Sciatica Monitoring For Changes Or Improvement

For individuals grappling with the persistent and often debilitating pain of sciatica, monitoring its progression – or regression – is crucial. Recent advancements in both at-home tracking methods and clinical assessment tools are offering new hope for improved management and treatment outcomes. These developments empower patients and healthcare providers to make more informed decisions based on objective data.
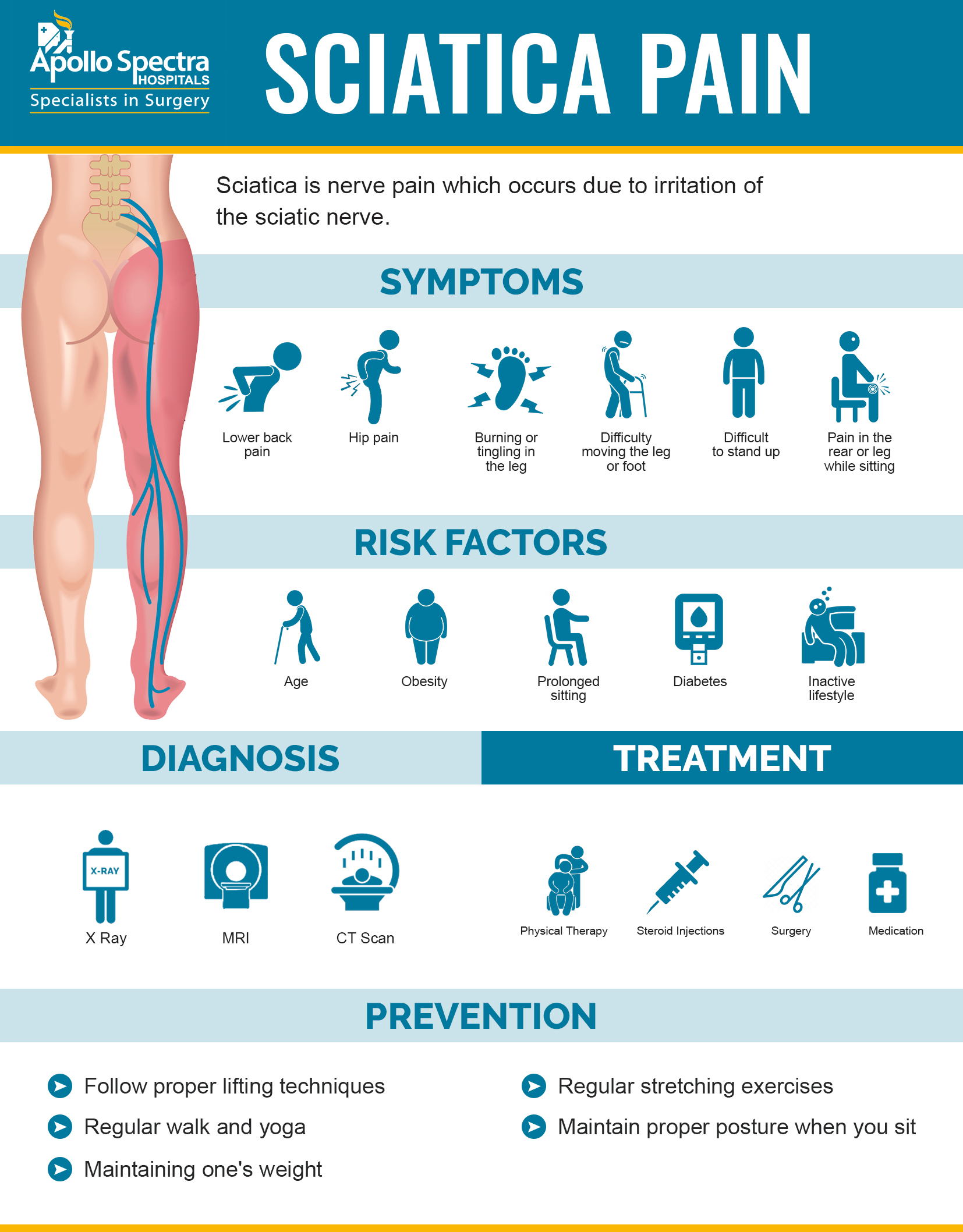
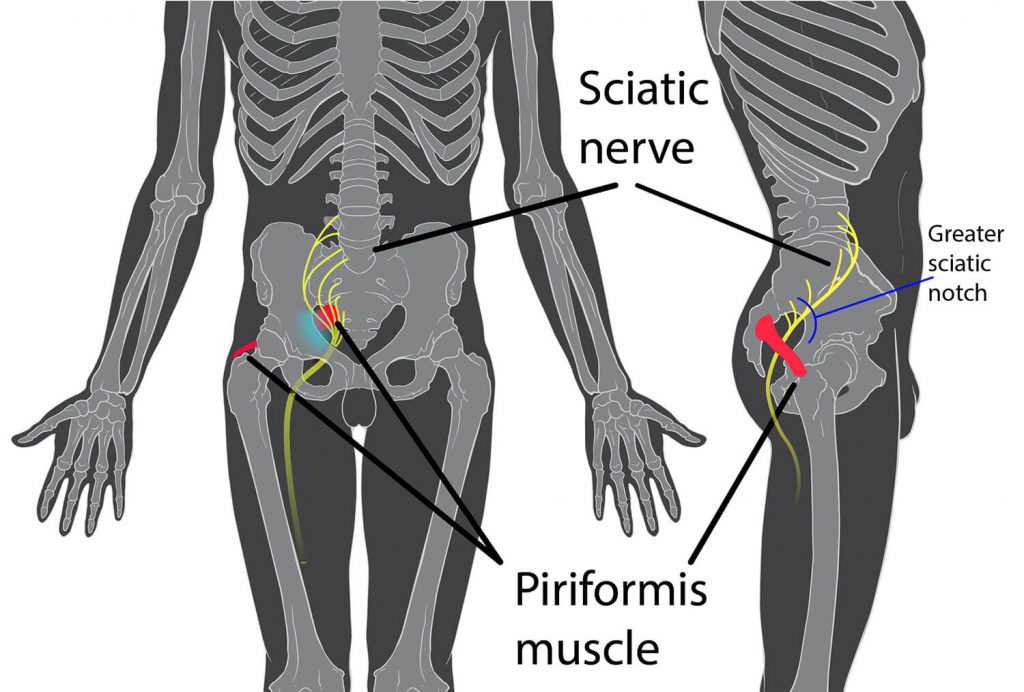
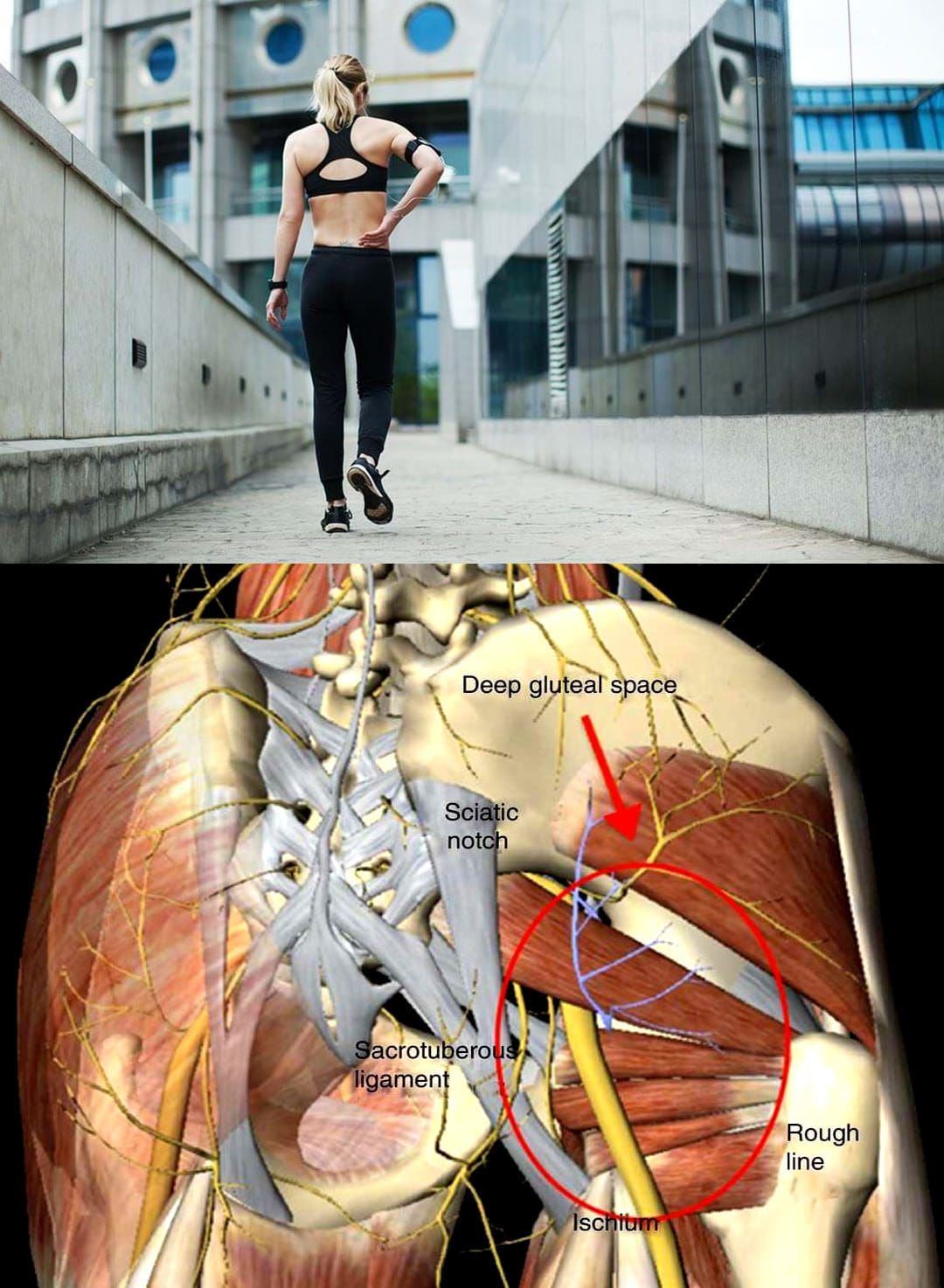
Sciatica, characterized by pain radiating along the sciatic nerve pathway from the lower back down the leg, affects a significant portion of the population. Effective monitoring allows for timely adjustments to treatment plans, potentially preventing chronic pain and improving quality of life. The increased focus on objective assessment represents a shift towards more personalized and data-driven approaches to sciatica care.
Understanding Sciatica Monitoring
Sciatica monitoring involves regularly assessing the severity and characteristics of the pain, as well as its impact on daily function. This includes tracking pain intensity, location, and any associated symptoms like numbness, tingling, or weakness. The aim is to identify trends, detect changes, and evaluate the effectiveness of interventions.
Monitoring is important to understanding when the sciatica is at its peak and at its worst. Without any monitoring it can be difficult to gauge the progression and regression.
Traditionally, monitoring relied heavily on patient self-reporting and subjective assessments during clinical visits. However, advances in technology and a greater emphasis on patient empowerment are leading to more objective and continuous monitoring methods.
At-Home Monitoring Tools
Several at-home monitoring tools are emerging, offering convenient ways to track sciatica symptoms. These tools often include pain diaries, digital questionnaires, and wearable sensors that can measure activity levels and posture.
Mobile apps, for example, allow patients to record their pain levels, activities, and medications, providing a comprehensive overview of their condition over time. Some apps even incorporate guided exercises and educational resources to support self-management.
Wearable sensors, such as accelerometers and gyroscopes, can track movement patterns and identify activities that exacerbate sciatica symptoms. This data can help patients and clinicians understand how daily activities contribute to their pain and adjust their routines accordingly.
Clinical Assessment Techniques
In addition to at-home monitoring, clinical assessments play a crucial role in tracking sciatica. Standard neurological examinations, including reflex tests, strength assessments, and sensory evaluations, help identify nerve compression and dysfunction.
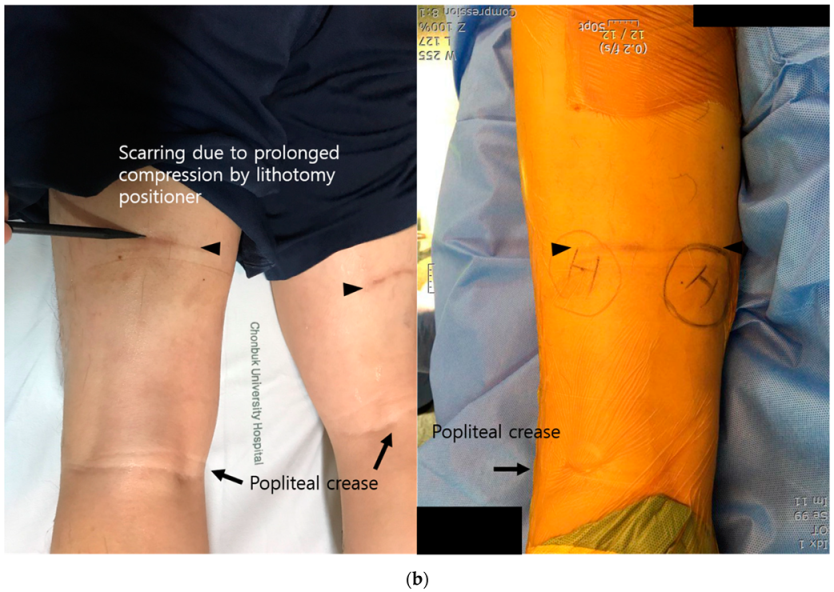
Imaging techniques, such as MRI scans, can visualize the spine and identify structural abnormalities that may be contributing to sciatica. However, these are not typically used for routine monitoring due to cost and potential radiation exposure.
A recent study published in the Journal of Pain Research highlighted the value of combining patient-reported outcomes with objective measures like gait analysis to assess sciatica severity. This approach provides a more comprehensive picture of the condition and its impact on functional abilities.
The Significance of Monitoring Changes
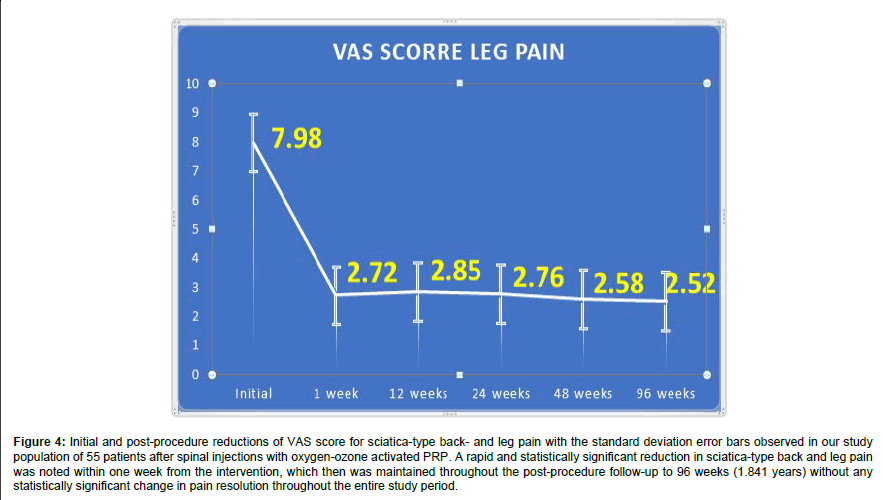
Effective sciatica monitoring allows for early detection of changes in symptoms, whether positive or negative. Identifying improvements in pain or function can reinforce the effectiveness of treatment strategies and encourage continued adherence.
Conversely, detecting worsening symptoms or the development of new complications can prompt timely adjustments to the treatment plan. This may involve modifying medication dosages, adding new therapies, or considering more invasive interventions if conservative approaches fail.
Dr. Anya Sharma, a leading neurologist at the National Institute of Neurological Disorders and Stroke (NINDS), emphasizes the importance of personalized monitoring. "Every patient's experience with sciatica is unique, and a one-size-fits-all approach is rarely effective," she explains. "Regular monitoring allows us to tailor treatment plans to individual needs and optimize outcomes."
Potential Impact and Future Directions
The increased focus on sciatica monitoring has the potential to significantly improve patient care. By providing objective data on treatment effectiveness, monitoring can help reduce reliance on subjective assessments and minimize the risk of inappropriate or ineffective interventions.
Furthermore, monitoring can empower patients to take a more active role in their own care. By tracking their symptoms and understanding the factors that influence their pain, patients can make informed decisions about their lifestyle and treatment choices.
Future research is likely to focus on developing more sophisticated and user-friendly monitoring tools. This includes exploring the use of artificial intelligence (AI) to analyze large datasets of patient information and predict treatment outcomes. AI can find more correlations between large data sets and can predict outcomes that would be difficult for doctors to predict.
Ultimately, the goal of sciatica monitoring is to provide patients with the best possible chance of achieving lasting pain relief and improved function. By embracing a data-driven approach to care, clinicians and patients can work together to optimize treatment strategies and enhance quality of life.
With continuing research and development of new at-home and clinical monitoring tools, the management of sciatica is poised for significant advancements. These advancements will help provide better long-term pain management.