Pathophysiology Of Congestive Heart Failure Pdf
Imagine your heart, a tireless engine, diligently pumping life-giving blood through your veins. Now, picture that engine struggling, weakening, unable to keep up with the body’s demands. This is the essence of congestive heart failure (CHF), a condition where the heart's pumping power is compromised.
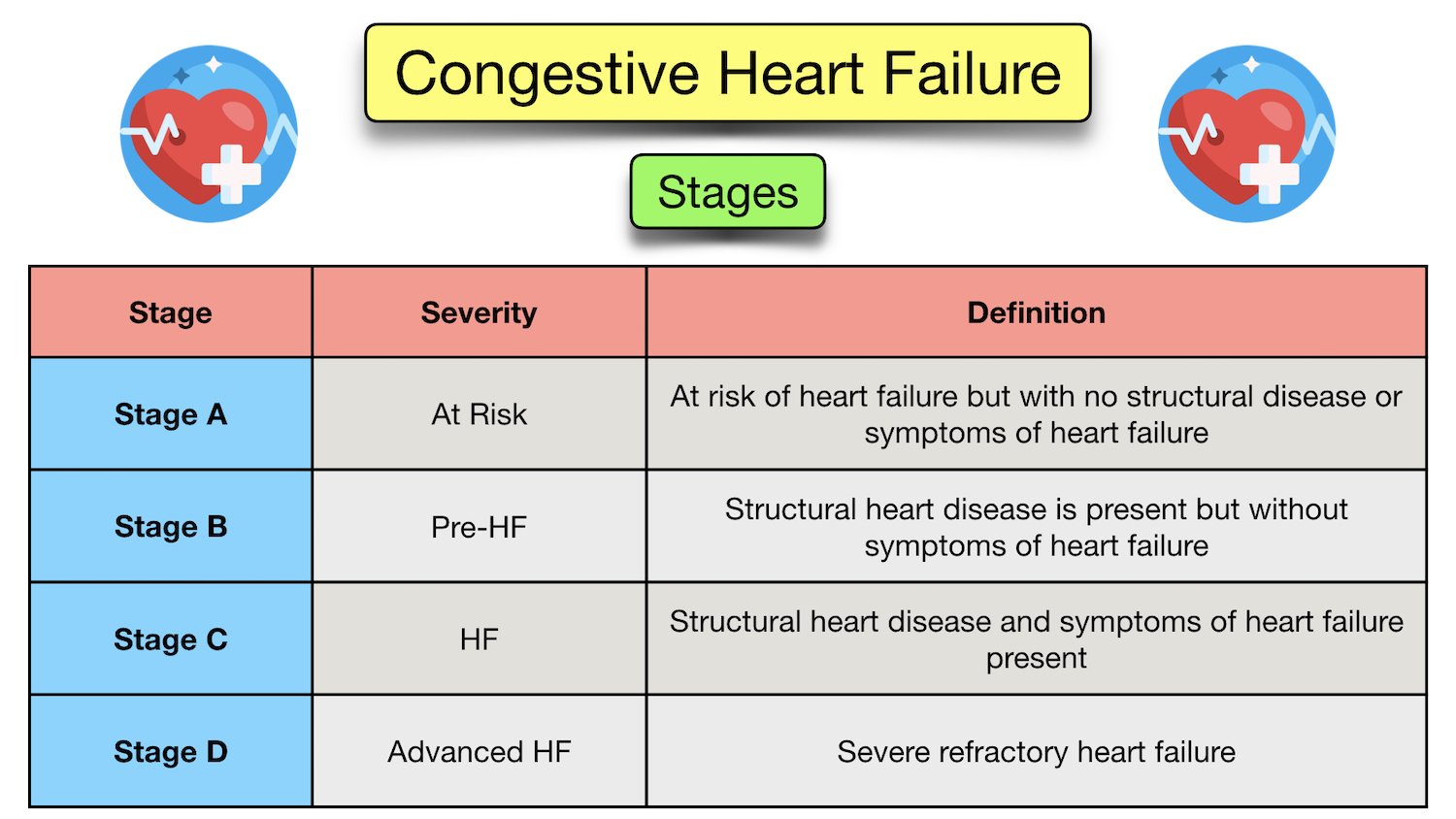
At its core, CHF isn't a sudden stop, but a gradual decline. Understanding the intricate mechanisms that lead to this decline – the pathophysiology – is crucial for effective diagnosis, treatment, and ultimately, improving the lives of those affected. This article delves into the complexities of CHF pathophysiology, exploring the cascade of events that transform a healthy heart into one struggling to survive.
Understanding Congestive Heart Failure
Congestive Heart Failure (CHF), often simply referred to as heart failure, is a chronic progressive condition. It affects millions worldwide. The heart, unable to pump sufficiently, leads to fluid build-up in the lungs and other body parts.
Think of it like this: a garden hose with a kink. The water still flows, but at a reduced pressure, leading to insufficient irrigation and eventual pooling where it shouldn’t be. This analogy, while simplified, captures the essence of how CHF impacts the body.
What is Pathophysiology?
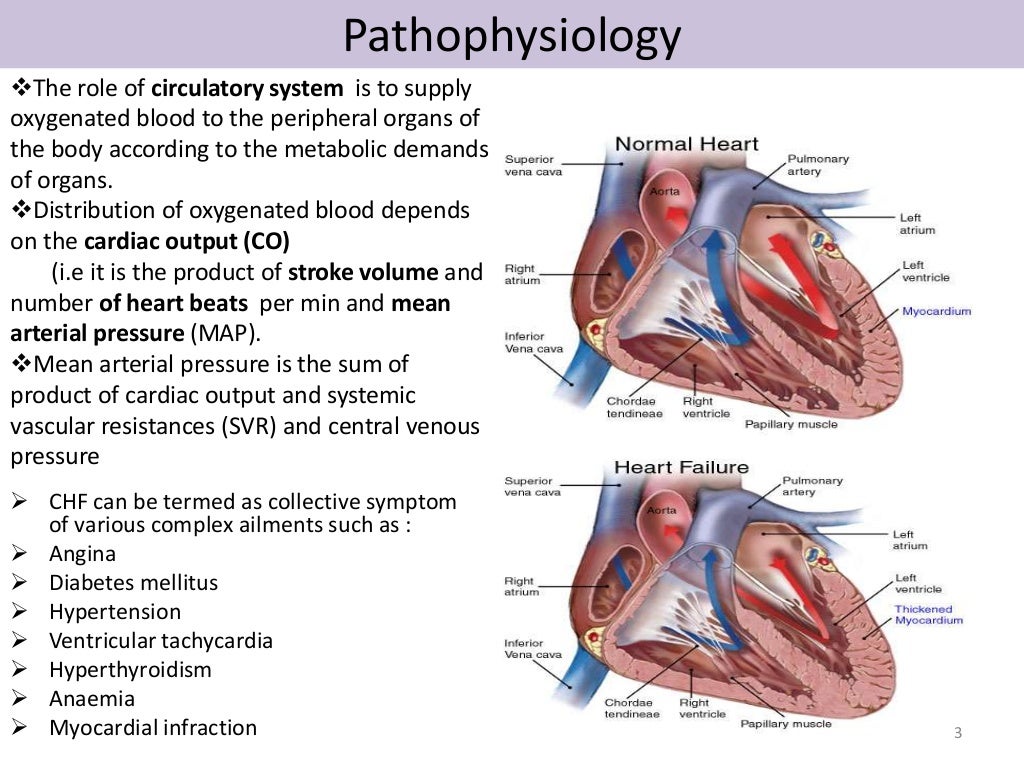
Pathophysiology is the study of how normal physiological processes are disrupted by disease. In the context of CHF, it explores the mechanisms that cause the heart to weaken and fail. It considers the intricate interplay of cellular changes, hormonal imbalances, and structural alterations.
Understanding these mechanisms allows healthcare professionals to develop targeted therapies. These therapies aim to slow the progression of the disease. They can also manage its symptoms more effectively.
The Cascade of Events: Pathophysiology of CHF
CHF rarely arises overnight; it typically unfolds through a series of interconnected events. Factors like high blood pressure, coronary artery disease, and previous heart attacks can initiate this cascade.
These initial insults force the heart to work harder. This eventually leads to structural and functional changes that compromise its ability to pump blood effectively. This is often where the problems begin.
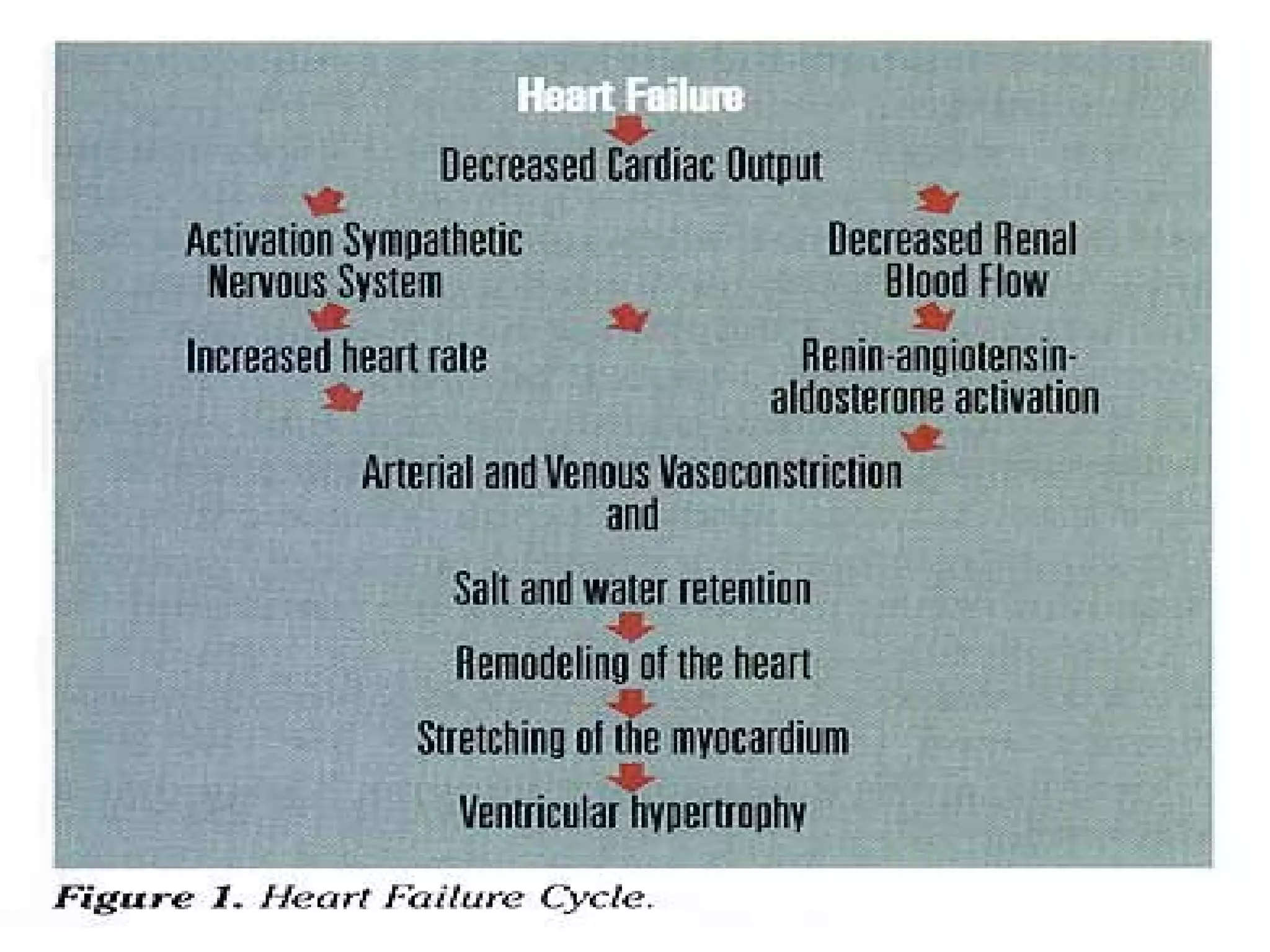
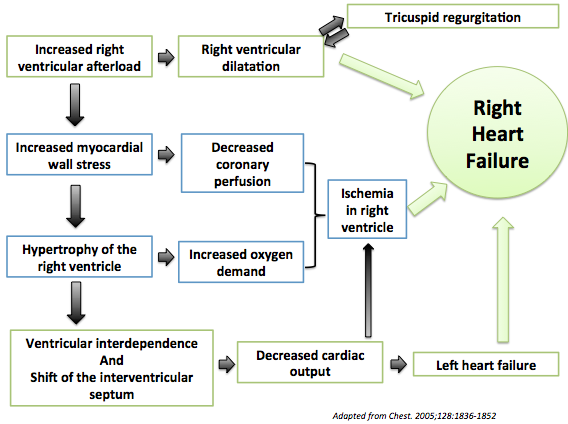
Cardiac Remodeling
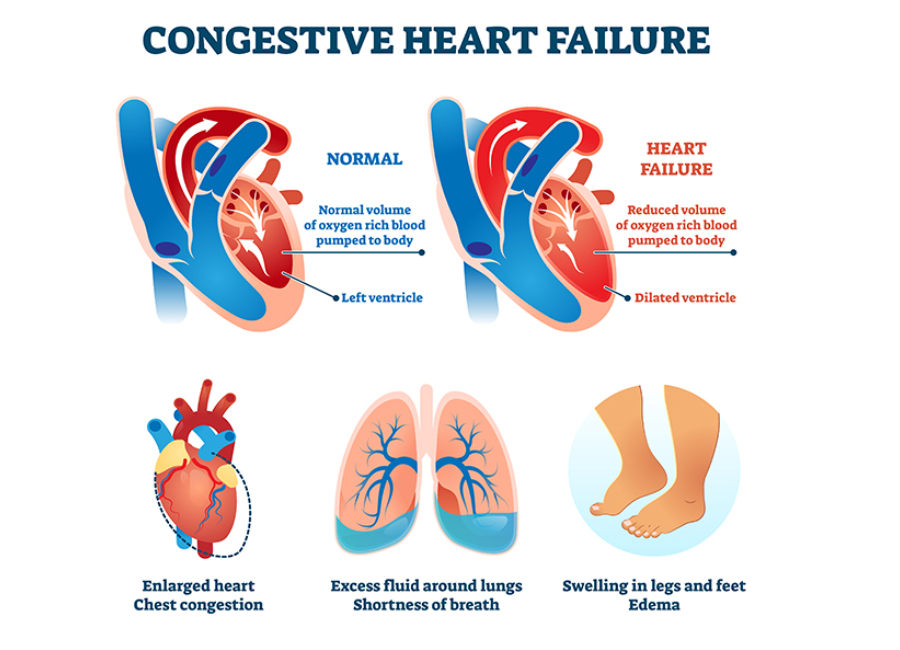
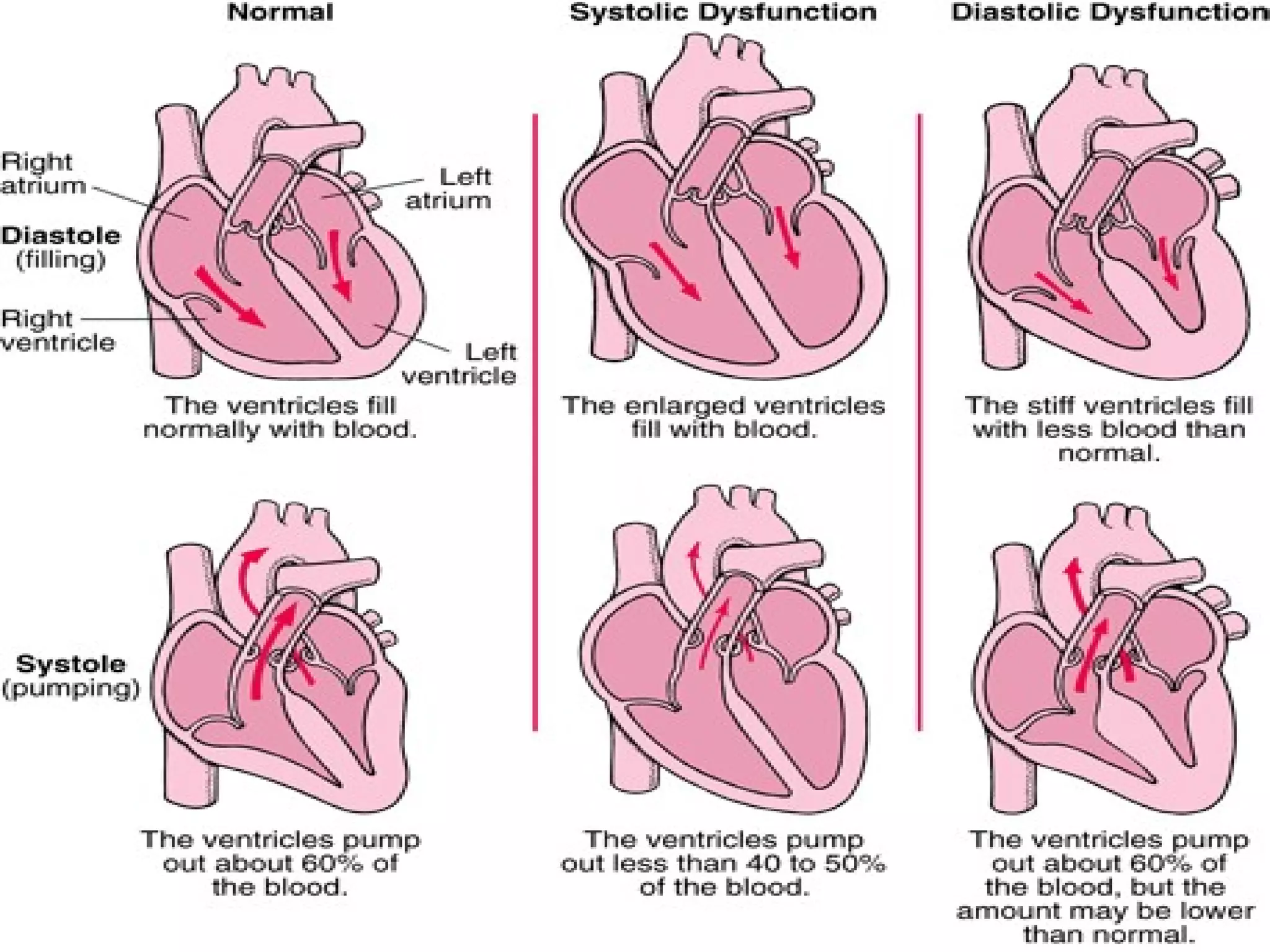
Cardiac remodeling is a key concept in CHF pathophysiology. The heart, in an attempt to compensate for the initial injury, undergoes structural changes.
These changes can include hypertrophy (enlargement of the heart muscle) and changes in the shape of the heart chambers. While initially beneficial, these alterations ultimately worsen the heart's function.
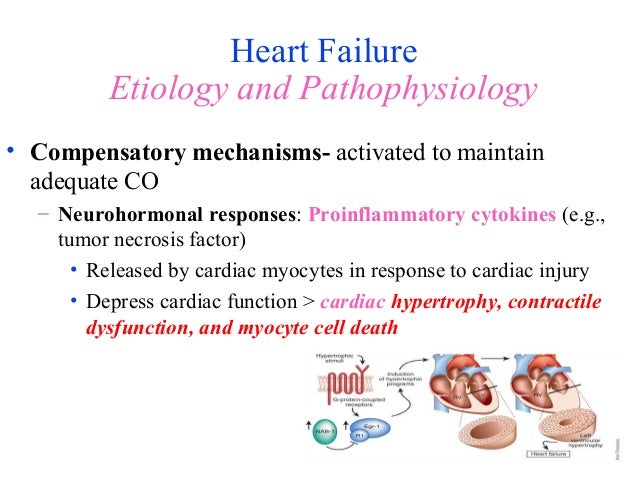
Neurohormonal Activation
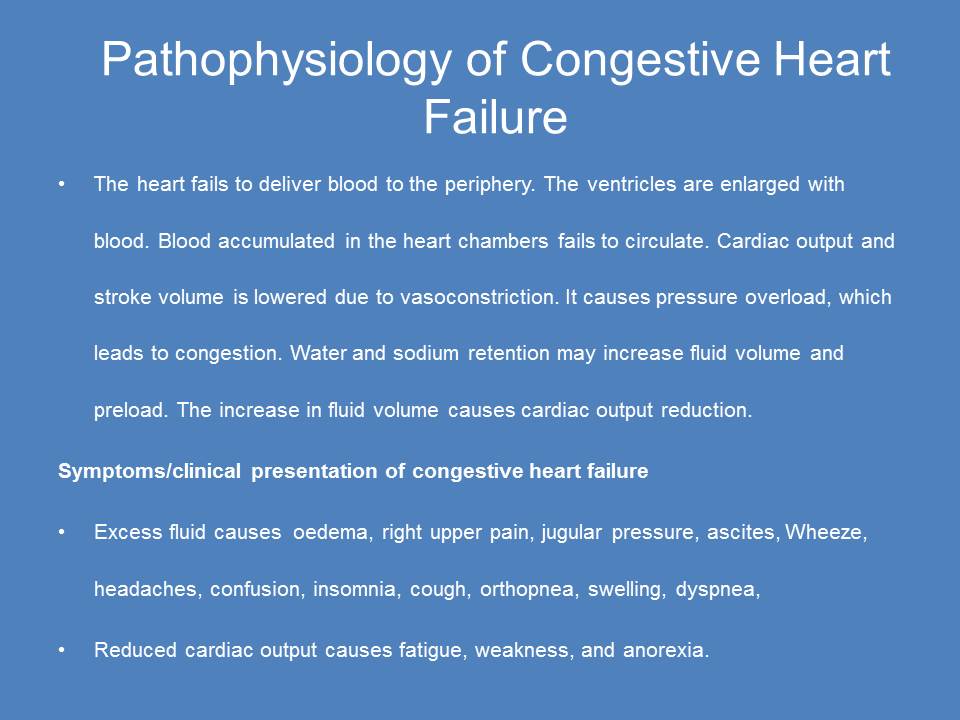
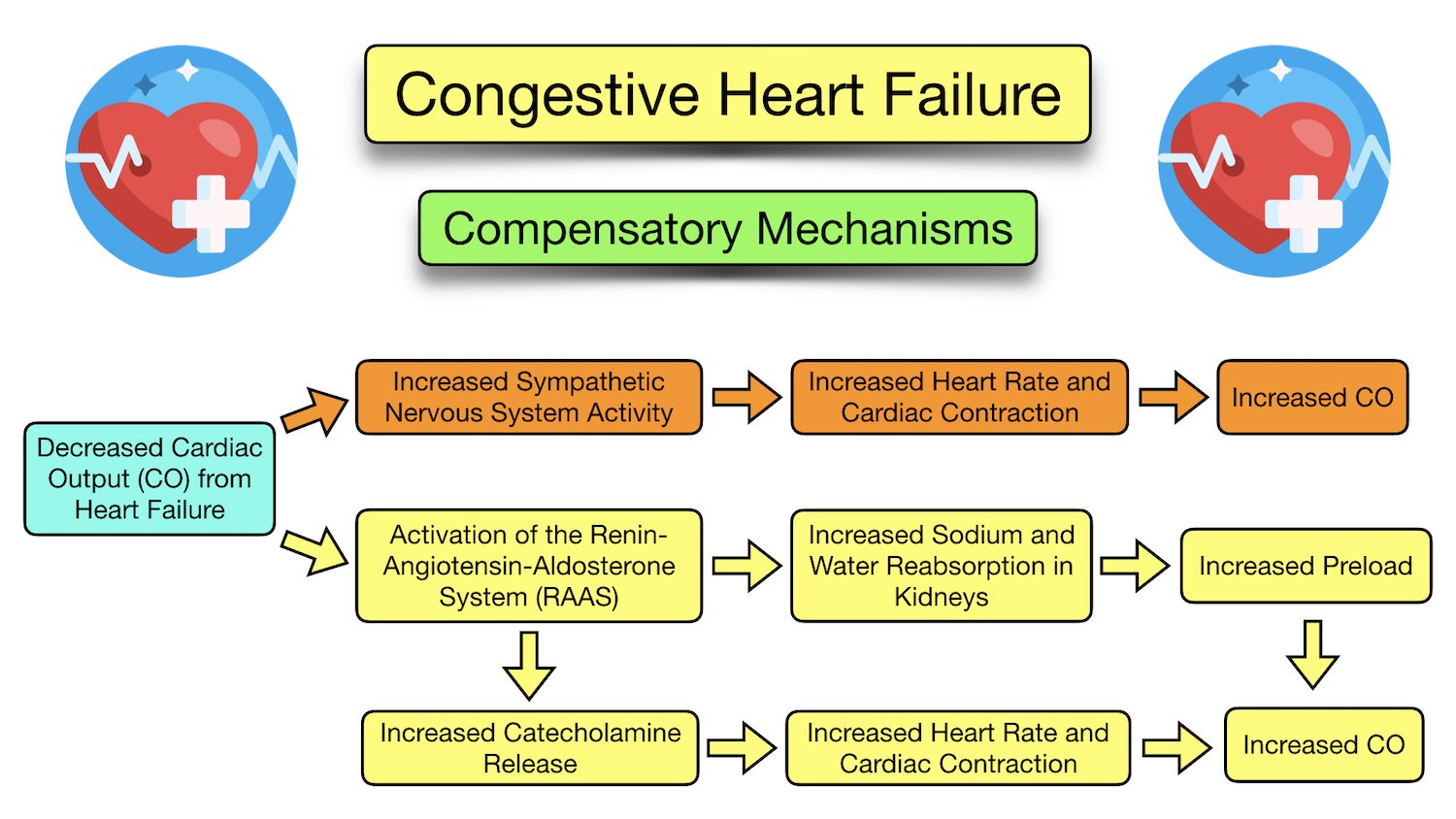
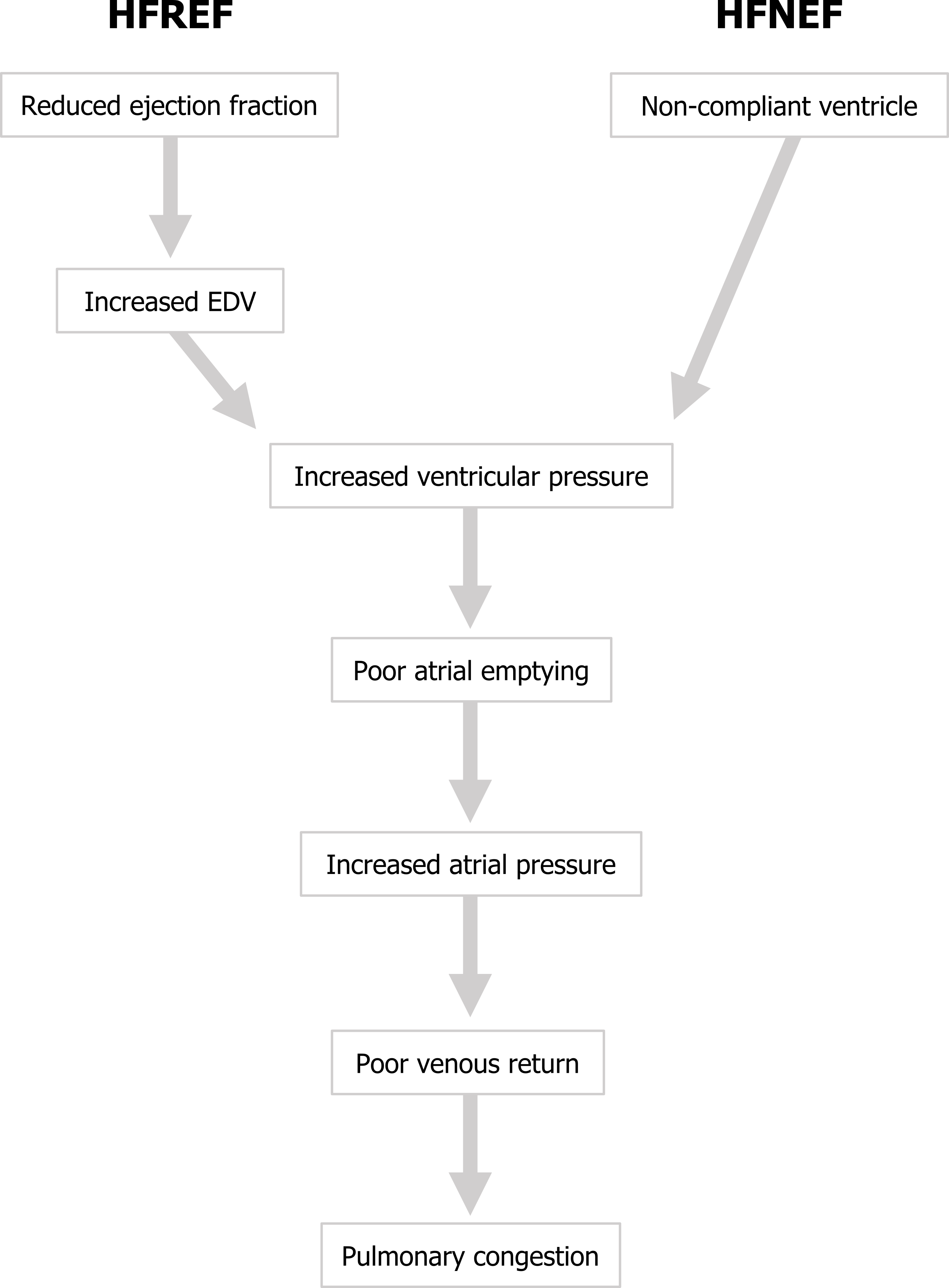
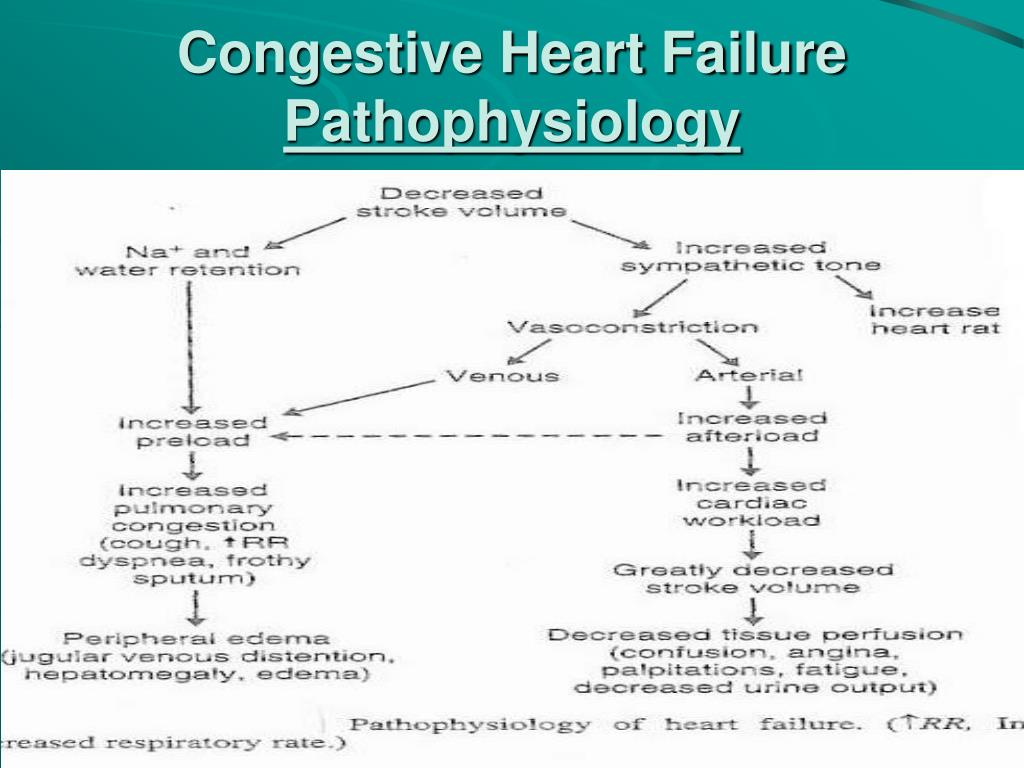
The body responds to reduced cardiac output by activating several neurohormonal systems. These systems, including the renin-angiotensin-aldosterone system (RAAS) and the sympathetic nervous system, are initially designed to maintain blood pressure and blood volume.
However, chronic activation of these systems leads to detrimental effects. It includes increased sodium and water retention, vasoconstriction, and further cardiac remodeling. Medications like ACE inhibitors and beta-blockers target these systems to mitigate their harmful effects.
Cellular and Molecular Changes
At the cellular level, CHF involves a complex interplay of molecular events. These events lead to changes in calcium handling, energy metabolism, and cell survival. The heart's ability to contract and relax properly is impaired.
Researchers are actively investigating these cellular mechanisms to identify new therapeutic targets. These targets can improve cardiac function and prevent further deterioration. Understanding these processes at a molecular level may allow for better treatments.
The Role of Inflammation
Emerging evidence suggests that inflammation plays a significant role in the pathophysiology of CHF. Inflammatory cytokines, released in response to cardiac injury, contribute to myocardial dysfunction and remodeling. This causes a vicious cycle.
Chronic inflammation can exacerbate the progression of heart failure. This is where studies into anti-inflammatory therapies are being looked at.
Clinical Manifestations and Diagnosis
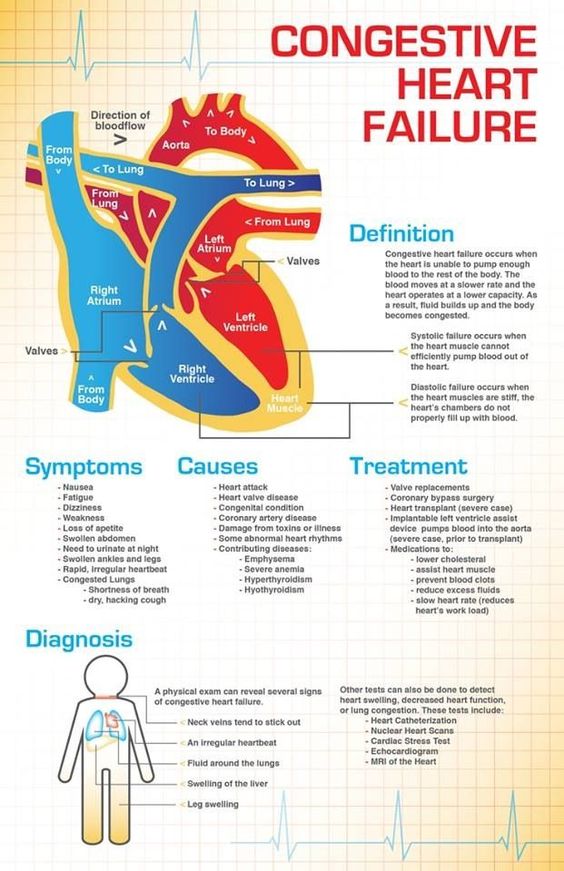
The signs and symptoms of CHF are diverse. They reflect the body's attempt to compensate for the heart's reduced pumping capacity. Common symptoms include shortness of breath, fatigue, swelling in the ankles and feet, and persistent coughing or wheezing.
These symptoms often worsen with exertion. Diagnosis typically involves a combination of physical examination, medical history, and diagnostic tests.
Diagnostic Tools
Echocardiography, an ultrasound of the heart, is a cornerstone of CHF diagnosis. It provides detailed information about the heart's structure, function, and valve integrity.
Other diagnostic tools include electrocardiograms (ECGs), chest X-rays, and blood tests (such as BNP or NT-proBNP levels, which are elevated in heart failure). These tests help assess the severity of CHF and identify underlying causes.
Management and Treatment Strategies
Managing CHF requires a multidisciplinary approach. This approach includes lifestyle modifications, medications, and in some cases, advanced therapies like cardiac resynchronization therapy or heart transplantation.
The goals of treatment are to alleviate symptoms, improve quality of life, and prevent disease progression. Patients are encouraged to adapt heart-healthy behaviors.
Pharmacological Interventions
Medications play a crucial role in managing CHF. ACE inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, and diuretics are commonly prescribed to reduce blood pressure, improve cardiac function, and reduce fluid retention.
Newer medications, such as sodium-glucose cotransporter-2 (SGLT2) inhibitors, have also shown promise in improving outcomes for patients with CHF. The variety of medications now available is encouraging.
Lifestyle Modifications
Lifestyle modifications are an integral part of CHF management. These modifications include adhering to a low-sodium diet, limiting fluid intake, engaging in regular exercise, and quitting smoking. They also include managing weight.
These changes empower patients to take control of their health and improve their overall well-being. Support from family and friends is also important to succeed.
The Future of CHF Research
Research into the pathophysiology of CHF is ongoing and constantly evolving. Scientists are exploring new therapeutic targets, developing novel diagnostic tools, and investigating the role of genetics and personalized medicine.
Advances in regenerative medicine, such as stem cell therapy, hold promise for repairing damaged heart tissue and restoring cardiac function. The progress being made is quite hopeful.
Understanding the pathophysiology of CHF is essential for advancing the field and improving the lives of those affected. As we unravel the complexities of this condition, we pave the way for more effective treatments and better outcomes.
The journey through the intricate landscape of CHF pathophysiology reveals not just the mechanisms of disease, but also the resilience of the human body and the dedication of those striving to understand and combat this condition. While the heart may falter, the pursuit of knowledge and innovative therapies continues to beat strong.