List Three Effects Of The Complement System
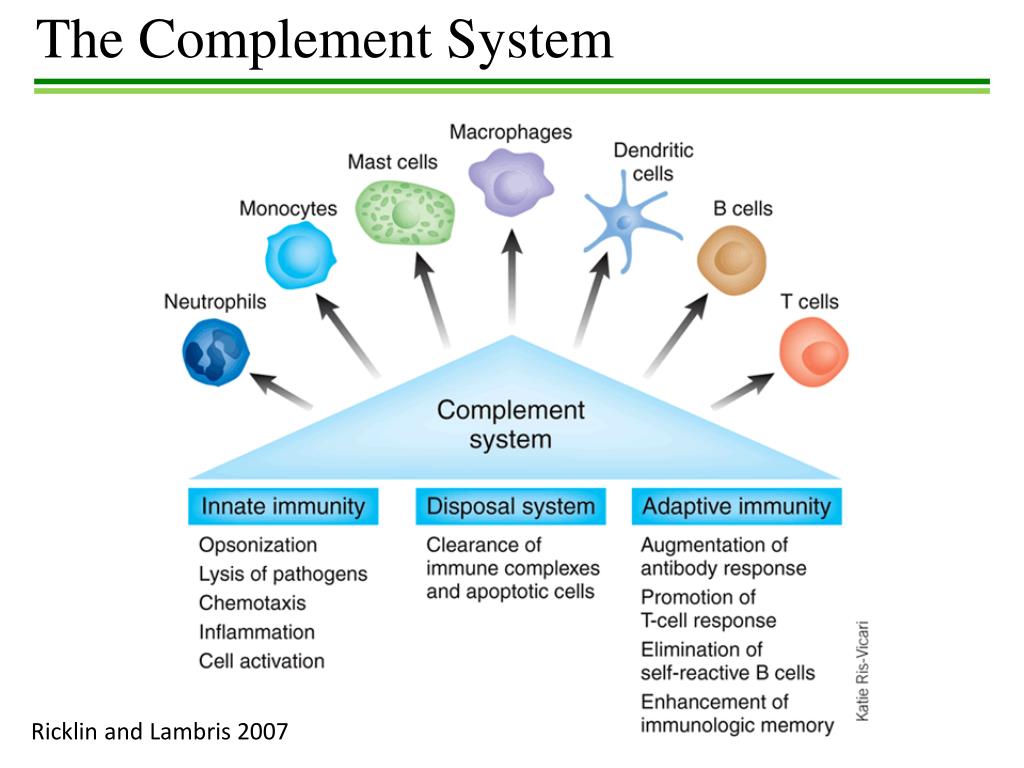
The complement system, a crucial part of the innate immune system, plays a significant role in defending the body against pathogens. It is a complex network of proteins that work together to identify and eliminate threats. While its primary function is to protect against infection, its effects extend beyond simple pathogen destruction.
Understanding the multifaceted impacts of the complement system is vital for comprehending immune responses and developing effective therapeutic strategies. It's not just about killing bacteria; its activities shape inflammation, immune cell behavior, and even tissue homeostasis.
Three Key Effects of the Complement System
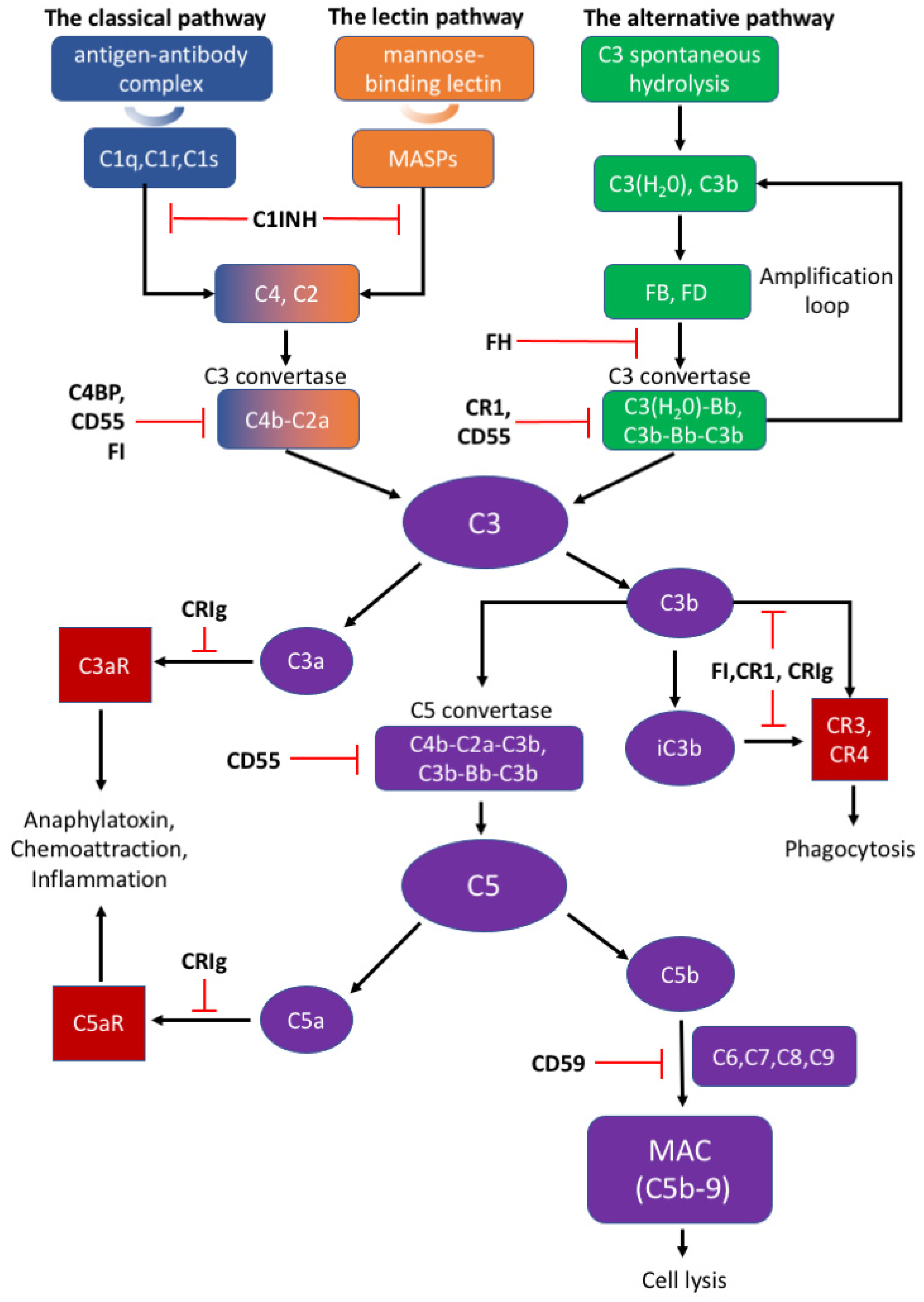
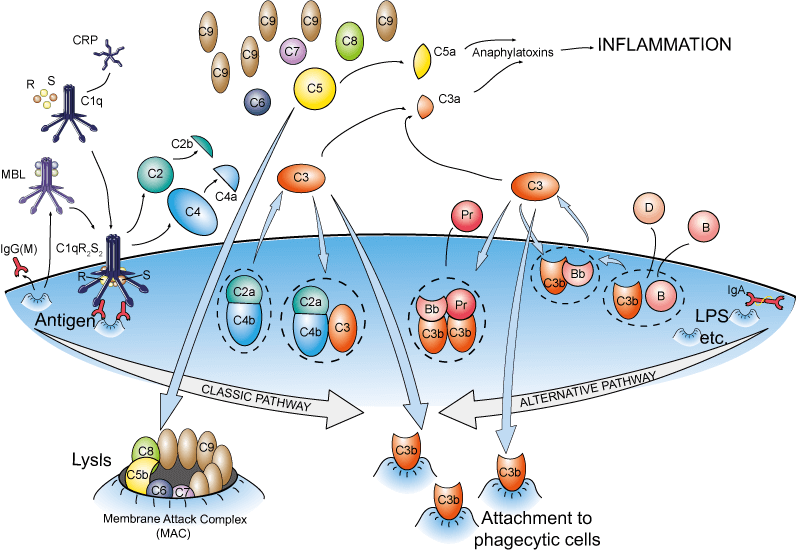
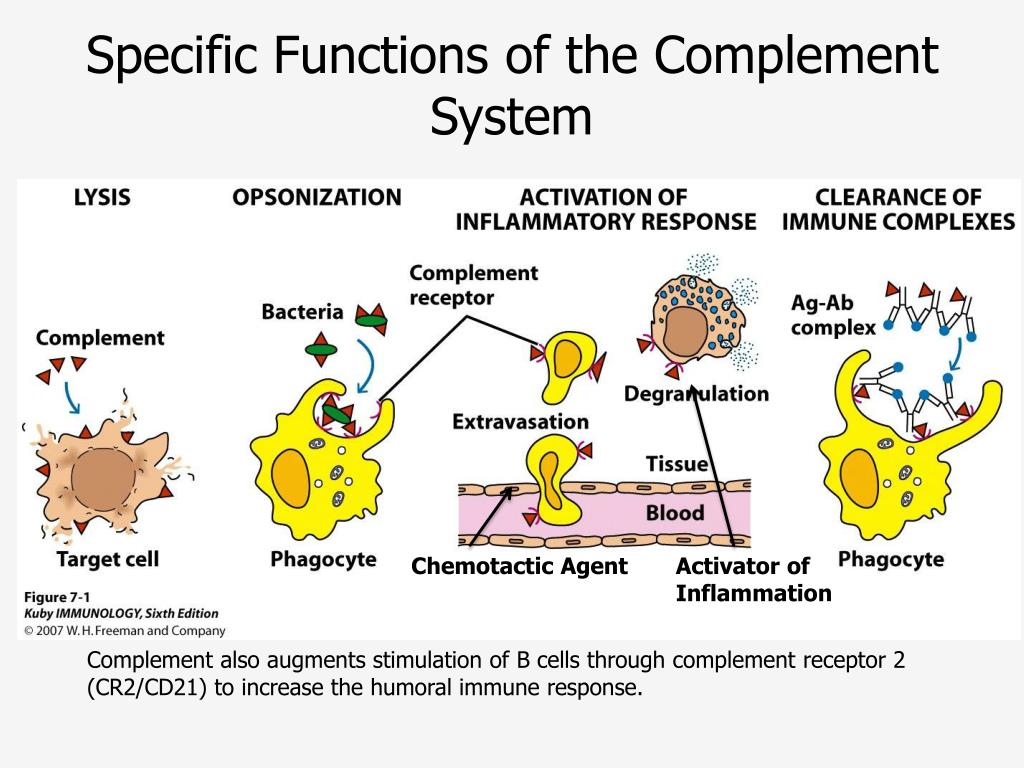
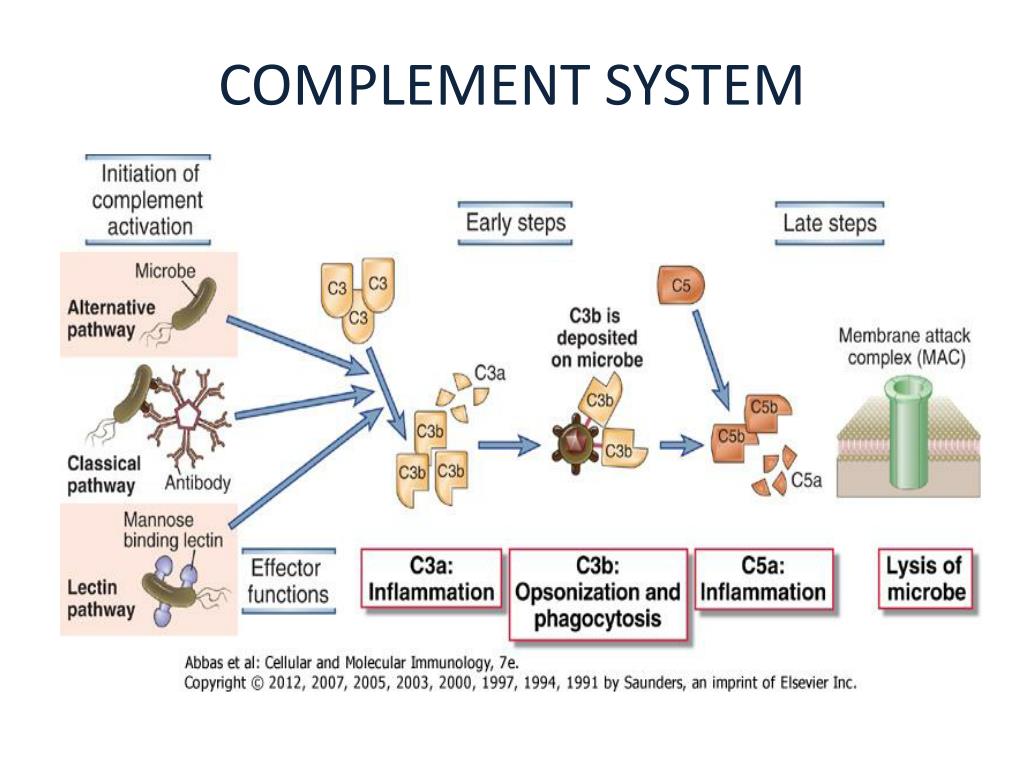
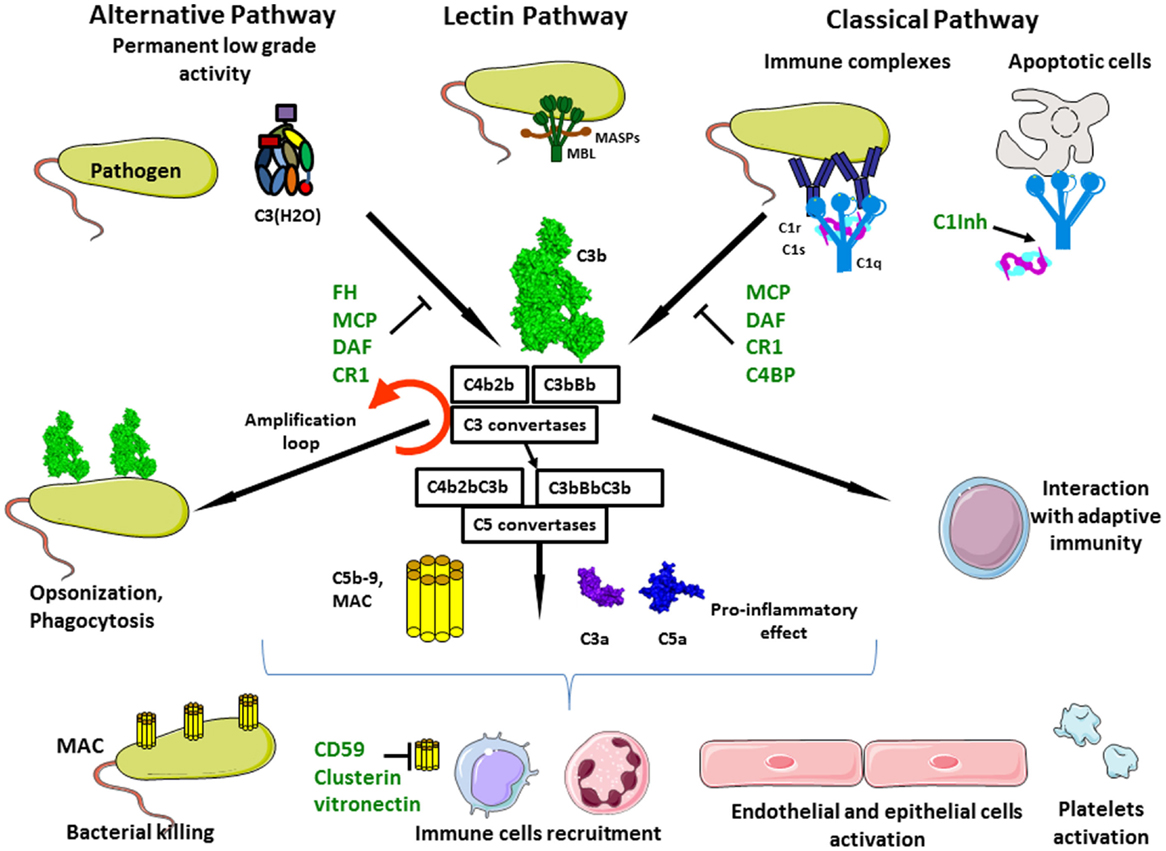
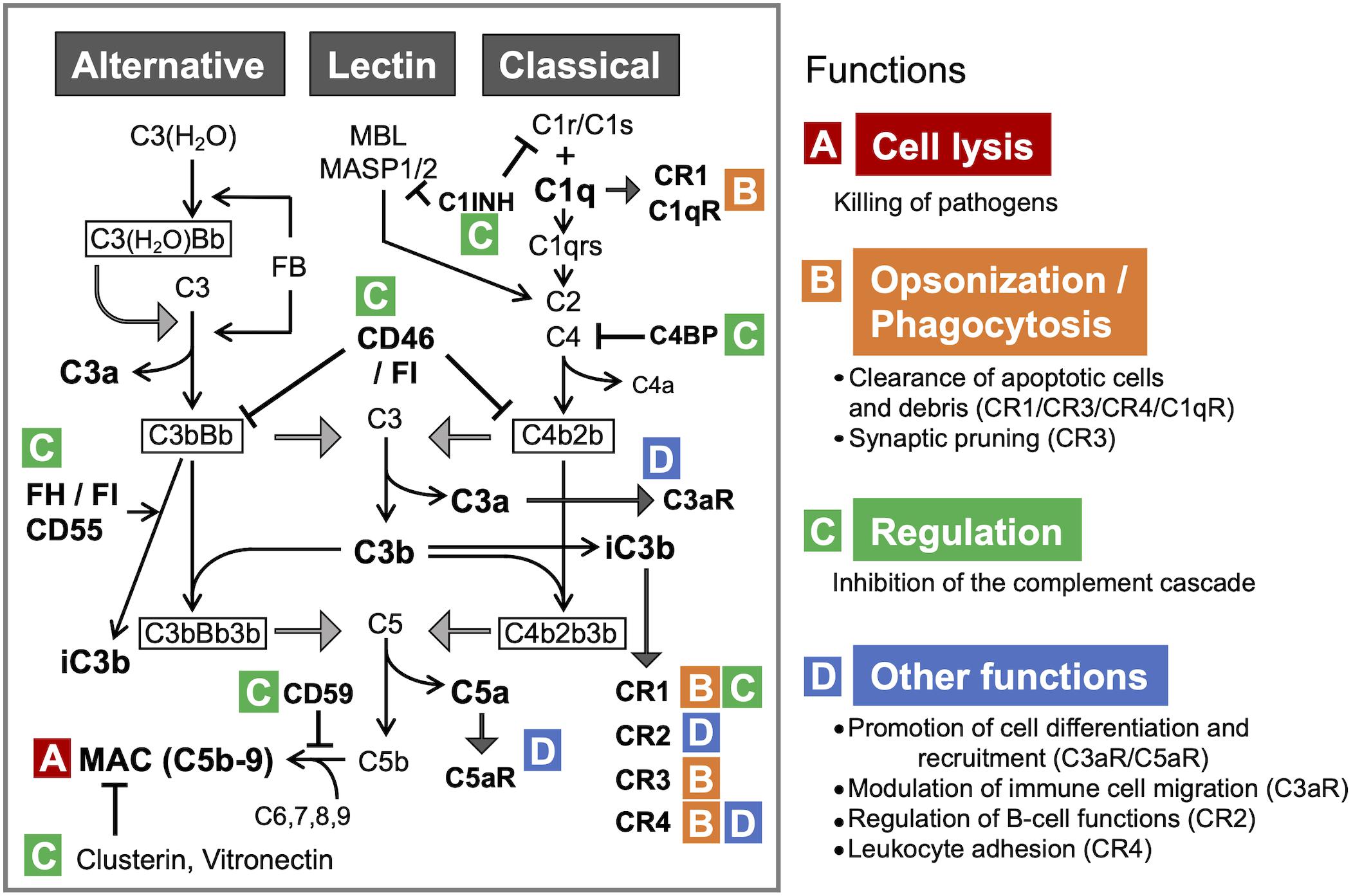
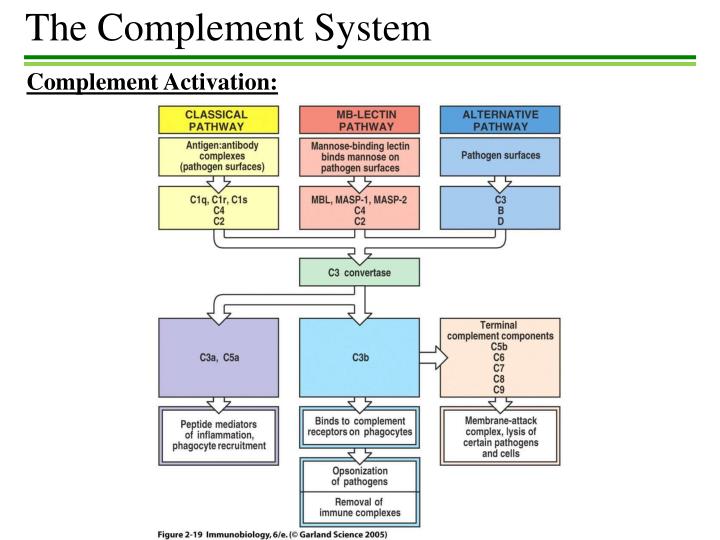
The complement system's activities can be broadly categorized into three major effects: opsonization, inflammation, and direct cytolysis. Each of these processes involves a cascade of protein interactions, leading to distinct outcomes that contribute to overall immune defense.
1. Opsonization: Enhancing Phagocytosis
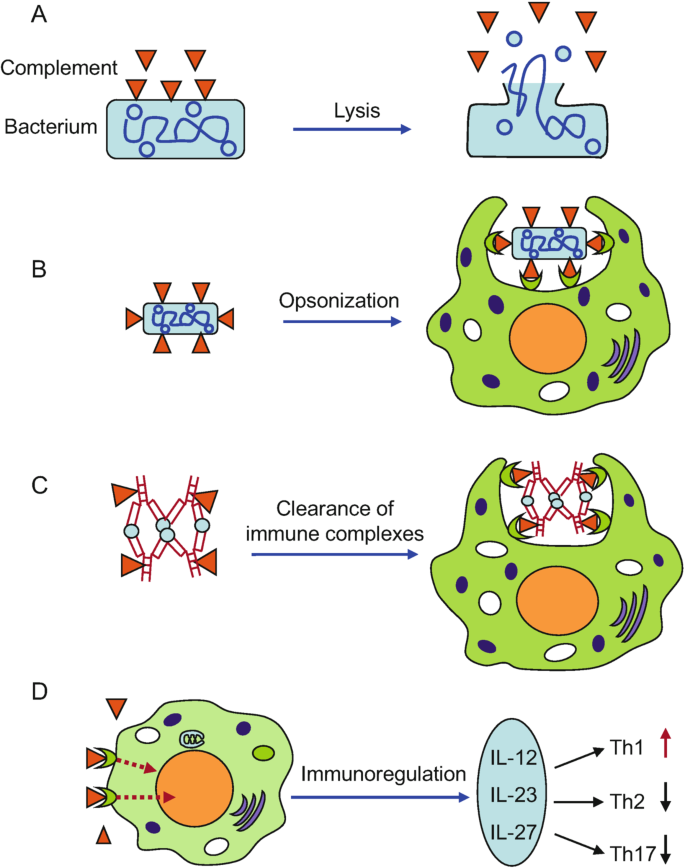
Opsonization is the process by which pathogens are coated with molecules that enhance their recognition and engulfment by phagocytes. Complement proteins, particularly C3b, act as potent opsonins.
When C3b binds to the surface of a pathogen, it acts like a flag, signaling to phagocytic cells like macrophages and neutrophils. These phagocytes have receptors that specifically recognize C3b, allowing them to efficiently bind to and internalize the pathogen.
This enhanced phagocytosis is critical for clearing infections. Without opsonization, pathogens might evade phagocytes, allowing them to replicate and spread.
2. Inflammation: Recruiting Immune Cells and Promoting Tissue Repair
The complement system plays a crucial role in initiating and amplifying inflammatory responses. Certain complement fragments, known as anaphylatoxins (C3a, C5a), act as potent chemoattractants, drawing immune cells to the site of infection or tissue damage.
C5a, in particular, is a powerful chemoattractant for neutrophils, the first responders to infection. It also activates mast cells, leading to the release of histamine and other inflammatory mediators.
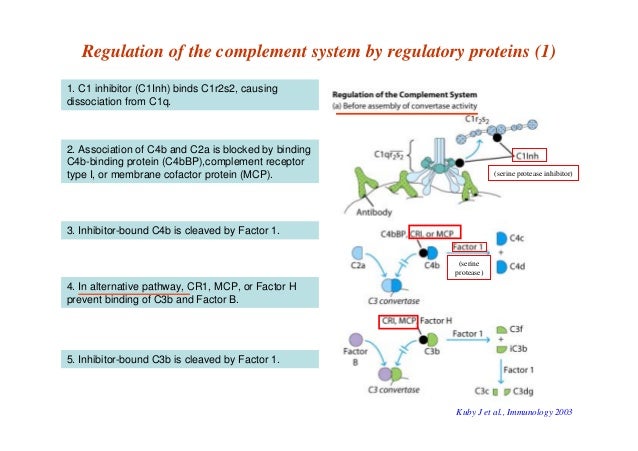
While inflammation is essential for clearing pathogens and initiating tissue repair, excessive or uncontrolled complement-mediated inflammation can contribute to tissue damage and chronic inflammatory diseases. Therefore, the complement system must be tightly regulated to prevent collateral damage.
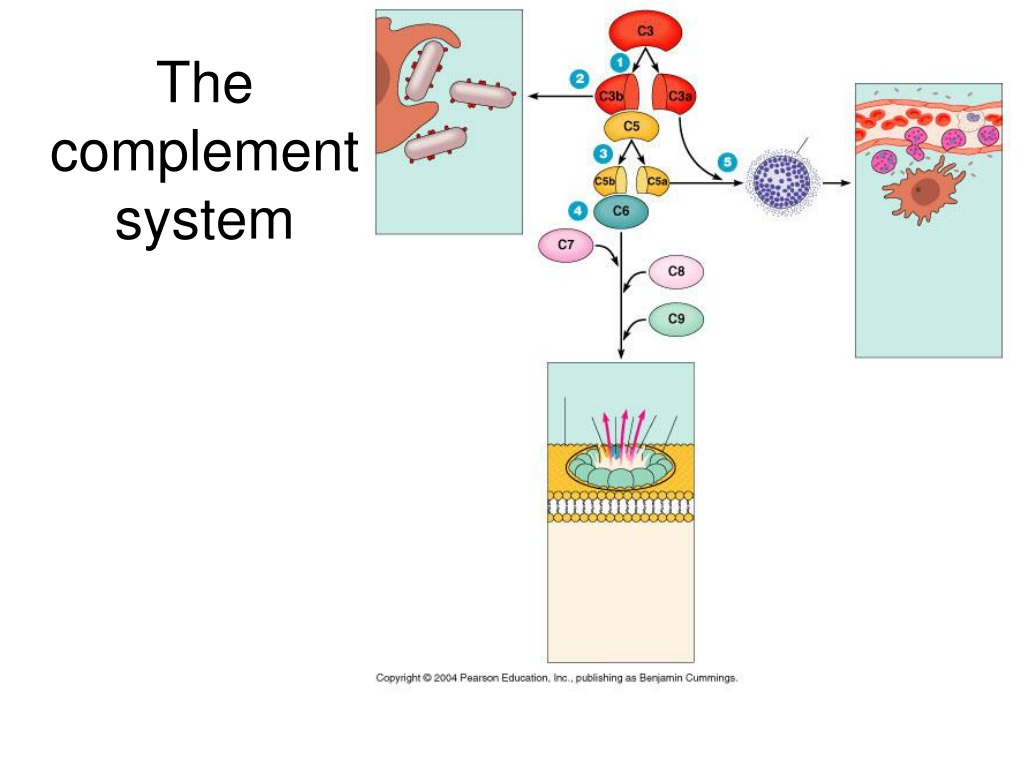
3. Direct Cytolysis: Membrane Attack Complex (MAC) Formation
The complement system can directly kill pathogens through the formation of the Membrane Attack Complex (MAC). This complex is formed by the assembly of several complement proteins (C5b, C6, C7, C8, and C9) on the surface of the pathogen.
The MAC inserts itself into the pathogen's cell membrane, creating a pore that disrupts the membrane's integrity. This leads to an influx of water and ions, ultimately causing the cell to lyse and die.
The MAC is particularly effective against bacteria with thin cell walls, such as Neisseria species. However, the MAC can also damage host cells, so its activity is carefully controlled by regulatory proteins.
Significance and Impact
The complement system's effects are far-reaching. Its involvement in opsonization, inflammation, and cytolysis highlights its central role in immunity and homeostasis.
Dysregulation of the complement system has been implicated in a wide range of diseases, including autoimmune disorders, inflammatory conditions, and neurodegenerative diseases. For example, excessive complement activation contributes to the pathogenesis of systemic lupus erythematosus (SLE) and rheumatoid arthritis.
Furthermore, complement deficiencies can increase susceptibility to infection, particularly by encapsulated bacteria. Understanding the intricacies of the complement system is therefore crucial for developing targeted therapies for these diseases.
Therapeutic Implications
The complement system is an attractive target for therapeutic intervention. Several drugs are currently in development or already approved that target specific components of the complement cascade.
For example, eculizumab is a monoclonal antibody that inhibits C5, preventing the formation of C5a and the MAC. It is used to treat paroxysmal nocturnal hemoglobinuria (PNH) and atypical hemolytic uremic syndrome (aHUS), both conditions characterized by excessive complement activation.
Other complement inhibitors are being developed for a variety of diseases, including age-related macular degeneration (AMD) and organ transplantation. By selectively modulating complement activity, it may be possible to treat a wide range of diseases while minimizing side effects.
Conclusion
The complement system is a powerful and versatile component of the immune system. Its effects extend beyond simple pathogen destruction, influencing inflammation, immune cell behavior, and tissue homeostasis.
Understanding the multifaceted impacts of the complement system is critical for comprehending immune responses and developing effective therapeutic strategies. Further research into this complex system will undoubtedly lead to new insights into the pathogenesis of disease and the development of novel therapies.


70167-8/asset/1c8b2064-f6e3-4577-ab7b-561590fb0e59/main.assets/gr1_lrg.jpg)