Nursing Goals For Impaired Skin Integrity
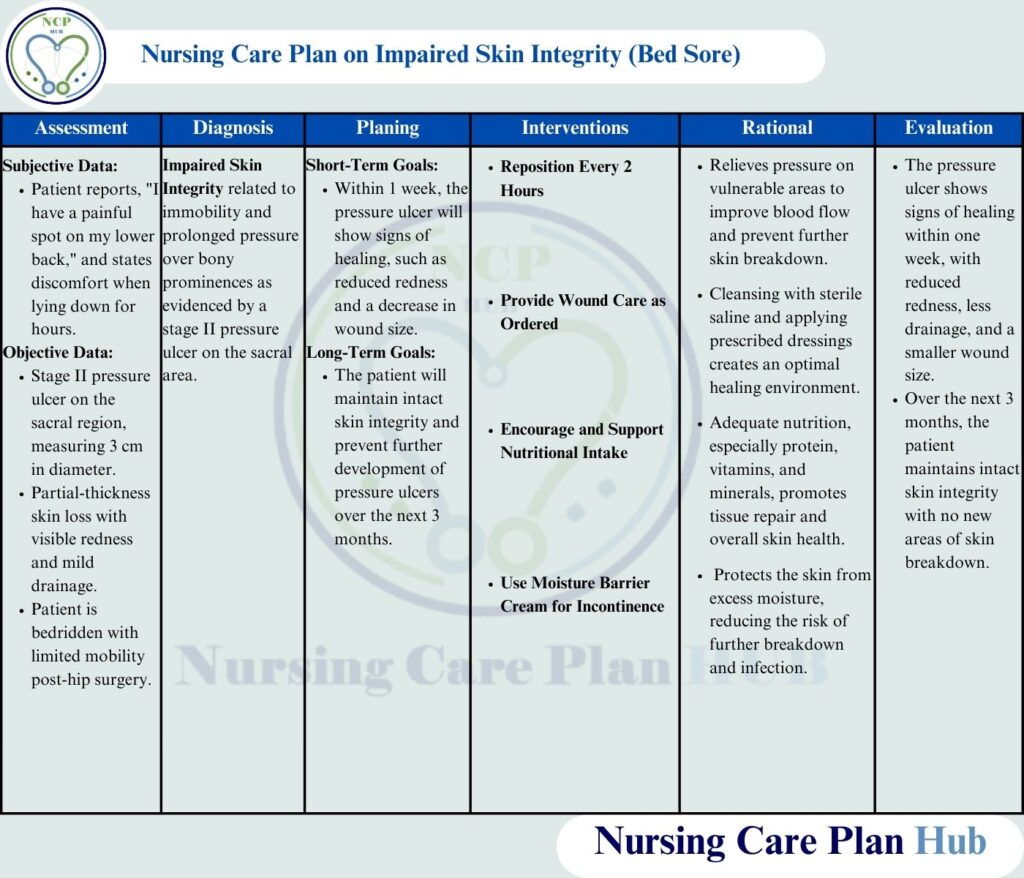
The silent epidemic of impaired skin integrity plagues healthcare facilities worldwide, impacting patient outcomes and driving up costs. Pressure ulcers, surgical wounds, and other forms of skin breakdown not only cause immense pain and suffering but also increase the risk of infection, prolonged hospital stays, and even mortality. The challenge is immense, requiring a multi-faceted approach grounded in evidence-based practice and dedicated nursing care.
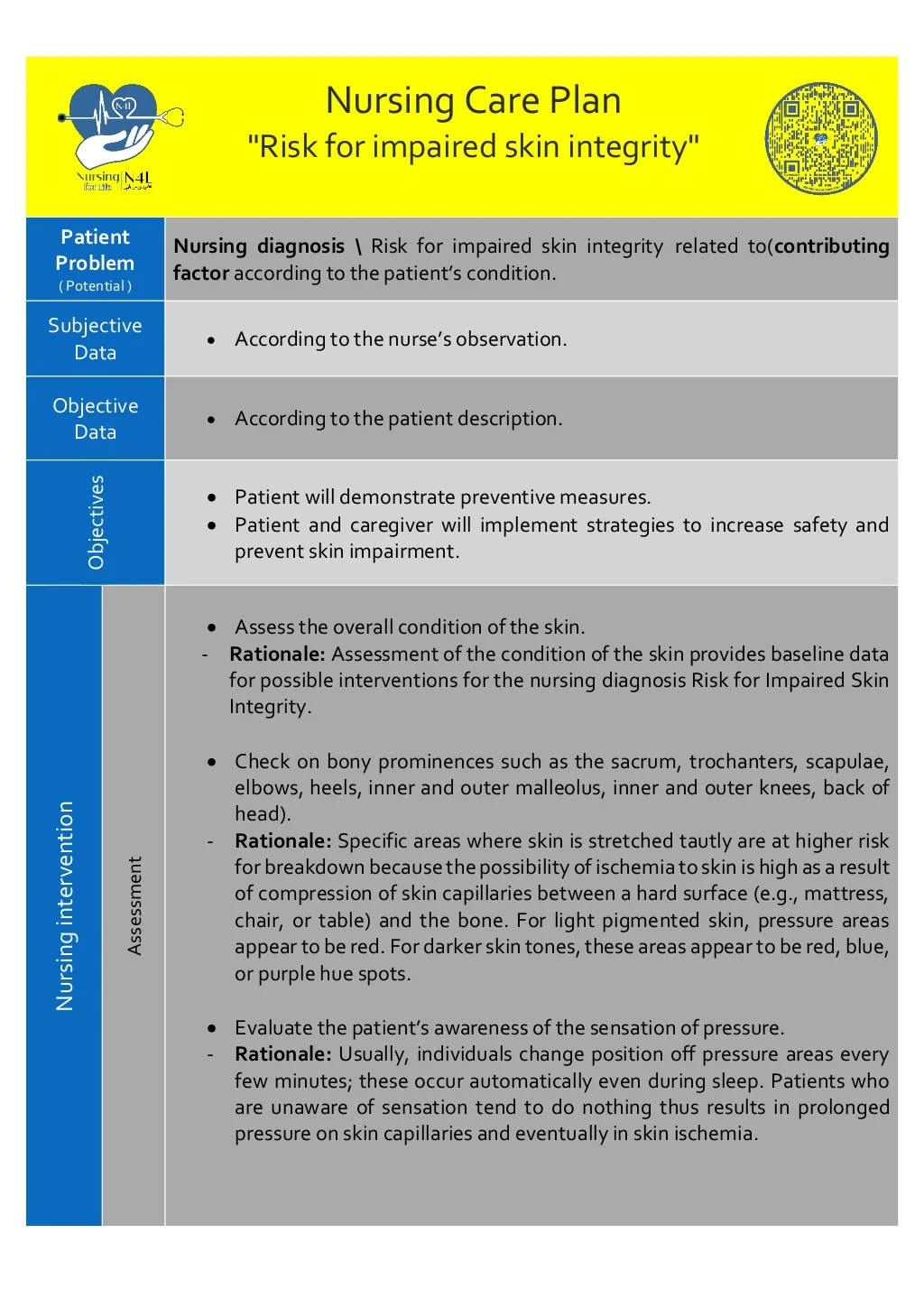
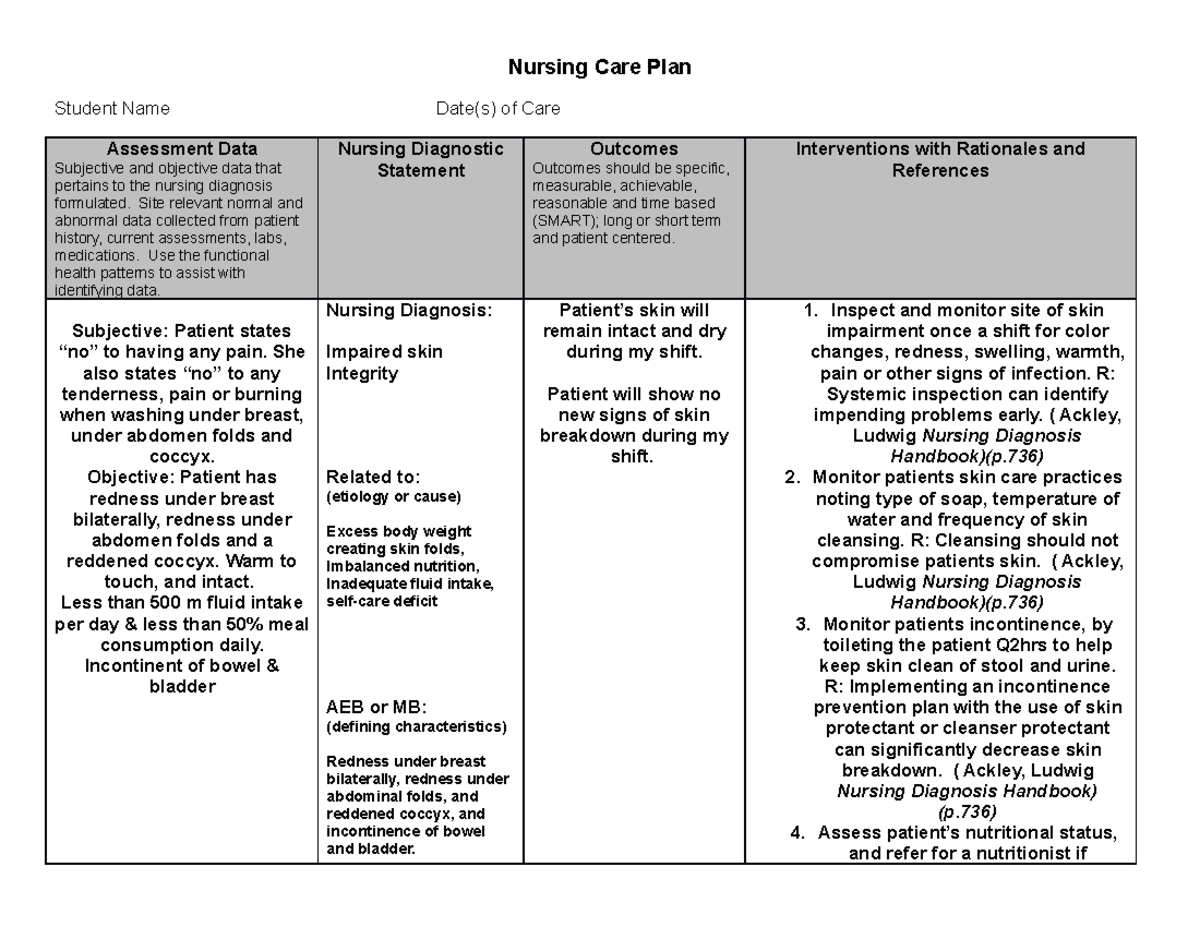
The following article delves into the crucial nursing goals for addressing impaired skin integrity. This includes prevention, early detection, and effective management. We explore the key strategies and protocols nurses employ, the technological advancements aiding in skin assessment and treatment, and the continuing need for education and collaboration to improve patient outcomes in this critical area of healthcare.
Prevention: The First Line of Defense
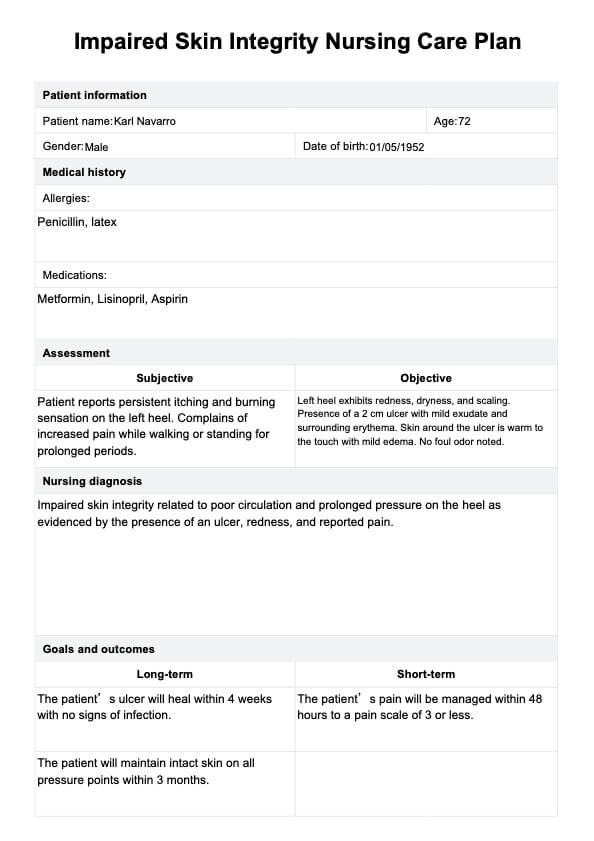
Prevention is paramount in managing impaired skin integrity. Nurses play a vital role in implementing preventative measures to minimize the risk of skin breakdown.
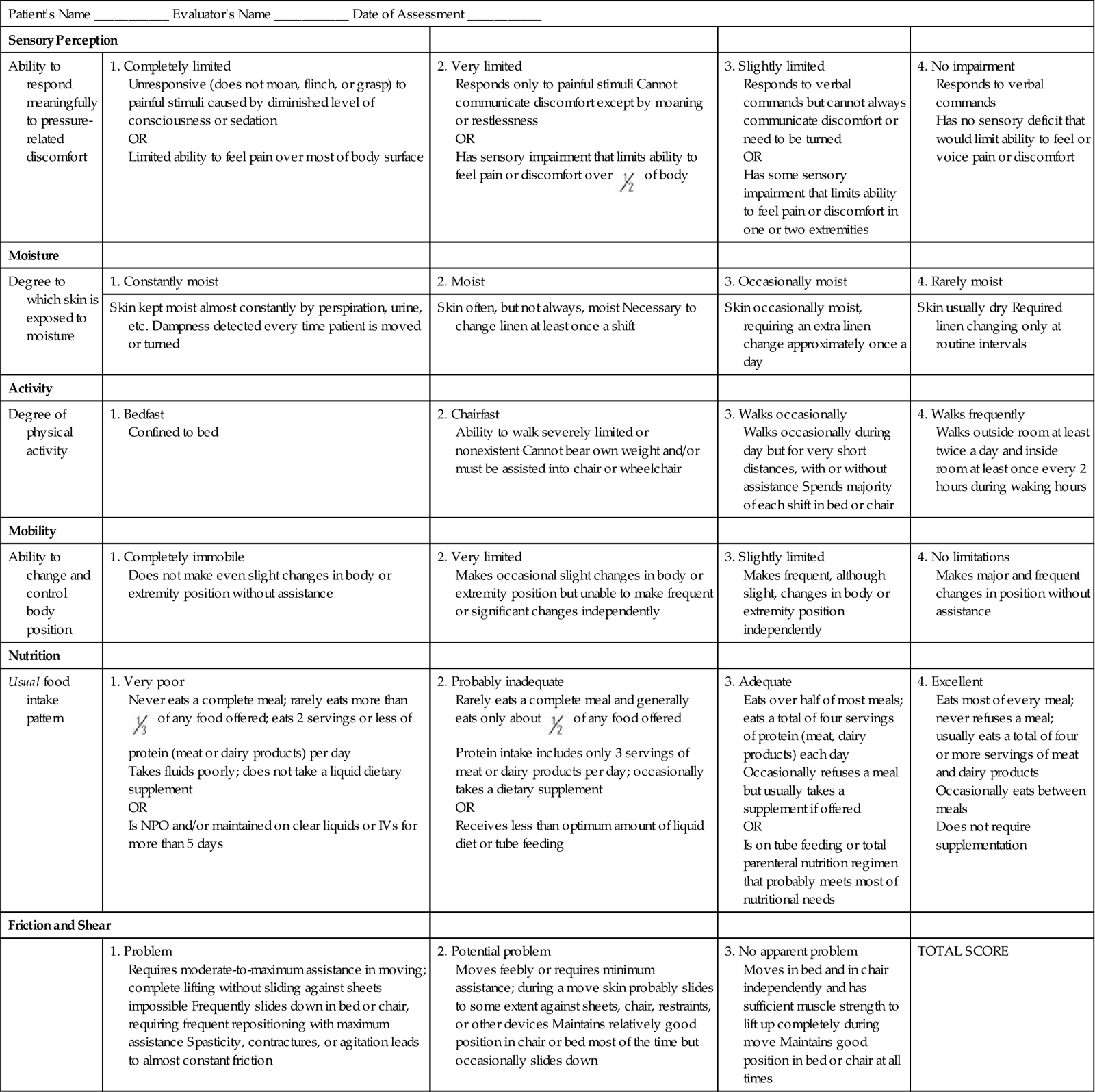
This involves comprehensive risk assessments using validated tools like the Braden Scale, which evaluates factors like sensory perception, moisture, activity, mobility, nutrition, and friction/shear.
Based on the assessment, tailored interventions are implemented.
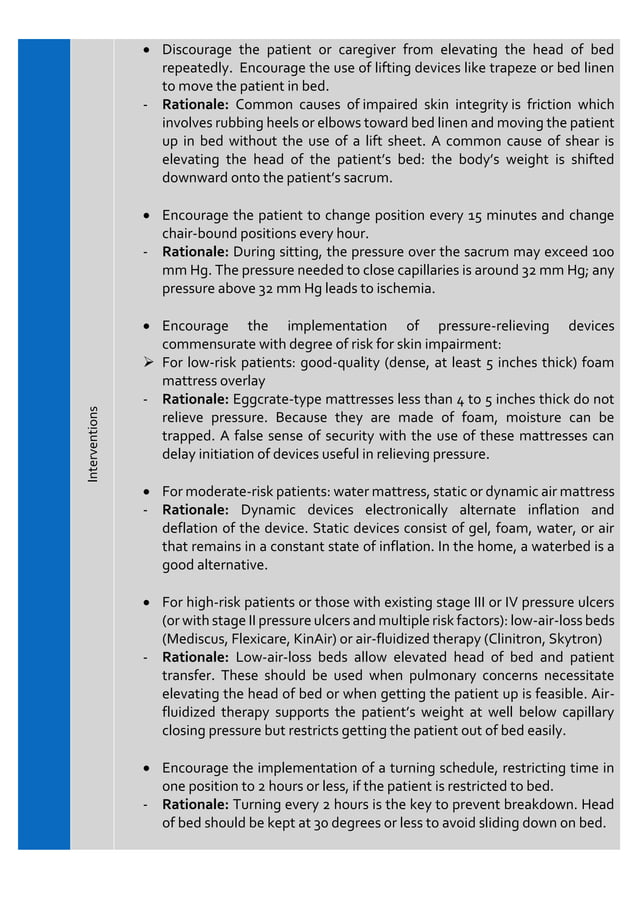
Repositioning and Offloading Pressure
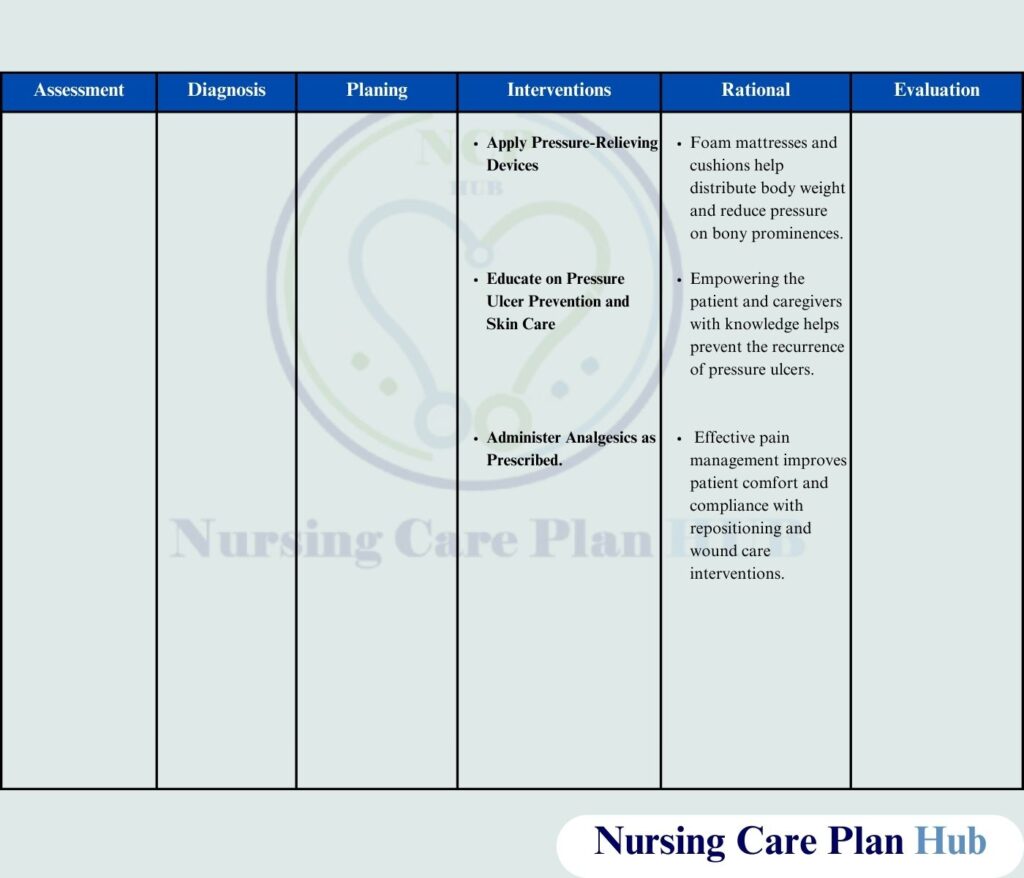
Frequent repositioning is a cornerstone of pressure ulcer prevention. Patients at risk are typically repositioned every two hours or more frequently, depending on their individual needs.
Specialized support surfaces, such as pressure-redistributing mattresses and cushions, are used to offload pressure from bony prominences.
Proper positioning techniques and the use of assistive devices minimize friction and shear forces that contribute to skin damage.
Skin Care and Moisture Management
Maintaining skin hygiene is crucial. This includes gentle cleansing with pH-balanced cleansers and avoiding harsh soaps that can strip the skin of its natural oils.
Moisturizing the skin regularly helps prevent dryness and cracking, reducing the risk of skin breakdown.
Incontinence-associated dermatitis (IAD) is a significant concern; prompt management with appropriate barrier creams and frequent cleansing is essential.
Nutritional Support
Adequate nutrition is vital for skin health and wound healing. Patients at risk of or experiencing skin breakdown require sufficient protein, vitamins, and minerals.
Nurses work with dietitians to ensure patients receive appropriate nutritional support through oral intake, enteral feeding, or parenteral nutrition if necessary.
Hydration is also crucial, as dehydration can compromise skin integrity.
Early Detection: Recognizing the Signs
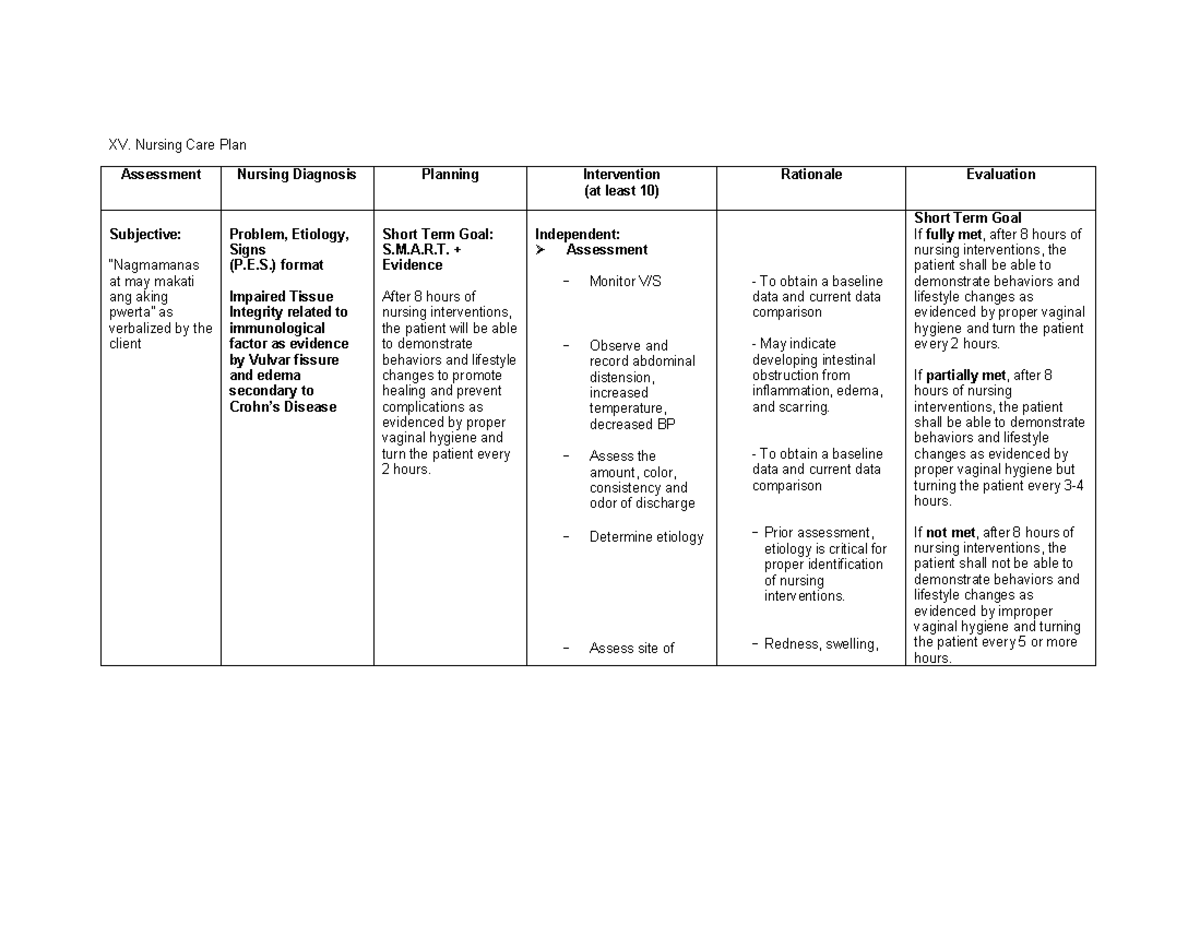
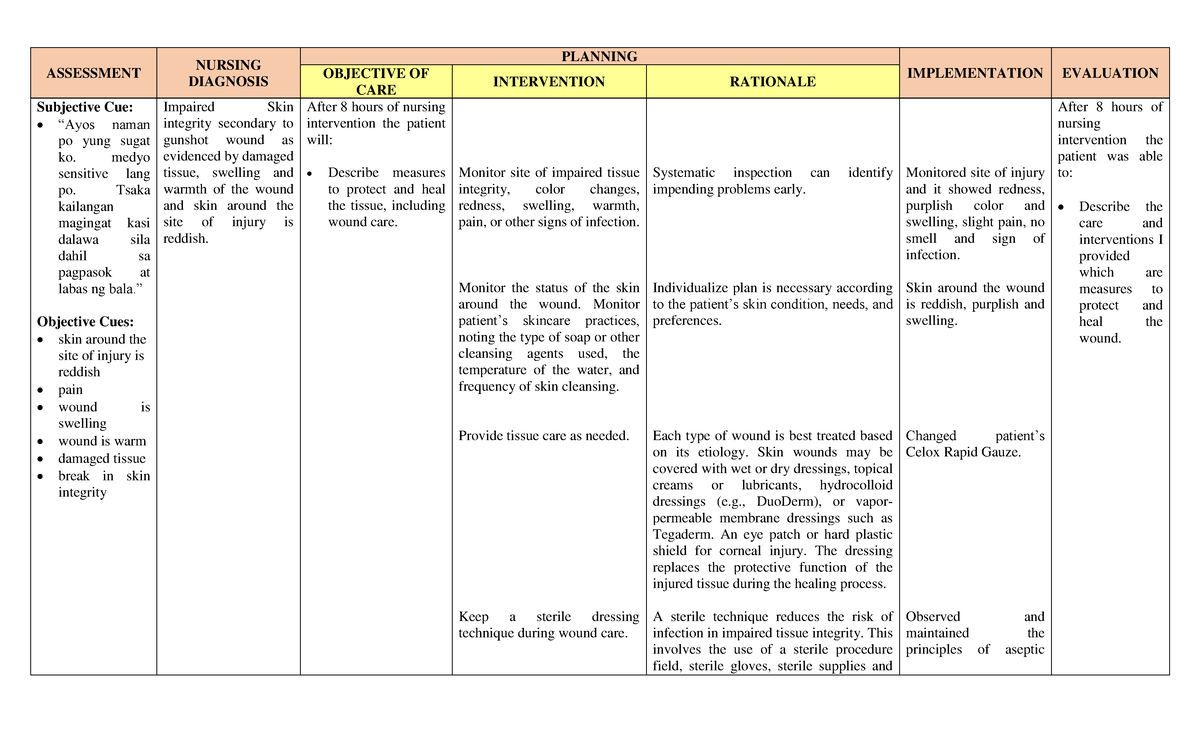
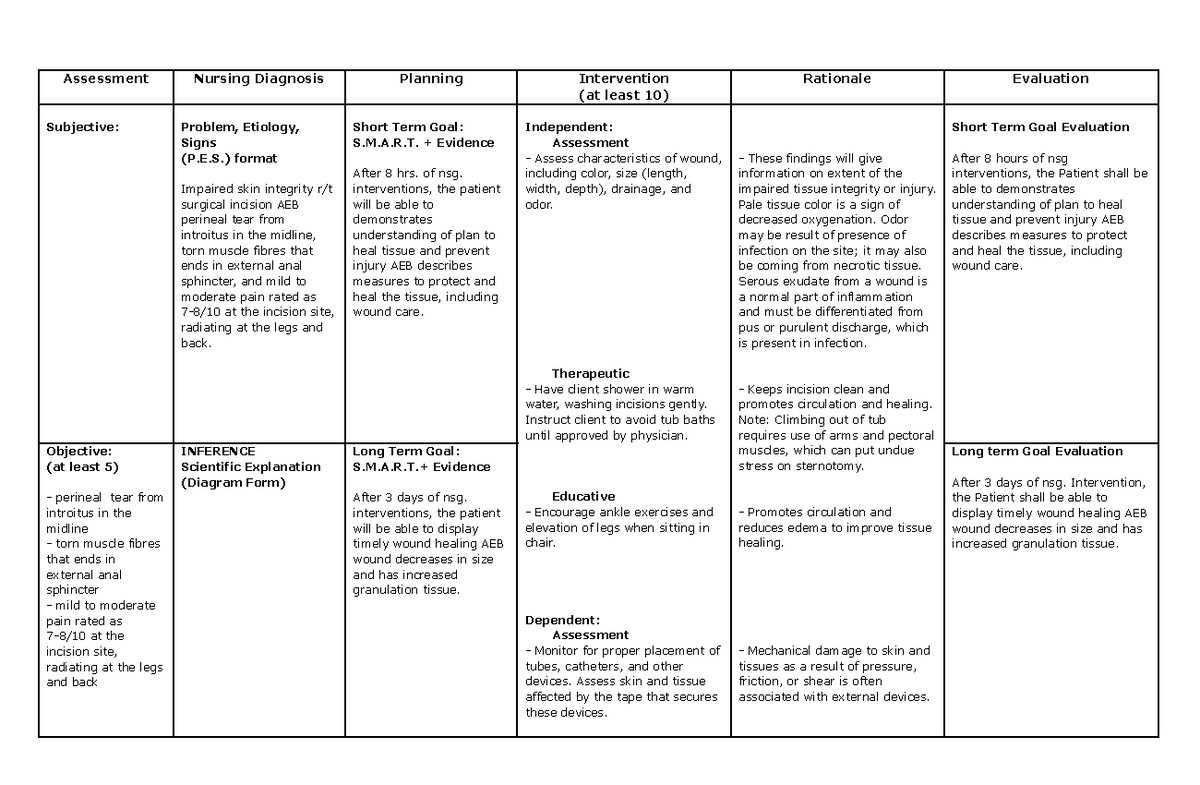
Early detection of skin changes is crucial for preventing further deterioration. Nurses are trained to identify subtle signs of skin breakdown.
This involves regular skin assessments, paying close attention to bony prominences and areas exposed to pressure, moisture, or friction.
Visual inspection, palpation, and the use of assistive devices like skin assessment lights can aid in early detection.
Stages of Pressure Ulcers
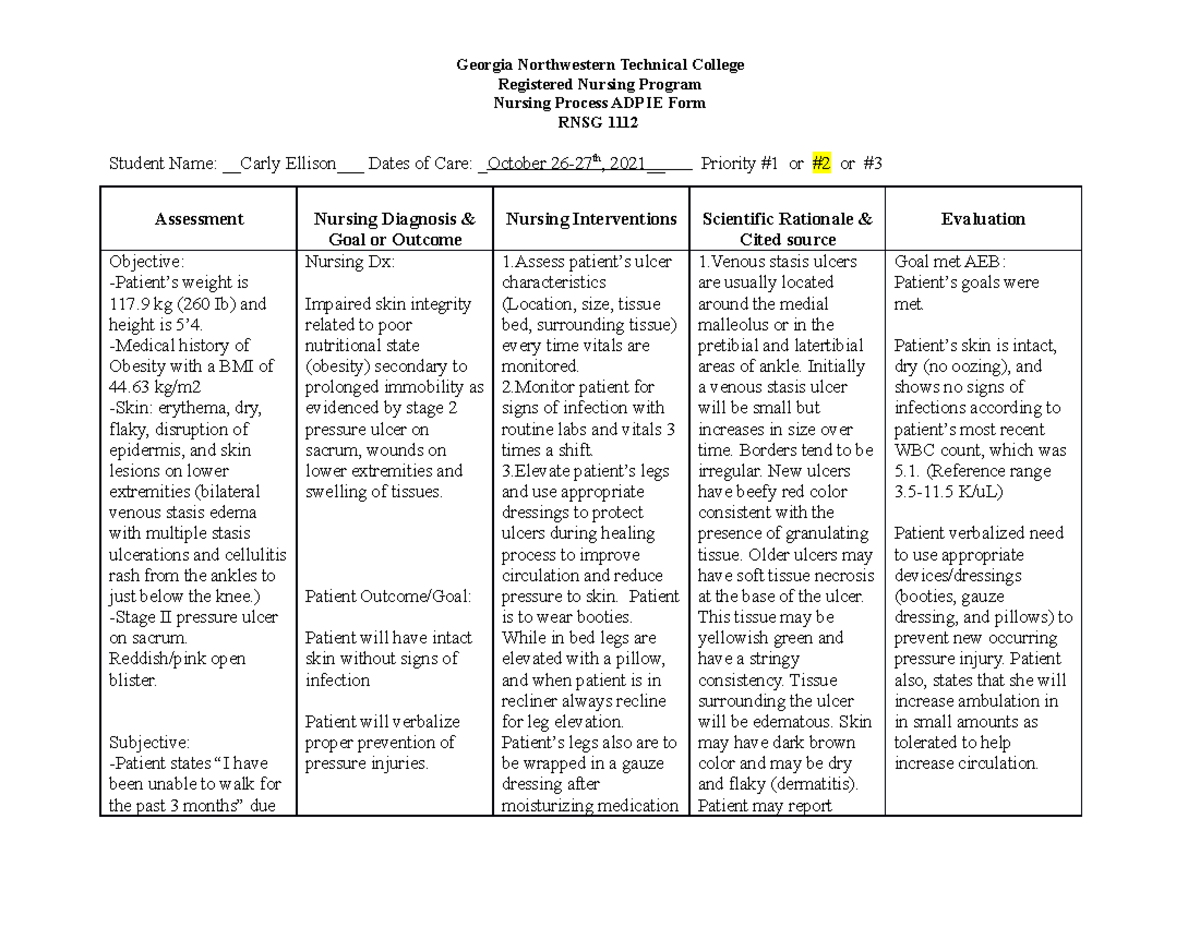
Accurate staging of pressure ulcers is essential for guiding treatment decisions. The National Pressure Injury Advisory Panel (NPIAP) defines specific stages based on the depth and characteristics of the wound.
Stage 1 involves non-blanchable erythema of intact skin, while Stage 2 presents with partial-thickness skin loss involving the epidermis or dermis.
Stages 3 and 4 involve full-thickness skin loss, potentially extending to subcutaneous tissue, muscle, or bone.
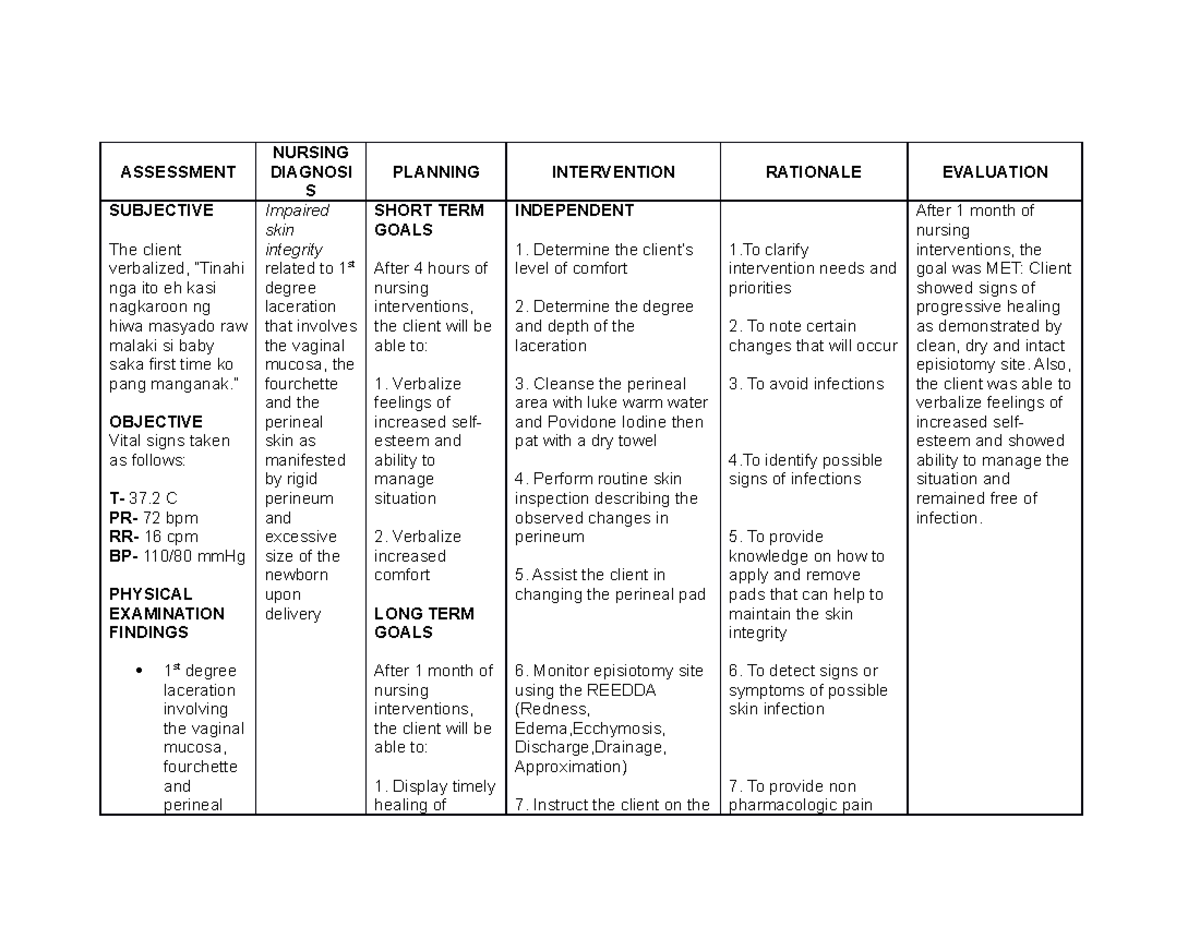
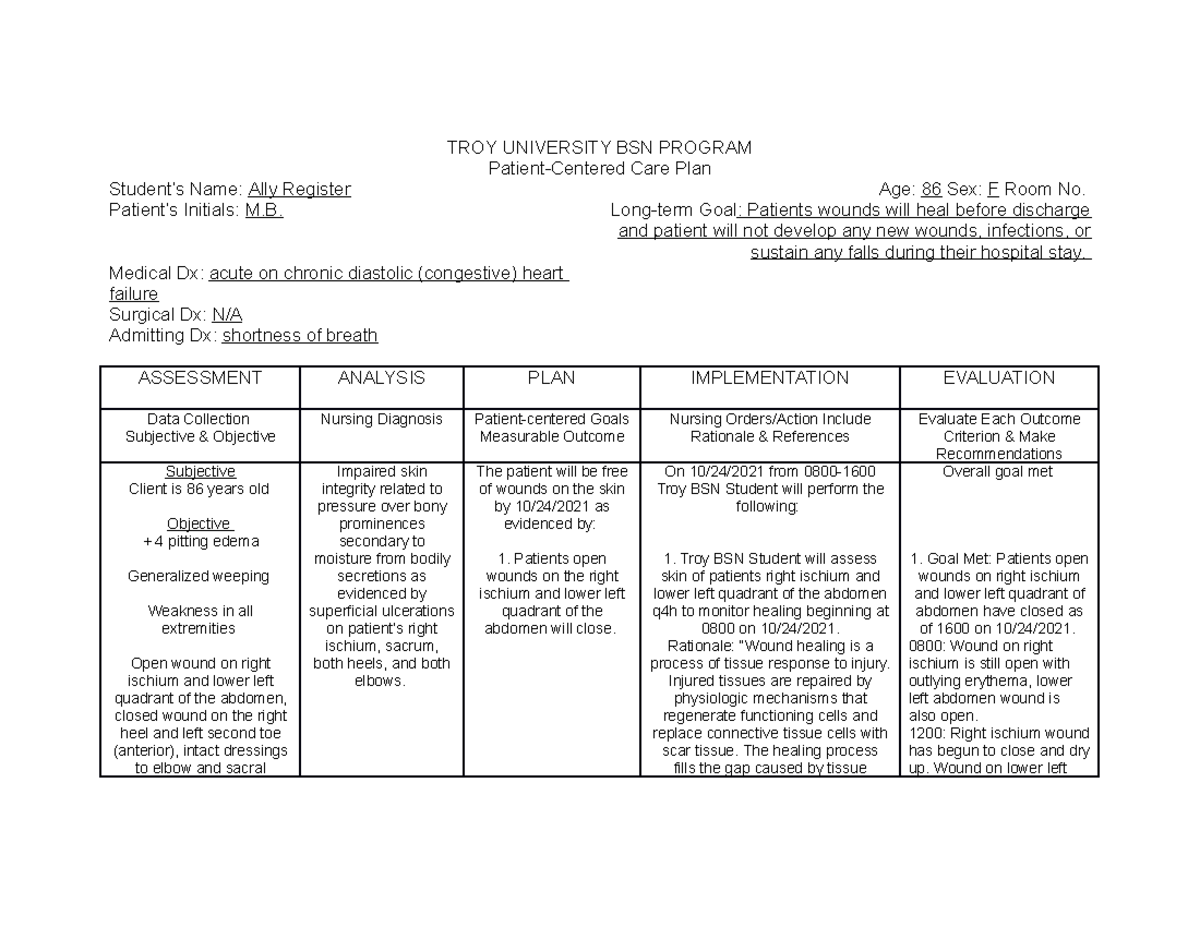
Documentation and Communication
Thorough documentation of skin assessments is critical. This includes detailed descriptions of wound characteristics, such as size, location, stage, and drainage.
Effective communication among healthcare team members is essential to ensure consistent and coordinated care. Nurses play a central role in communicating skin assessment findings and treatment plans to physicians, wound care specialists, and other relevant providers.
Digital photography can be a valuable tool for tracking wound progress over time.
Management: Implementing Evidence-Based Strategies
Effective management of impaired skin integrity requires a multidisciplinary approach. Nurses collaborate with physicians, wound care specialists, and other healthcare professionals to develop individualized treatment plans.
These plans address the underlying causes of skin breakdown and promote wound healing.
Wound care protocols are based on evidence-based guidelines and tailored to the specific characteristics of the wound.
Wound Cleansing and Debridement
Wound cleansing is essential for removing debris and bacteria. Normal saline is typically used for wound cleansing, as it is non-toxic to healthy tissue.
Debridement involves the removal of necrotic tissue, which can impede wound healing. Several debridement methods are available, including sharp, enzymatic, and autolytic debridement.
The choice of debridement method depends on the type and amount of necrotic tissue, the patient's overall health, and the available resources.
Wound Dressings
Wound dressings play a crucial role in promoting wound healing. Various types of dressings are available, each with specific properties and indications.
These include hydrocolloids, hydrogels, foams, alginates, and films. The appropriate dressing is selected based on the wound's characteristics, such as exudate level, depth, and presence of infection.
Nurses are responsible for applying and changing dressings according to established protocols.
Pain Management
Pain is a common symptom associated with impaired skin integrity. Nurses play a key role in assessing and managing pain.
This includes the use of pharmacological and non-pharmacological interventions. Pain medications, such as analgesics and topical anesthetics, may be prescribed.
Non-pharmacological interventions, such as repositioning, distraction, and relaxation techniques, can also help manage pain.
The Future of Nursing and Skin Integrity
The field of wound care is constantly evolving. Technological advancements, such as negative pressure wound therapy (NPWT) and bioengineered skin substitutes, are improving outcomes for patients with complex wounds.
Nurses must stay abreast of these advancements to provide the best possible care. Furthermore, continuing education and certification in wound care are essential for nurses specializing in this area.
Addressing impaired skin integrity requires a sustained commitment to prevention, early detection, and evidence-based management. By prioritizing these goals, nurses can significantly improve patient outcomes and reduce the burden of this pervasive healthcare challenge. The collaborative efforts of healthcare professionals, patients, and caregivers are essential to achieving optimal skin health and preventing the devastating consequences of skin breakdown. Further research and innovation are crucial to developing even more effective strategies for preventing and managing impaired skin integrity, ultimately improving the quality of life for countless individuals.