Nursing Care Plan For Fluid Electrolyte Imbalance

Hospitals nationwide are facing a critical surge in patients presenting with severe fluid and electrolyte imbalances. The escalating cases are pushing healthcare systems to rapidly refine and implement effective nursing care plans.
This surge, impacting both adult and pediatric populations, necessitates immediate action to standardize treatment protocols and improve patient outcomes. Standardized protocols are especially critical given the wide range of potential causes, from acute illnesses to chronic conditions.
Recognizing the Imbalance
Early identification is paramount. Nurses must be vigilant in recognizing the signs and symptoms of fluid and electrolyte imbalances, which can manifest differently depending on the specific imbalance.
Common indicators include altered mental status, muscle weakness or cramps, changes in heart rate and blood pressure, edema, and abnormal urine output. Accurate and timely assessment is crucial for guiding appropriate interventions.
Immediate Nursing Actions
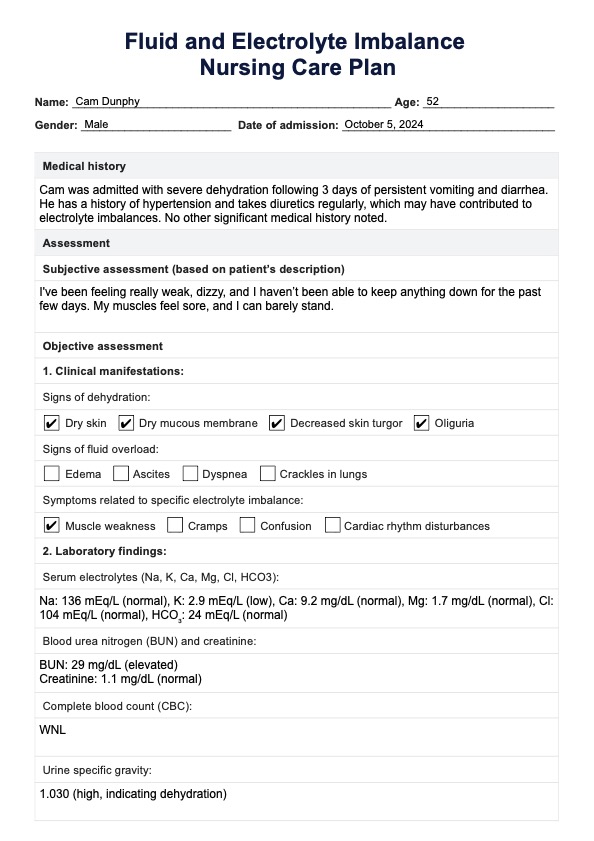
Upon identifying a suspected imbalance, the first step is to initiate continuous monitoring of vital signs, including heart rate, blood pressure, respiratory rate, and oxygen saturation. Careful recording of intake and output is also mandatory.
Accurate and frequent monitoring provides the foundation for tailoring the nursing care plan. Laboratory values, specifically serum electrolytes (sodium, potassium, calcium, magnesium, chloride), blood urea nitrogen (BUN), creatinine, and osmolality, must be reviewed promptly.
Based on the assessment, initiate fluid resuscitation as prescribed by the physician. This may involve administering intravenous fluids, such as normal saline or lactated Ringer's solution, depending on the patient's specific needs and electrolyte profile.
Potassium Imbalance: A Critical Focus
Potassium imbalances, both hypokalemia (low potassium) and hyperkalemia (high potassium), require particularly urgent attention. Potassium plays a vital role in cardiac function, and even slight deviations from the normal range can have life-threatening consequences.
For hypokalemia, administer potassium supplements as prescribed, either orally or intravenously, closely monitoring the patient's cardiac rhythm. For hyperkalemia, implement measures to lower potassium levels, such as administering medications like sodium polystyrene sulfonate (Kayexalate) or insulin and glucose.
Sodium Imbalance: Managing Fluid Shifts
Sodium imbalances, including hyponatremia (low sodium) and hypernatremia (high sodium), require careful management of fluid shifts. Rapid correction of sodium imbalances can lead to severe neurological complications.
In hyponatremia, fluid restriction may be necessary, and in some cases, hypertonic saline may be administered under close supervision. In hypernatremia, gradual rehydration with hypotonic fluids is essential to prevent cerebral edema.
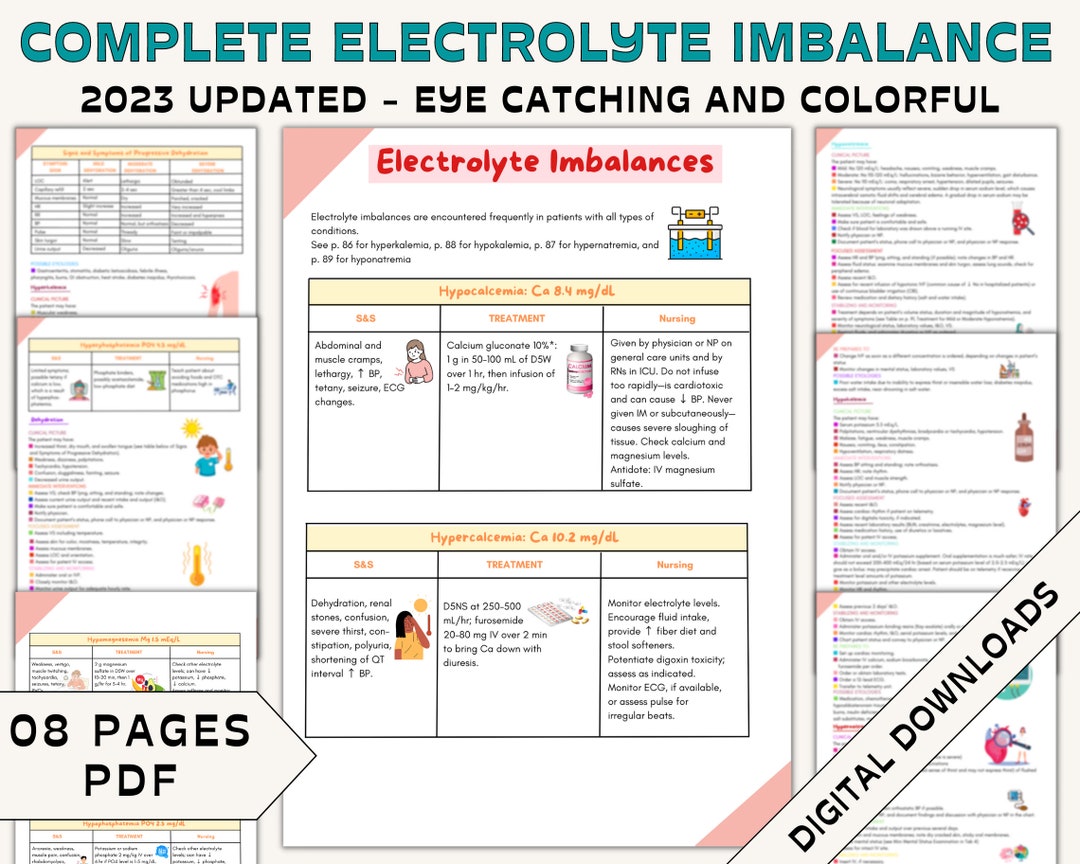
Calcium and Magnesium Imbalances
Calcium and magnesium imbalances, while less common than sodium and potassium imbalances, can also have significant clinical consequences. Hypocalcemia can lead to tetany and seizures, while hypercalcemia can cause cardiac arrhythmias and renal dysfunction.
Similarly, hypomagnesemia can result in cardiac arrhythmias and muscle weakness, while hypermagnesemia can lead to respiratory depression and cardiac arrest. Prompt identification and correction of these imbalances are crucial.
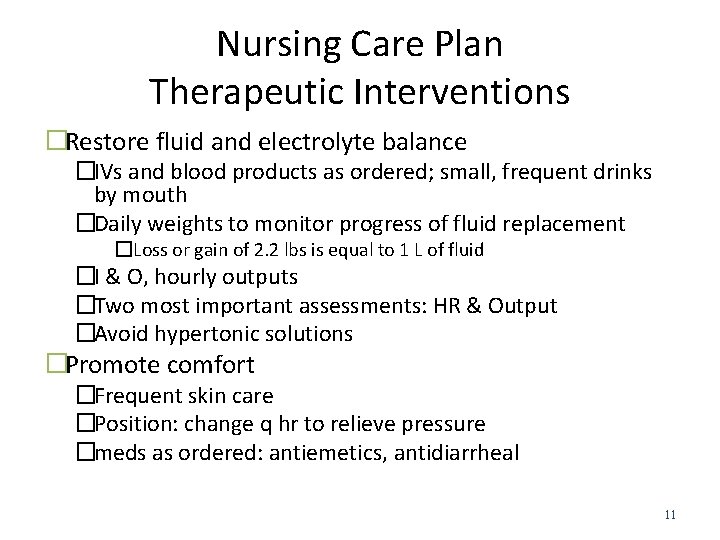
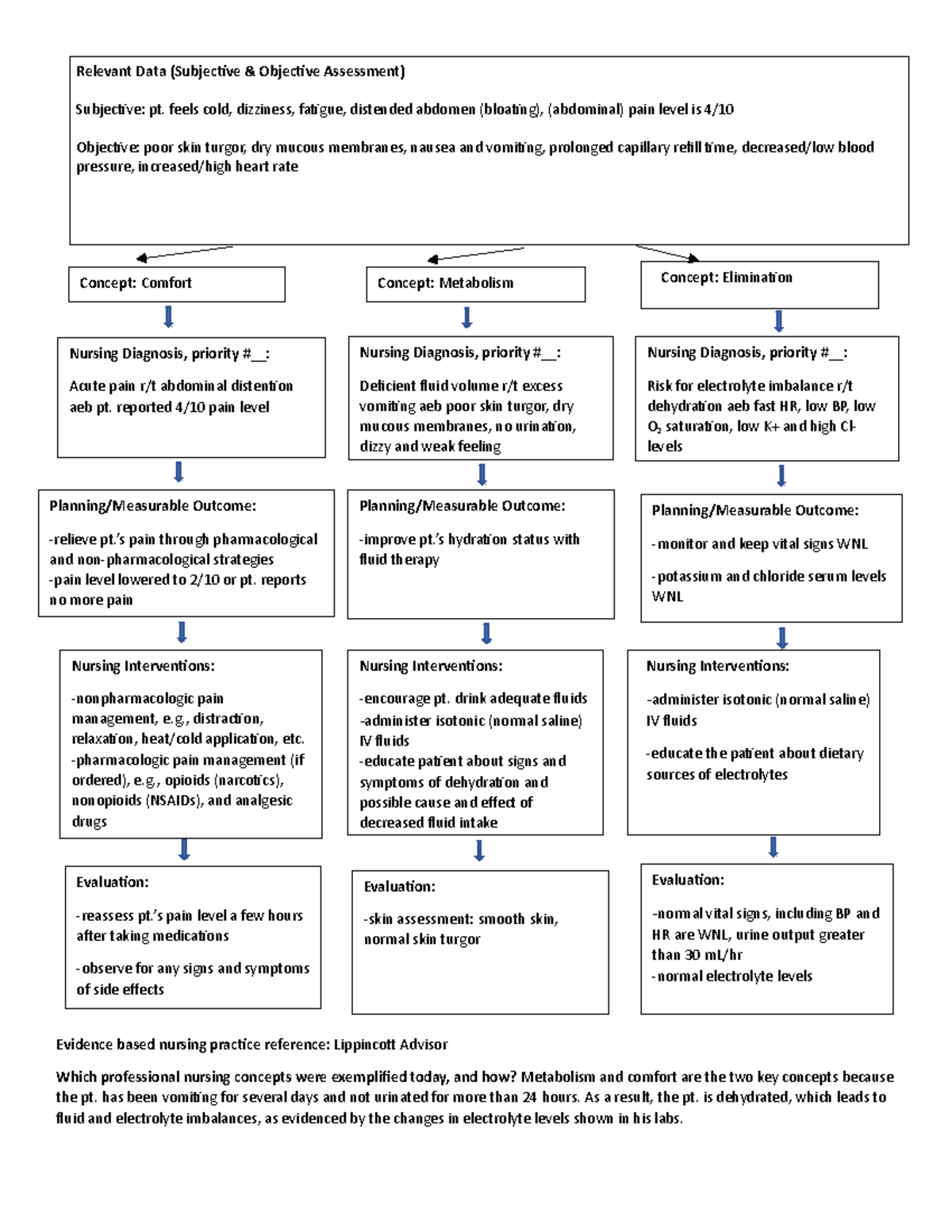
Developing the Nursing Care Plan
The nursing care plan must be individualized to address the patient's specific needs and underlying medical conditions. The plan should include specific goals for fluid and electrolyte balance, as well as measurable outcomes.
Examples of goals include maintaining adequate hydration, restoring normal electrolyte levels, and preventing complications such as cardiac arrhythmias or seizures. The nursing interventions should be clearly outlined, including medication administration, fluid management, and monitoring parameters.
Patient Education and Discharge Planning
Patient education is an integral component of the nursing care plan. Patients and their families need to understand the importance of maintaining adequate hydration, following dietary recommendations, and recognizing the signs and symptoms of fluid and electrolyte imbalances.
Before discharge, provide patients with clear instructions on medication administration, fluid intake, and follow-up appointments. Ensure they have the resources they need to manage their condition at home.
Current Data and Trends
Recent studies indicate a 15% increase in hospital admissions related to fluid and electrolyte imbalances over the past year. The Centers for Disease Control and Prevention (CDC) is investigating potential contributing factors, including changes in dietary habits, medication use, and environmental conditions.
The American Nurses Association (ANA) is actively promoting continuing education programs for nurses to enhance their knowledge and skills in managing fluid and electrolyte imbalances. The Joint Commission is also emphasizing the importance of standardized protocols and interdisciplinary collaboration in addressing this growing healthcare challenge.
Next Steps and Ongoing Developments
Healthcare institutions are implementing mandatory training programs for nurses on the recognition and management of fluid and electrolyte imbalances. Research is underway to identify new and more effective strategies for preventing and treating these conditions.
A national task force, comprised of physicians, nurses, and other healthcare professionals, has been formed to develop national guidelines for the management of fluid and electrolyte imbalances. The goal is to standardize care across all healthcare settings and improve patient outcomes.