Metformin For Weight Loss While Breastfeeding
The use of metformin, a common medication for type 2 diabetes, for weight loss is a growing area of interest, but its safety and efficacy during breastfeeding remains a complex and often debated topic. While some studies suggest limited transfer of the drug into breast milk, questions persist about potential effects on infant development and milk supply, leaving both mothers and healthcare providers grappling with uncertainty.
This article delves into the current understanding of metformin use for weight loss while breastfeeding. It examines existing research, expert opinions, and available guidelines to provide a comprehensive overview of this multifaceted issue. Our goal is to offer evidence-based information to help inform decision-making for breastfeeding mothers considering metformin for weight management.
The Science of Metformin and Breastfeeding
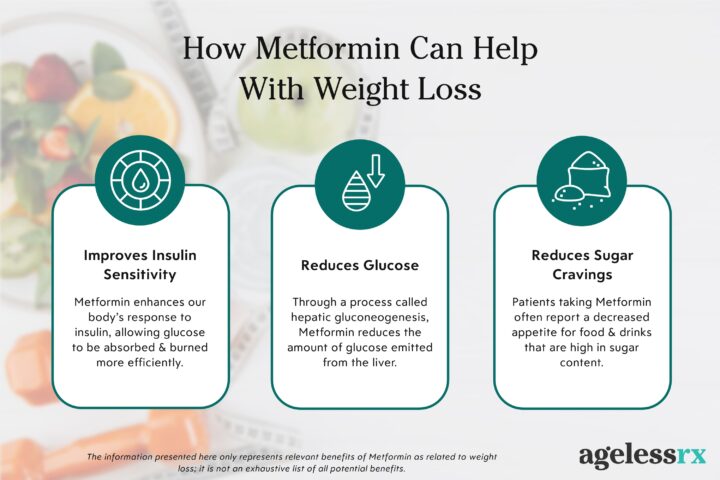
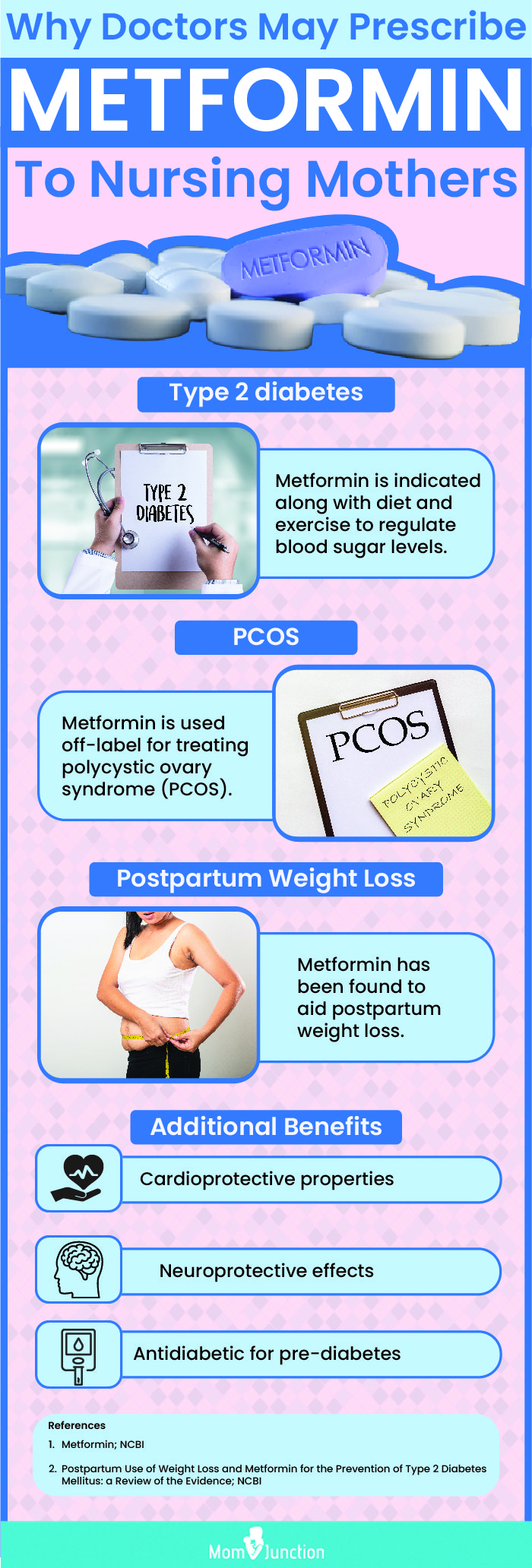
Metformin is primarily used to treat type 2 diabetes by improving insulin sensitivity and reducing glucose production in the liver. Its off-label use for weight loss, particularly in women with polycystic ovary syndrome (PCOS), has gained traction due to its potential to aid in weight management.
However, the critical question is whether metformin passes into breast milk and, if so, what effects it might have on a nursing infant. Studies have attempted to quantify the transfer of metformin into breast milk, but results vary.
Research suggests that metformin does transfer into breast milk, but in relatively low concentrations. A study published in *Diabetes Care* found that the infant's exposure to metformin through breast milk was significantly lower than the therapeutic dose given directly to infants. However, long-term effects of even low-level exposure remain largely unknown.
Expert Opinions and Guidelines
The Academy of Breastfeeding Medicine (ABM) has issued guidelines on the use of medications during breastfeeding, but specific recommendations on metformin are somewhat cautious. While acknowledging that metformin appears to be compatible with breastfeeding, they emphasize the need for individualized assessment.
Healthcare professionals generally advise weighing the potential benefits for the mother against the possible risks to the infant. "The decision to use metformin while breastfeeding should be made in consultation with a doctor," states Dr. Emily Carter, a lactation consultant, "taking into account the mother's overall health, weight loss goals, and the infant's health status."
Potential Risks to the Infant
One primary concern is the potential for hypoglycemia (low blood sugar) in the infant, although this is considered rare with metformin. Another concern is the unknown long-term effects on the infant's gastrointestinal system, as metformin can cause gastrointestinal side effects in adults.
Furthermore, some experts have raised concerns about the potential impact on the infant's developing gut microbiome. However, more research is needed to confirm these potential risks.
Dr. David Lee, a pediatrician specializing in infant nutrition, notes, "While the amount of metformin in breast milk is typically low, we lack sufficient data to rule out subtle effects on infant growth and development, especially with prolonged exposure."
Impact on Milk Supply
Another crucial consideration is the potential impact of metformin on milk supply. Some anecdotal reports suggest that metformin can reduce milk production, potentially due to its effects on hormonal balance.
However, scientific evidence on this topic is limited and inconsistent. Some studies suggest that metformin may even improve milk supply in women with PCOS who have insulin resistance, potentially due to its impact on insulin levels.
Careful monitoring of milk supply and infant weight gain is essential for breastfeeding mothers taking metformin. If a decrease in milk supply is observed, consulting with a lactation consultant is highly recommended.
Making Informed Decisions
Ultimately, the decision of whether to use metformin for weight loss while breastfeeding is a personal one that should be made in consultation with healthcare professionals. Mothers should have open and honest conversations with their doctors and lactation consultants to weigh the risks and benefits.
Alternative strategies for weight loss during breastfeeding, such as diet and exercise, should also be explored. A healthy diet rich in fruits, vegetables, and whole grains, combined with regular physical activity, can often be effective for weight management without the potential risks associated with medication.
"The key is to prioritize the health and well-being of both the mother and the infant," emphasizes Dr. Carter. "A comprehensive approach that includes lifestyle modifications and close monitoring is essential for safe and effective weight management during breastfeeding."
Conclusion
The use of metformin for weight loss while breastfeeding is a complex issue with limited definitive data. While some studies suggest low levels of metformin transfer into breast milk, potential risks to the infant and impacts on milk supply remain concerns.
Individualized assessment and careful monitoring are crucial for breastfeeding mothers considering metformin. Open communication with healthcare providers, exploration of alternative weight loss strategies, and prioritization of both maternal and infant health are paramount in making informed decisions.
Further research is needed to fully understand the long-term effects of metformin exposure through breast milk and to provide more definitive guidelines for its use in breastfeeding mothers. This will help ensure the safety and well-being of both mothers and their infants.