Medicare Progress Note Every 30 Days Or 10 Visits

A new mandate impacting Medicare providers requires that progress notes be documented at least every 30 days or after every 10 visits, whichever comes first. The policy shift, aimed at enhancing oversight and ensuring quality of care, has sparked debate among healthcare professionals regarding its potential benefits and burdens.
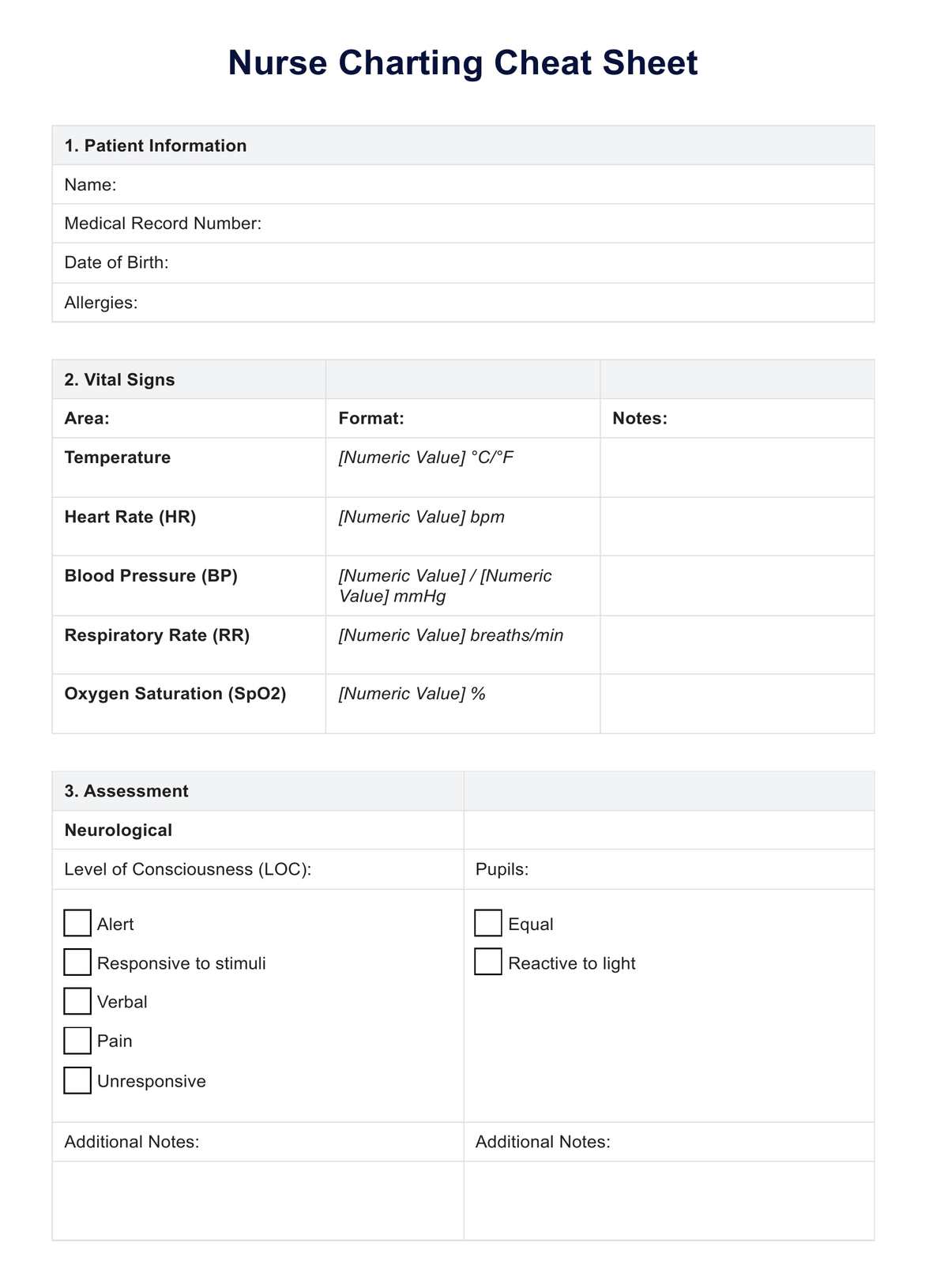
This policy change is poised to significantly affect how Medicare providers, including physicians, therapists, and other healthcare professionals, document and manage patient care. The increased frequency of progress note documentation is intended to improve care coordination, provide better tracking of patient progress, and ensure compliance with Medicare regulations.
The New Requirement: Details and Scope
The requirement stipulates that a Medicare progress note must be completed either every 30 days or after every 10 patient visits, whichever occurs sooner. This applies to a wide range of outpatient services covered by Medicare Part B, impacting numerous healthcare settings.
The Centers for Medicare & Medicaid Services (CMS) has stated that the new rule seeks to bolster transparency and accountability within the Medicare system. It aims to ensure that patient progress is regularly assessed and documented, allowing for timely adjustments to treatment plans when necessary.
Rationale Behind the Change
CMS argues that more frequent progress notes will lead to better continuity of care. Regularly updated records can facilitate smoother transitions between providers and improve communication amongst the care team.
Furthermore, the increased documentation is intended to help identify potential issues or concerns early on. This might include a lack of progress, adverse reactions to treatment, or the need for additional services.
CMS also highlights the potential for enhanced fraud detection. Consistent and detailed documentation can make it easier to identify billing irregularities or instances of inappropriate service provision.
Provider Perspectives and Concerns
The new mandate has elicited mixed reactions from healthcare providers. While some acknowledge the potential benefits, others express concerns about the additional administrative burden.
Many providers worry that the increased documentation requirements will take time away from direct patient care. The extra paperwork could lead to decreased efficiency and increased administrative costs.
Some fear that the focus on documentation may overshadow the importance of clinical judgment. Providers might feel pressured to adhere to rigid templates, potentially hindering their ability to tailor care to individual patient needs.
"While we understand the need for accountability, we are concerned about the potential impact on our ability to provide timely and effective care," said Dr. Emily Carter, a primary care physician in a rural clinic. "The additional administrative burden could stretch our resources thin."
Smaller practices and solo practitioners may face particular challenges. These providers often lack the administrative support necessary to manage the increased documentation workload effectively.
Impact on Patients
The impact on patients is expected to be multifaceted. Proponents argue that patients will benefit from improved care coordination and more personalized treatment plans.
However, some worry that the increased administrative burden on providers could lead to longer wait times for appointments. If providers are spending more time on documentation, they may have less time available to see patients.
There is also concern that the emphasis on documentation could create a less personal patient-provider relationship. The focus on ticking boxes might detract from the human element of care.
Preparing for the Change
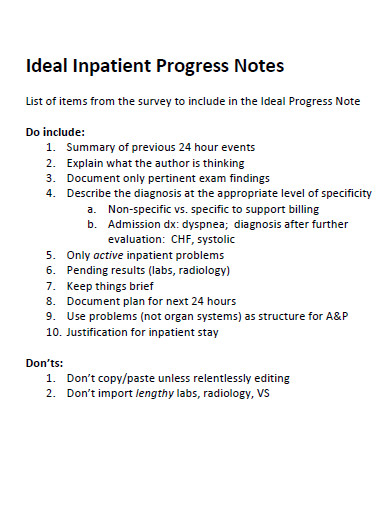
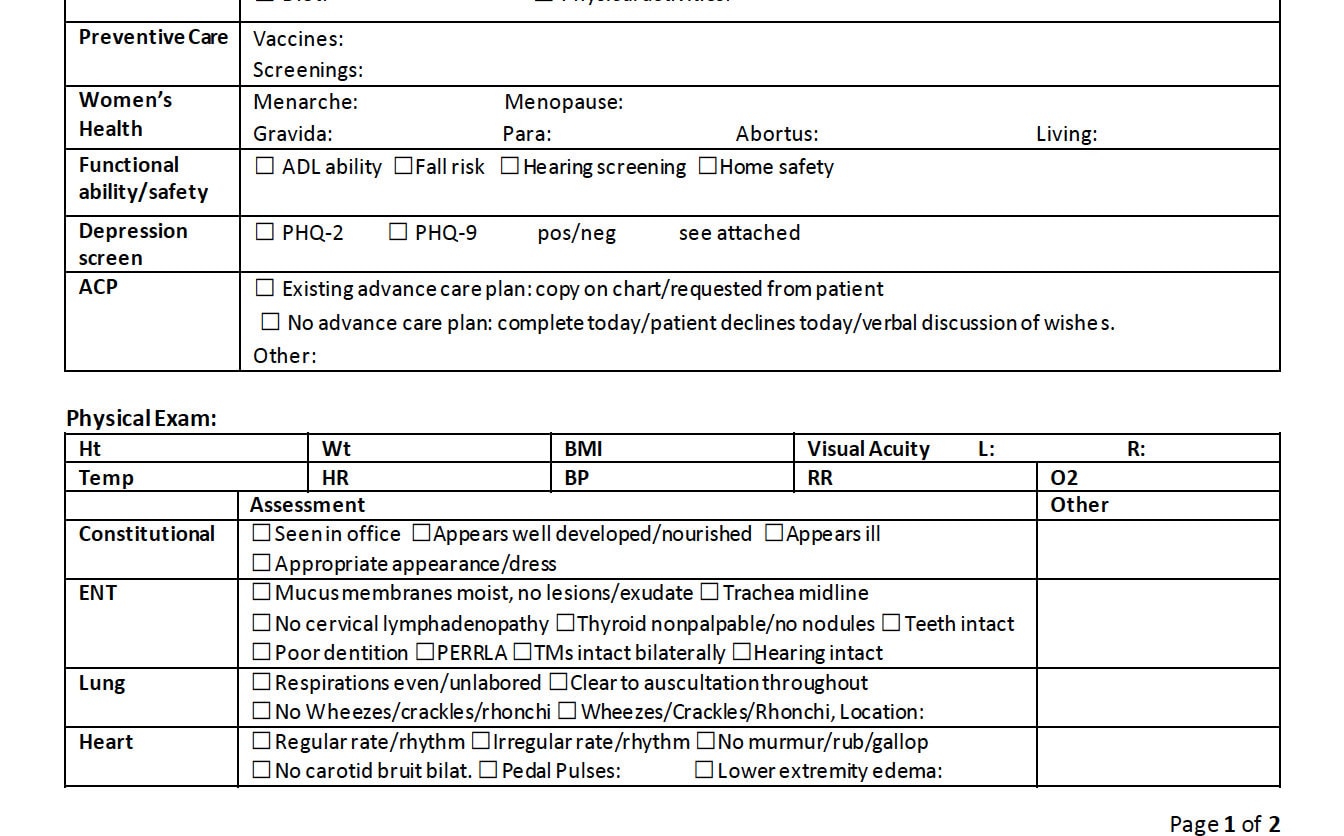
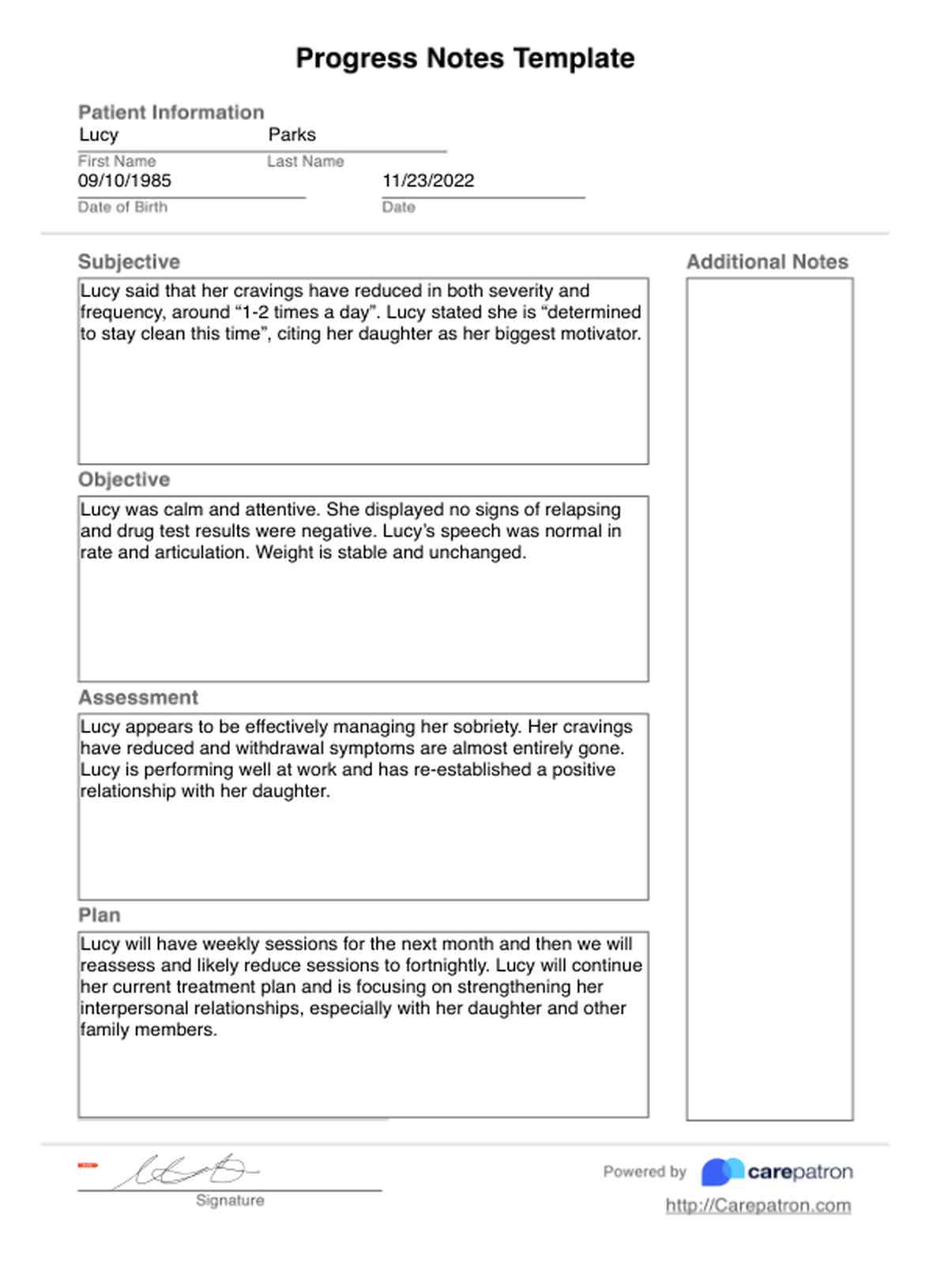
Healthcare providers are advised to familiarize themselves with the new CMS guidelines. Understanding the specific requirements for progress note documentation is crucial for compliance.
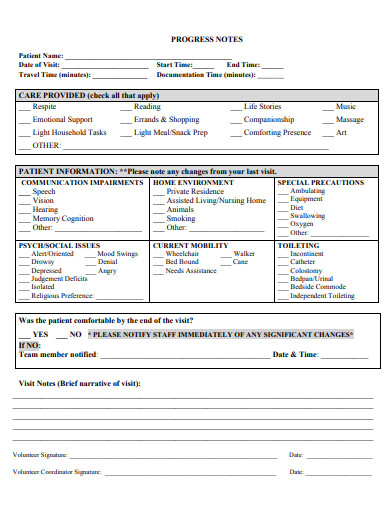
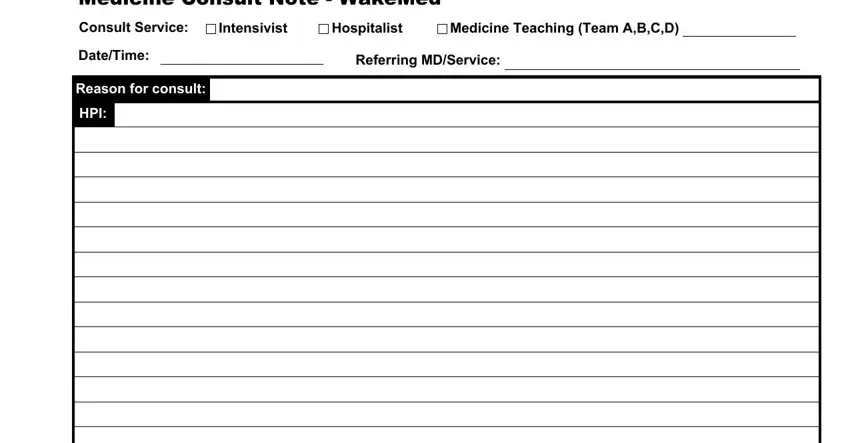
Many practices are exploring ways to streamline their documentation processes. This includes implementing electronic health record (EHR) systems, using templates, and delegating administrative tasks to support staff.
Some providers are also seeking training on effective documentation techniques. This can help them complete progress notes efficiently while still capturing all the necessary information.
Looking Ahead
The long-term impact of the new Medicare progress note requirement remains to be seen. CMS will likely monitor the effects of the policy and make adjustments as needed.
It is essential for healthcare providers to adapt to the changes and find ways to balance documentation requirements with the provision of high-quality patient care. Open communication between providers and CMS will be critical to ensuring that the new policy achieves its intended goals.
The effectiveness of this policy will ultimately depend on how well it is implemented and how it affects both providers and patients in the long run.