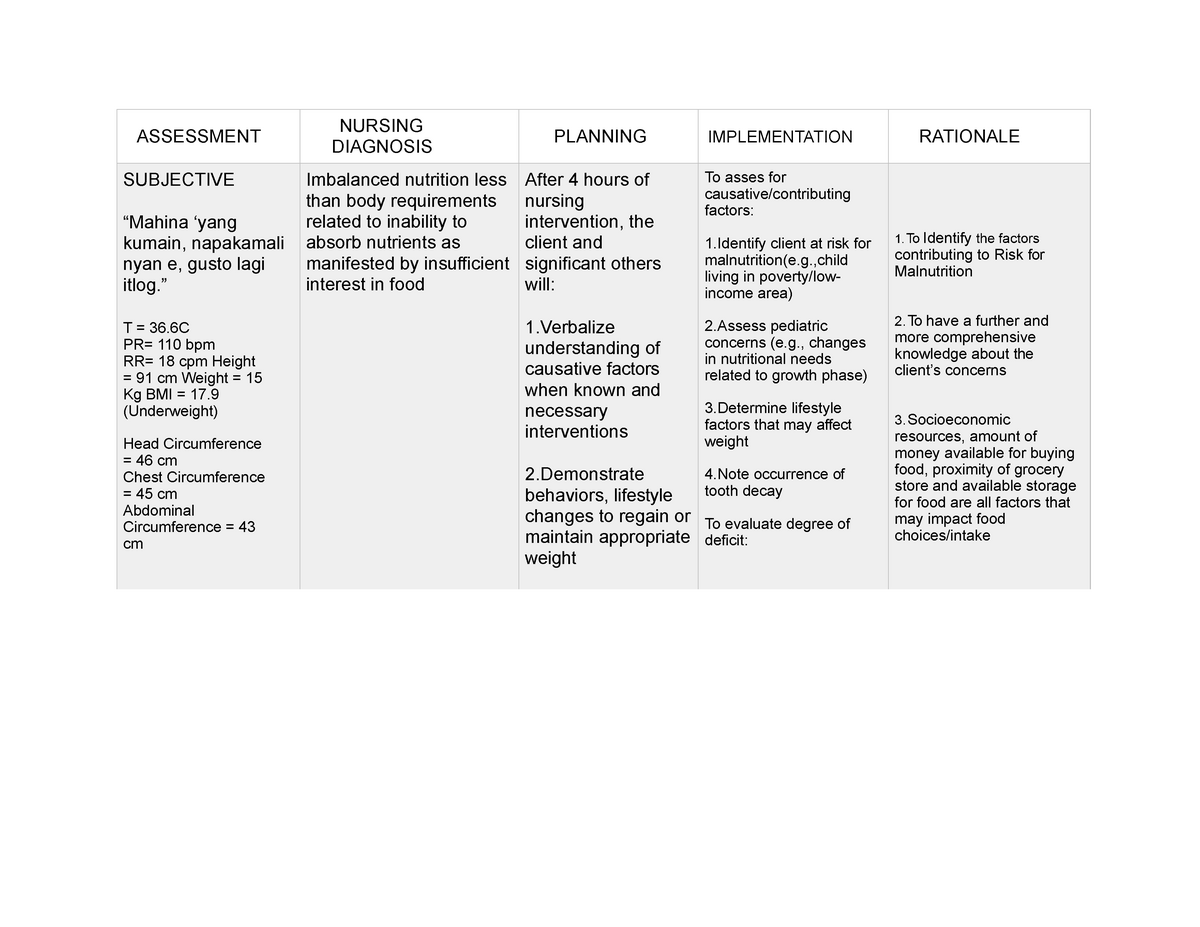
Assessment and Diagnosis
The first step is a thorough assessment of the patient's nutritional status. This typically involves a review of their medical history, dietary habits, physical examination, and laboratory tests.
Key indicators, such as weight loss, muscle wasting, and blood protein levels, are carefully evaluated to determine the severity of the nutritional deficit. The assessment also helps identify any underlying medical conditions contributing to the malnutrition.
Setting Goals and Objectives
Once a diagnosis is made, specific, measurable, achievable, relevant, and time-bound (SMART) goals are established. These goals might include weight gain, improved energy levels, enhanced wound healing, or reduced risk of infection.
The care plan outlines concrete steps to achieve these goals, taking into account the patient's individual preferences and limitations. Collaboration with the patient is crucial to ensure adherence to the plan.
Implementation Strategies
The implementation phase involves a multi-faceted approach. Dietary modifications are often a cornerstone, with tailored meal plans designed to meet the patient's specific nutritional requirements.
These plans may include increasing caloric intake, emphasizing protein-rich foods, and incorporating vitamin and mineral supplements. In some cases, enteral or parenteral nutrition, delivered through tubes or intravenously, may be necessary.
Furthermore, the care plan addresses any barriers to adequate nutrition, such as difficulty swallowing, nausea, or lack of appetite. Healthcare professionals provide education and support to help patients overcome these challenges.
"Effective nutritional care is not just about providing food; it's about understanding the individual's needs and tailoring the approach accordingly." - Dr. Emily Carter, Registered Dietitian.
Monitoring and Evaluation
Regular monitoring is essential to track the patient's progress and adjust the care plan as needed. This involves ongoing assessments of weight, appetite, energy levels, and laboratory values.
Any changes in the patient's condition are promptly addressed, and the care plan is modified to ensure continued effectiveness. The goal is to optimize nutritional intake and promote overall well-being.
The Role of the Healthcare Team
The "Imbalanced Nutrition Less Than Body Requirements" care plan requires a coordinated effort from a multidisciplinary team. Physicians oversee the medical aspects of the plan, while nurses provide direct patient care and monitor vital signs.
Registered dietitians play a critical role in developing and implementing individualized meal plans. Other healthcare professionals, such as speech therapists and occupational therapists, may be involved to address specific challenges related to eating and swallowing.
Family members and caregivers are also important members of the team, providing support and encouragement to the patient. Education and training are provided to ensure that they can effectively assist with the care plan at home.
Impact and Significance
Effective implementation of an "Imbalanced Nutrition Less Than Body Requirements" care plan can have a profound impact on patient outcomes. Improved nutritional status can lead to faster wound healing, reduced risk of infection, and increased energy levels.
It can also enhance the effectiveness of other medical treatments and improve overall quality of life. In some cases, nutritional support can even be life-saving, particularly for patients with severe malnutrition.
The cost-effectiveness of nutritional interventions has also been demonstrated in numerous studies. By preventing complications and reducing hospital readmissions, these care plans can ultimately lower healthcare costs.
Challenges and Future Directions
Despite its benefits, implementing an "Imbalanced Nutrition Less Than Body Requirements" care plan can be challenging. Factors such as limited resources, lack of awareness, and difficulty coordinating care can hinder its effectiveness.
Future directions in this field include developing more personalized and targeted nutritional interventions, utilizing technology to improve monitoring and communication, and promoting greater collaboration between healthcare providers.
Further research is also needed to better understand the complex interplay between nutrition, illness, and overall health. By investing in research and innovation, healthcare professionals can continue to improve the lives of patients with malnutrition.
In conclusion, the "Imbalanced Nutrition Less Than Body Requirements" care plan is a vital tool for addressing malnutrition and improving patient outcomes. Through careful assessment, individualized planning, and coordinated implementation, healthcare professionals can help patients achieve optimal nutritional status and enhance their overall well-being.