Intrathecal Injection Is Administered Into The
A precise, yet potentially fraught procedure, intrathecal injection carries profound implications for pain management, neurological disorders, and even cancer treatment. This method of drug delivery bypasses many of the body's natural barriers, offering direct access to the central nervous system. However, the inherent risks demand meticulous technique and a thorough understanding of potential complications.
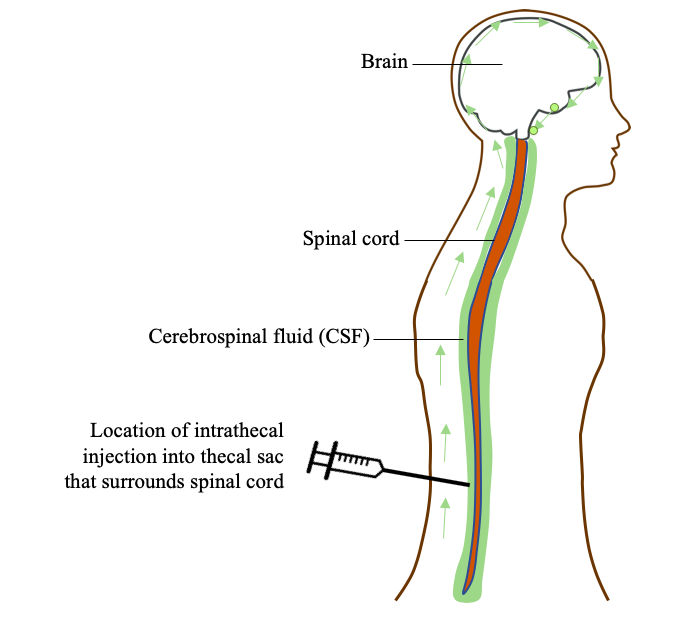
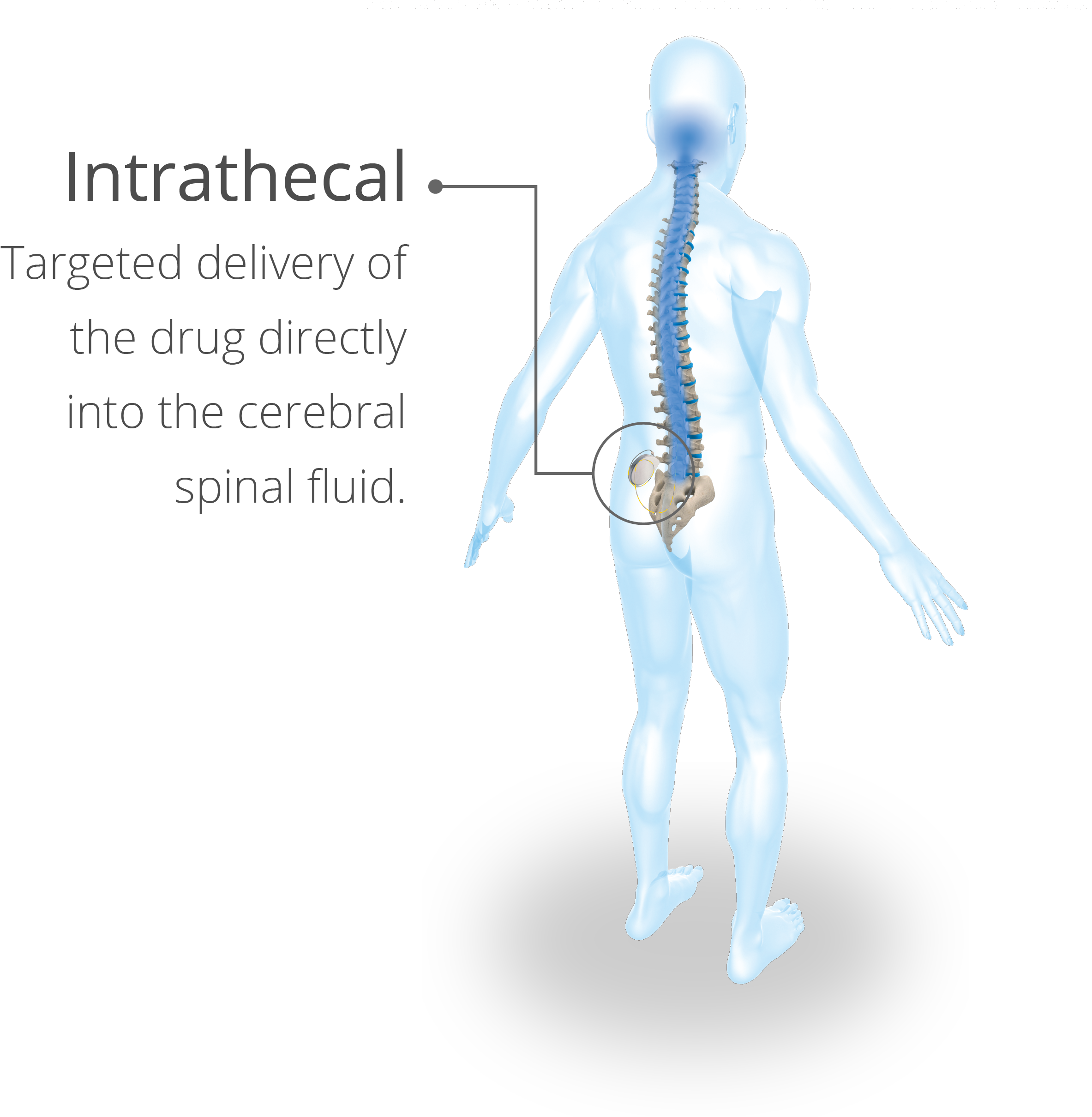
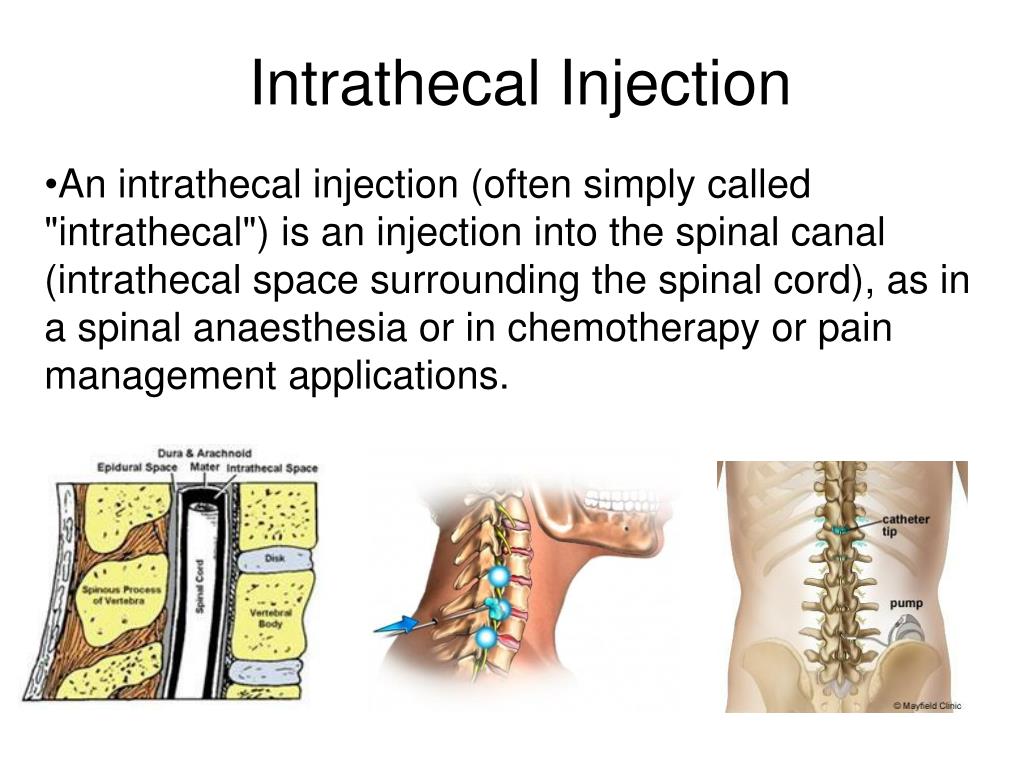
Intrathecal injection, the administration of medication directly into the cerebrospinal fluid (CSF) surrounding the spinal cord, stands as a powerful tool in modern medicine. This article delves into the intricacies of this procedure, exploring its applications, benefits, risks, and the future directions shaping its role in patient care. It examines the science underpinning intrathecal drug delivery, the clinical contexts where it proves most valuable, and the critical considerations that guide its safe and effective implementation.
Understanding the Procedure
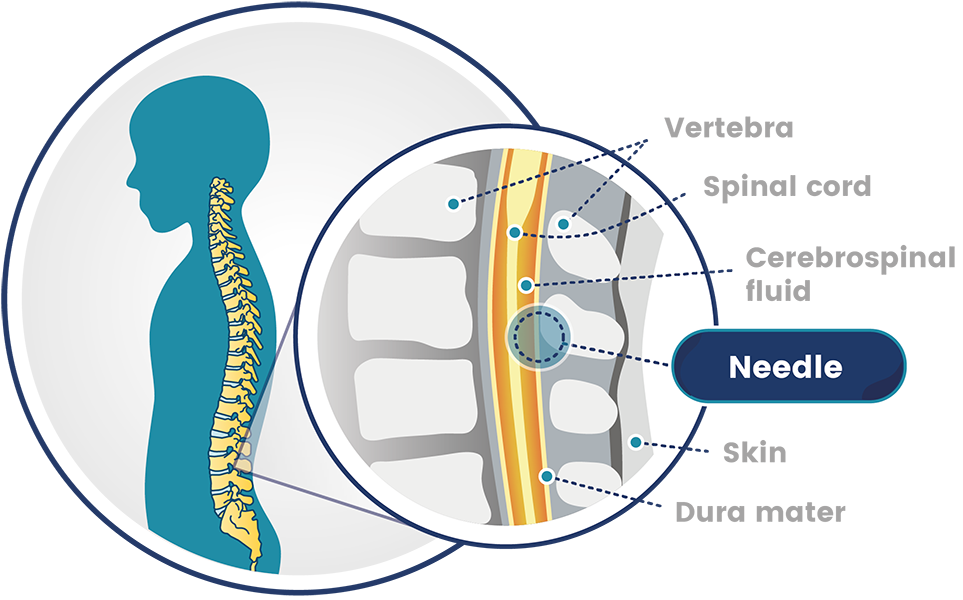
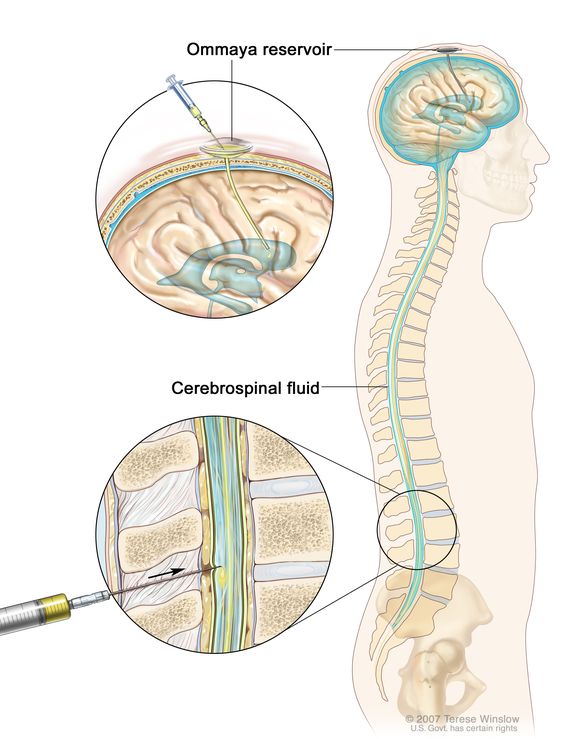
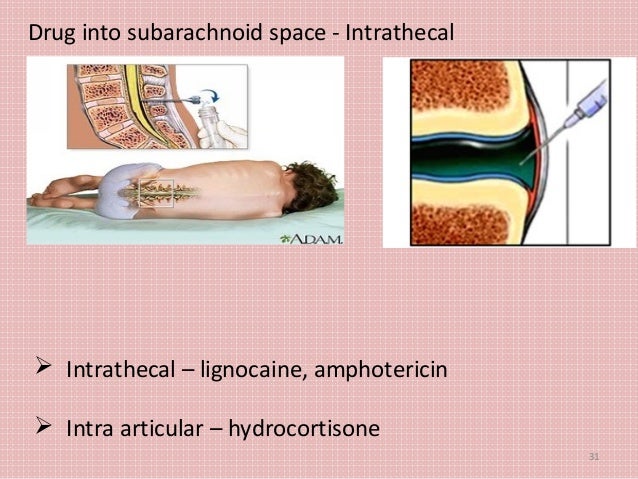
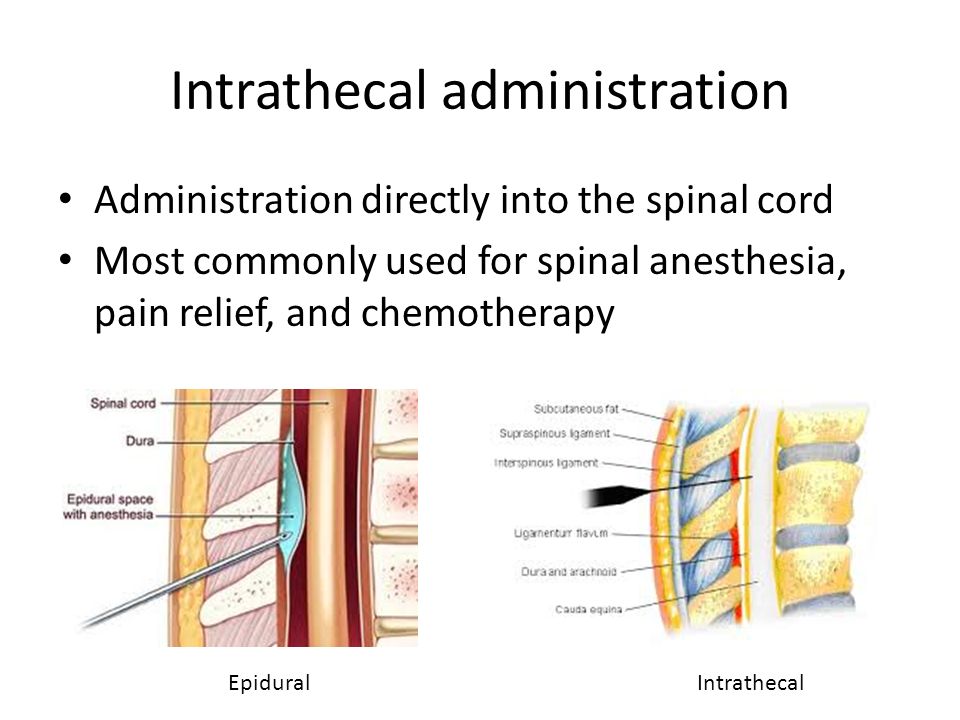
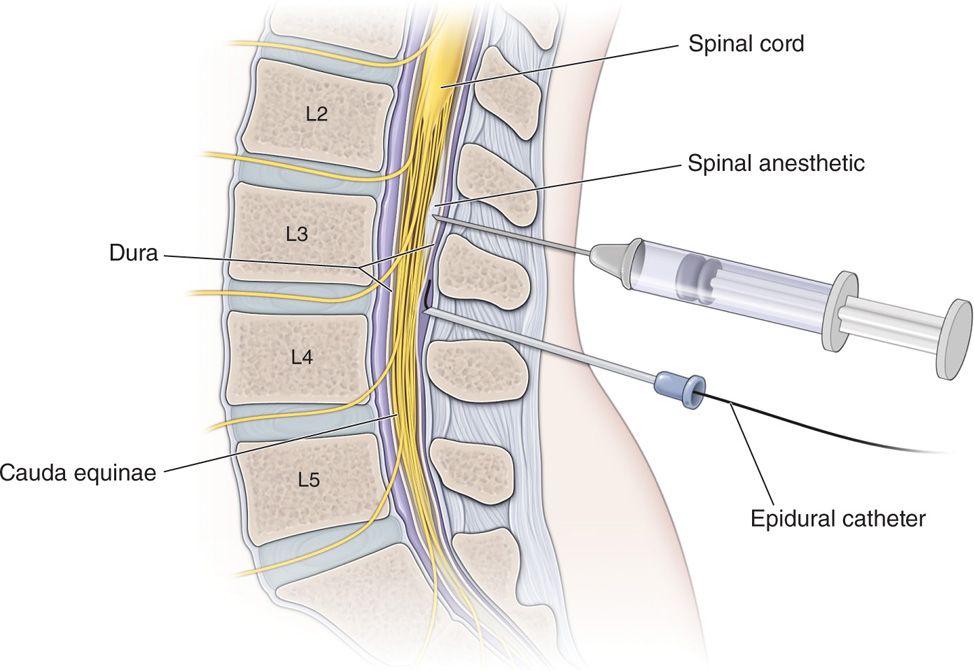
The procedure involves inserting a needle into the subarachnoid space, the fluid-filled area surrounding the spinal cord. This space is located between the arachnoid mater and pia mater, two of the protective membranes that cover the brain and spinal cord.
Typically performed by physicians with specialized training, such as anesthesiologists, neurologists, or pain management specialists, intrathecal injection requires careful patient positioning and meticulous technique. Fluoroscopy, a type of real-time X-ray imaging, is often used to guide needle placement and ensure accurate drug delivery.
Prior to the injection, the patient is typically positioned in a seated or lateral decubitus (lying on their side) position. The skin is then cleansed with an antiseptic solution to minimize the risk of infection.
Key Considerations for Safe Practice
Strict adherence to sterile technique is paramount to prevent infection, a serious complication that can lead to meningitis or other neurological problems. Proper needle placement is crucial to avoid spinal cord injury or nerve damage.
Careful patient selection is essential, as not all individuals are suitable candidates for intrathecal injection. A thorough medical history and physical examination are necessary to assess potential risks and benefits.
The choice of medication and dosage must be carefully considered based on the patient's condition and individual response. Close monitoring of the patient's vital signs and neurological status is required during and after the procedure.
Clinical Applications and Benefits
Intrathecal injection is used to treat a variety of conditions, including chronic pain, spasticity, and certain types of cancer. Its ability to deliver medication directly to the central nervous system allows for lower doses and potentially fewer systemic side effects compared to oral or intravenous administration.
For chronic pain management, intrathecal drug delivery systems (IDDS), also known as pain pumps, can provide long-term relief for patients who have not responded to other treatments. These systems typically involve implanting a pump under the skin that continuously delivers medication, such as opioids or local anesthetics, into the intrathecal space.
In patients with severe spasticity, often caused by conditions such as cerebral palsy or multiple sclerosis, intrathecal baclofen can significantly reduce muscle stiffness and improve motor function. This can lead to enhanced mobility, reduced pain, and improved quality of life.
Intrathecal chemotherapy is sometimes used to treat certain types of cancer that have spread to the brain or spinal cord, such as leukemia or lymphoma. This allows for higher concentrations of chemotherapy drugs to reach the cancer cells while minimizing exposure to the rest of the body.
Risks and Potential Complications
While intrathecal injection can offer significant benefits, it is not without risks. Headache is a common side effect, often caused by leakage of cerebrospinal fluid (CSF) from the puncture site. This is known as a postdural puncture headache (PDPH).
Other potential complications include infection, bleeding, nerve damage, and allergic reactions to the medication. In rare cases, more serious complications such as arachnoiditis (inflammation of the arachnoid membrane) or spinal cord injury can occur.
The risk of complications can be minimized by careful patient selection, meticulous technique, and close monitoring of the patient's condition. It is crucial for patients to be fully informed of the potential risks and benefits before undergoing the procedure.
"Patient safety is paramount," emphasizes Dr. Anya Sharma, a leading pain management specialist. "Thorough evaluation and informed consent are essential to ensure the best possible outcomes with intrathecal injections."
The Future of Intrathecal Drug Delivery
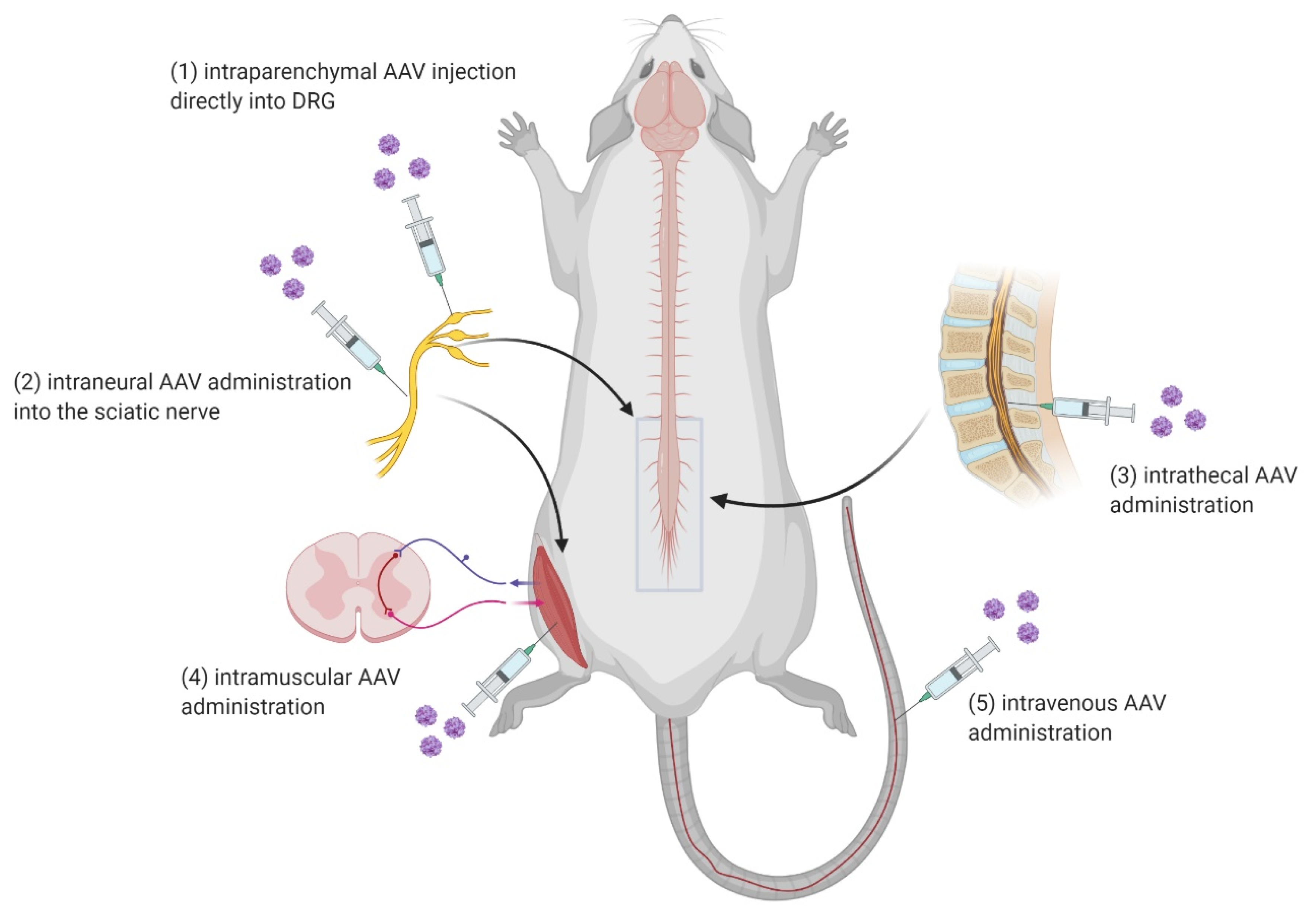
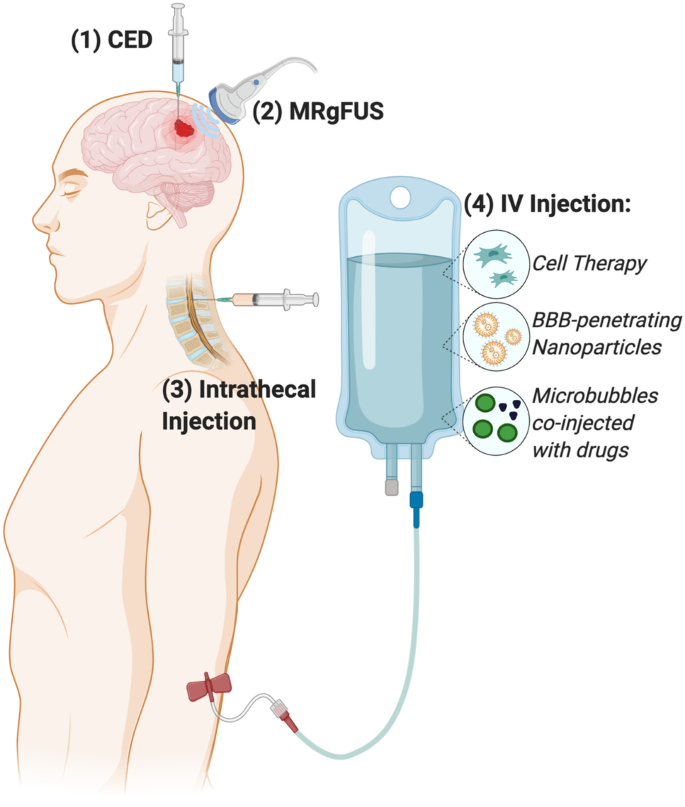
Research is ongoing to develop new and improved intrathecal drug delivery systems and therapies. This includes the development of more targeted medications that can selectively act on specific areas of the central nervous system.
Advances in nanotechnology are also being explored to create drug carriers that can deliver medication more efficiently and effectively to the target site. These nano-carriers could potentially improve drug penetration, reduce side effects, and prolong the duration of action.
Furthermore, researchers are investigating the potential of using gene therapy to deliver therapeutic genes directly to the spinal cord via intrathecal injection. This could offer a long-term solution for certain neurological disorders and chronic pain conditions.
Intrathecal injection represents a significant advancement in the treatment of various medical conditions. As technology and research continue to evolve, this method of drug delivery holds great promise for improving the lives of patients suffering from chronic pain, neurological disorders, and cancer.
The ongoing refinements in technique, medication, and delivery systems are poised to further enhance the safety and efficacy of this powerful therapeutic tool. However, careful patient selection, meticulous execution, and continuous monitoring will remain the cornerstones of responsible intrathecal injection practice.
Ultimately, the successful application of this procedure hinges on a multidisciplinary approach, involving collaboration between physicians, pharmacists, nurses, and other healthcare professionals to ensure optimal patient care.







.jpg)
