In Network Providers For Premera Blue Cross

Urgent action is needed for Premera Blue Cross members. Significant disruptions are occurring within Premera's network of in-network providers, impacting access to care and potentially increasing out-of-pocket costs.
This article provides a concise overview of the current situation, identifies the affected parties, details the scope of the provider network changes, and outlines steps Premera members can take to navigate these challenges and ensure continued access to affordable healthcare.
Understanding the Provider Network Changes
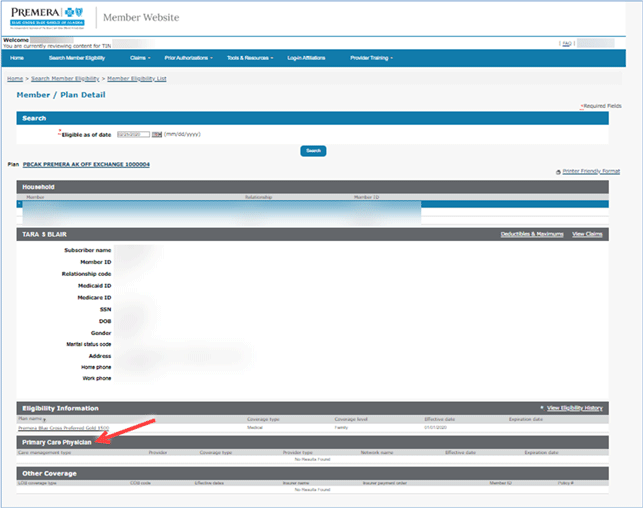
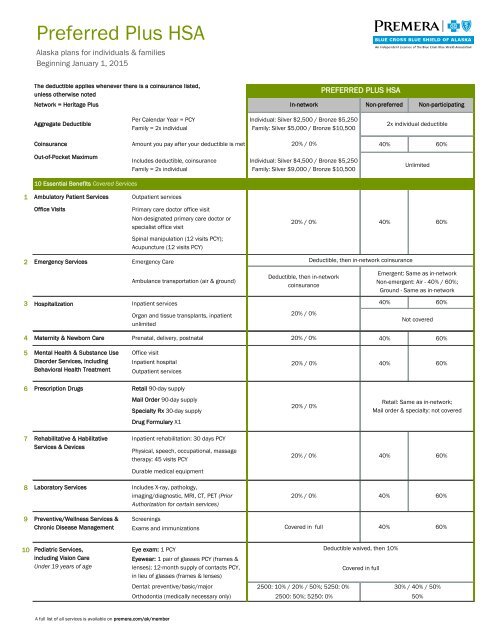
Premera Blue Cross is currently undergoing changes to its in-network provider list. The precise nature and extent of these changes vary depending on the specific plan and geographic location of the member.
Members are reporting difficulties confirming provider status. Many are finding that doctors and facilities previously listed as in-network are no longer participating, or that information available online is outdated and inaccurate.
Who is Affected?
The primary impact is on individuals and families covered by Premera Blue Cross plans. This includes those with individual, family, and employer-sponsored plans.
Specifically, residents of Washington and Alaska are most likely to be affected. Changes are also occurring in other regions where Premera operates.
What Services Are Impacted?
Reports indicate that a wide range of services are experiencing network disruptions. This includes primary care physicians, specialists, mental health providers, and hospitals.
Some members are also reporting issues with access to urgent care facilities. This broad impact is raising concerns about timely access to necessary medical care.
Where and When Are These Changes Happening?
The network changes are occurring throughout Premera's service areas, with noticeable impacts in major metropolitan areas. There is no single geographic area spared from the issues.
These changes have been unfolding over the past few months. Many members are only now becoming aware of the extent of the disruptions as they attempt to schedule appointments.
How to Navigate the Network Changes
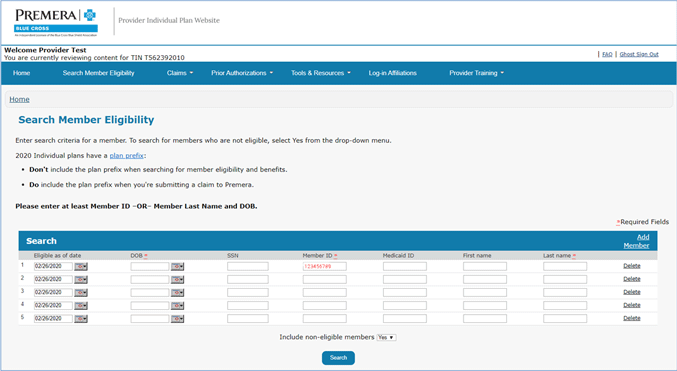
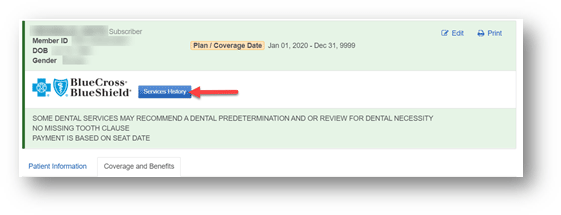
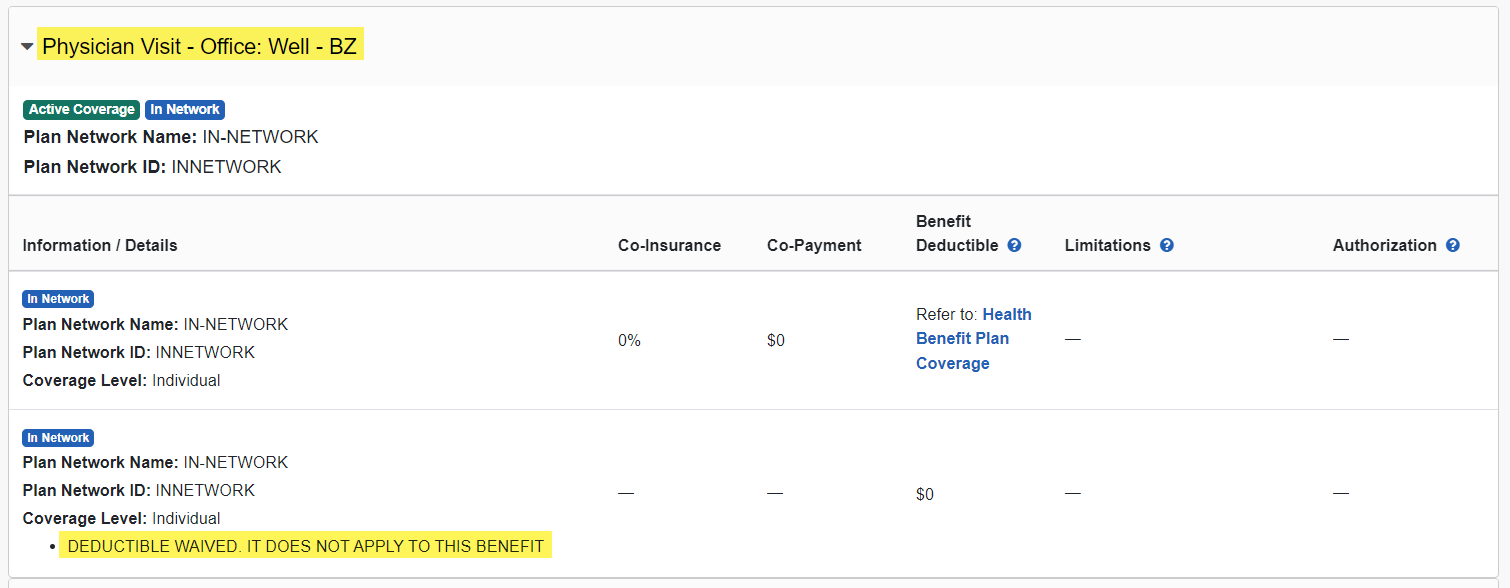
It is crucial for Premera members to proactively verify the network status of their healthcare providers. Do not assume that a provider listed as in-network in the past remains in-network.
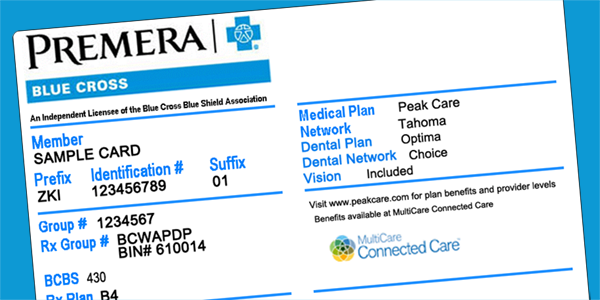
Contact Premera Blue Cross directly to confirm your provider's current status. Use the customer service number listed on your insurance card or access the online provider directory on the Premera website.
Request written confirmation of network status from both Premera and your provider's office. This documentation can be vital if billing disputes arise later.
Utilizing Premera's Resources
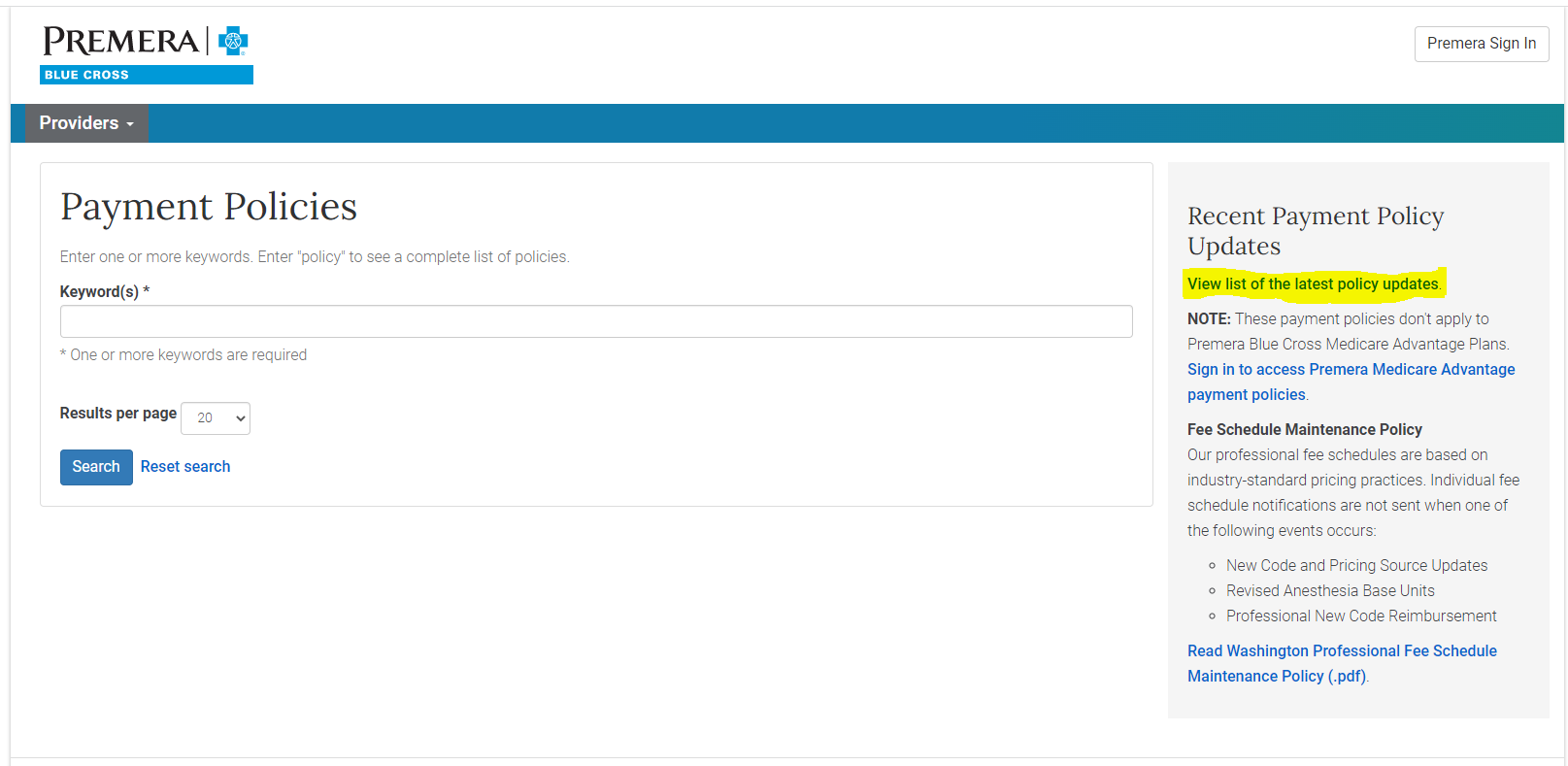
Familiarize yourself with Premera's online resources for finding in-network providers. However, be aware that the online directory may not be entirely up-to-date.
Take advantage of Premera's customer service representatives. They can assist with provider searches and address specific questions about your plan's coverage.
"Members should not hesitate to escalate concerns to Premera's management if they encounter persistent difficulties in finding in-network care," advises healthcare advocate Sarah Miller.
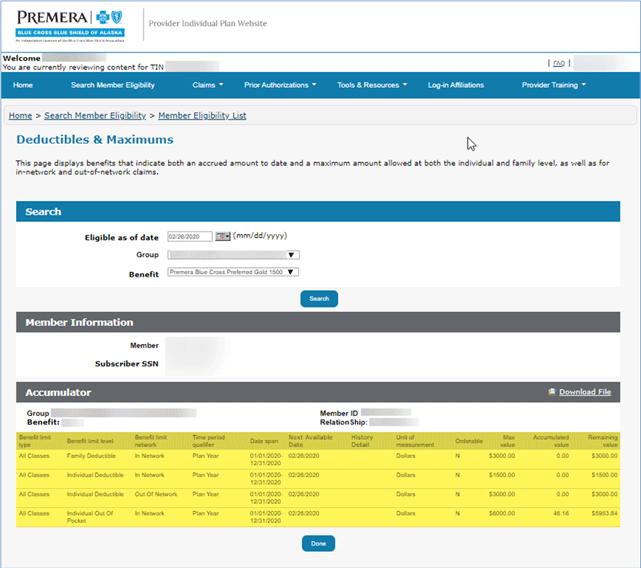
Understanding Out-of-Network Costs
Be aware of the potential for increased out-of-pocket costs if you receive care from an out-of-network provider. Carefully review your plan's out-of-network benefits.
If you are forced to see an out-of-network provider due to a lack of in-network options, consider appealing to Premera for an exception or reduced cost-sharing.
Addressing the Problem: Advocacy and Next Steps
If you are experiencing significant difficulties accessing in-network care, consider filing a formal complaint with Premera Blue Cross. Document all communication and interactions related to the issue.
Contact your state's insurance commissioner to report the problem. State regulators can investigate potential violations of network adequacy requirements.
Engage with consumer advocacy groups and share your experiences. Collective action can help to raise awareness and pressure Premera to address the network disruptions.
Ongoing monitoring of Premera's provider network is essential. Members should remain vigilant and proactive in verifying provider status and advocating for access to affordable healthcare. Further updates will be provided as more information becomes available.