What Are The Disadvantages Of Using Artificial Blood

Imagine a battlefield medic, desperately trying to stabilize a wounded soldier. Every second counts. The familiar bags of blood hang uselessly – the soldier's blood type is unknown, or worse, they're facing a rare blood type shortage. A solution, shimmering with promise, sits nearby: artificial blood. But is this life-saving innovation a silver bullet, or does it come with hidden costs?
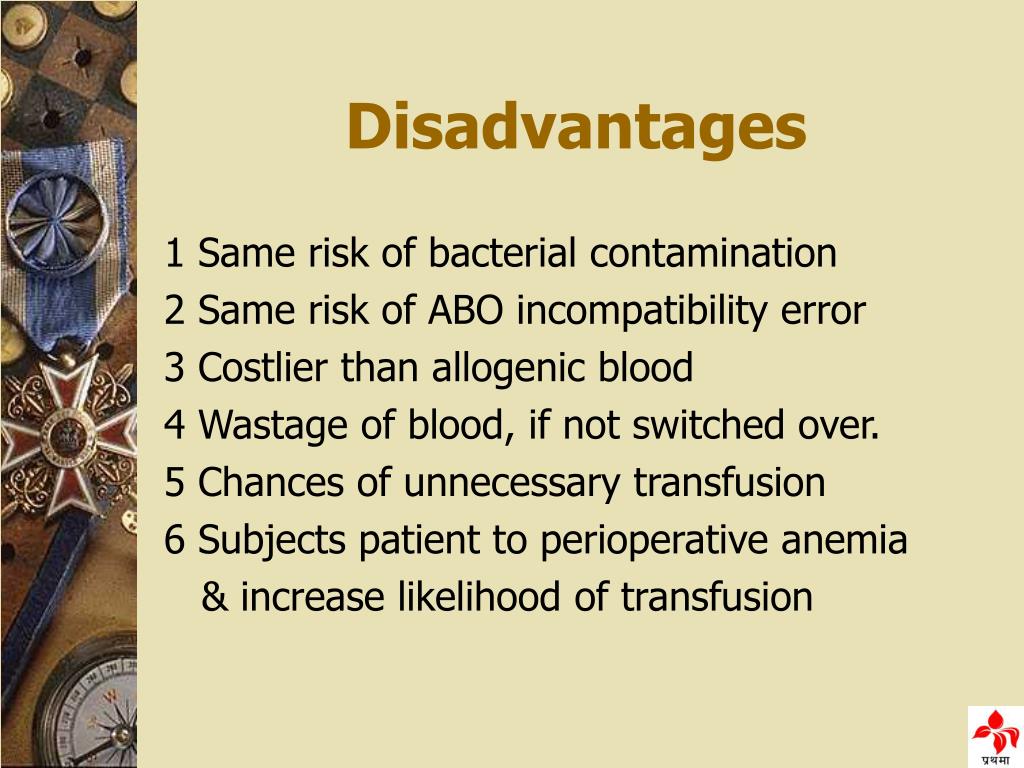
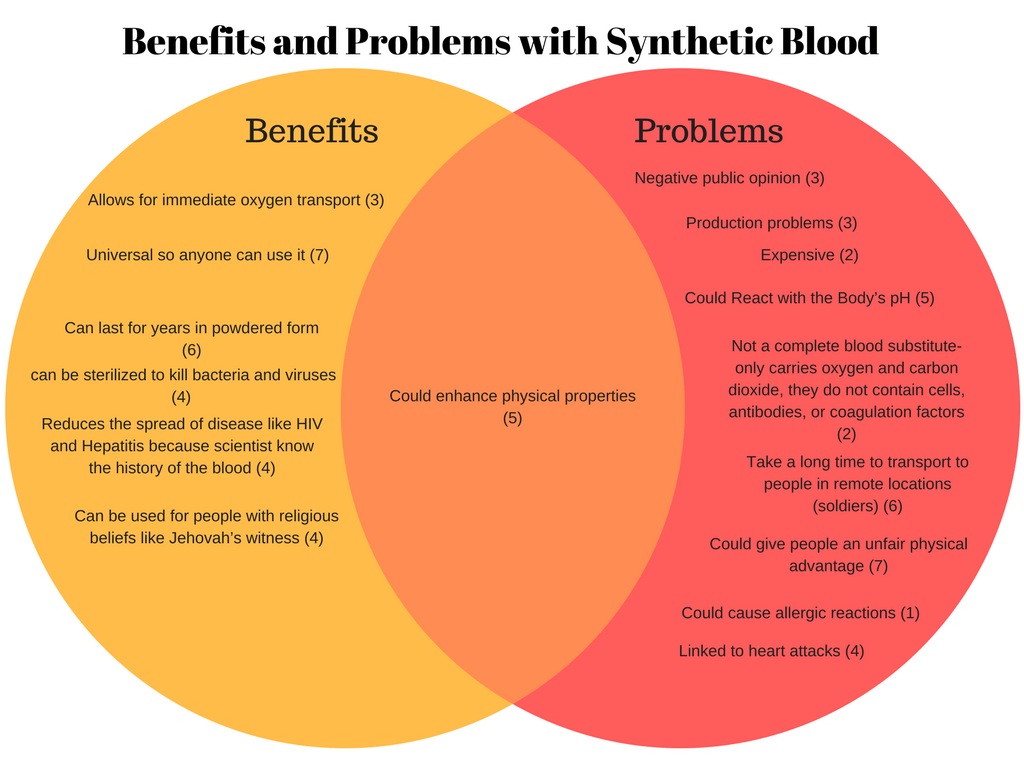
While the development of artificial blood presents a potentially revolutionary advancement in medicine, overcoming critical blood shortages and transfusion limitations, it's crucial to understand that this technology is not without its challenges. The disadvantages, ranging from potential toxicity and immune responses to complex manufacturing processes and limited oxygen-carrying capacity, need careful consideration before widespread adoption can occur.
The Promise and the Peril: A History of Blood Substitutes
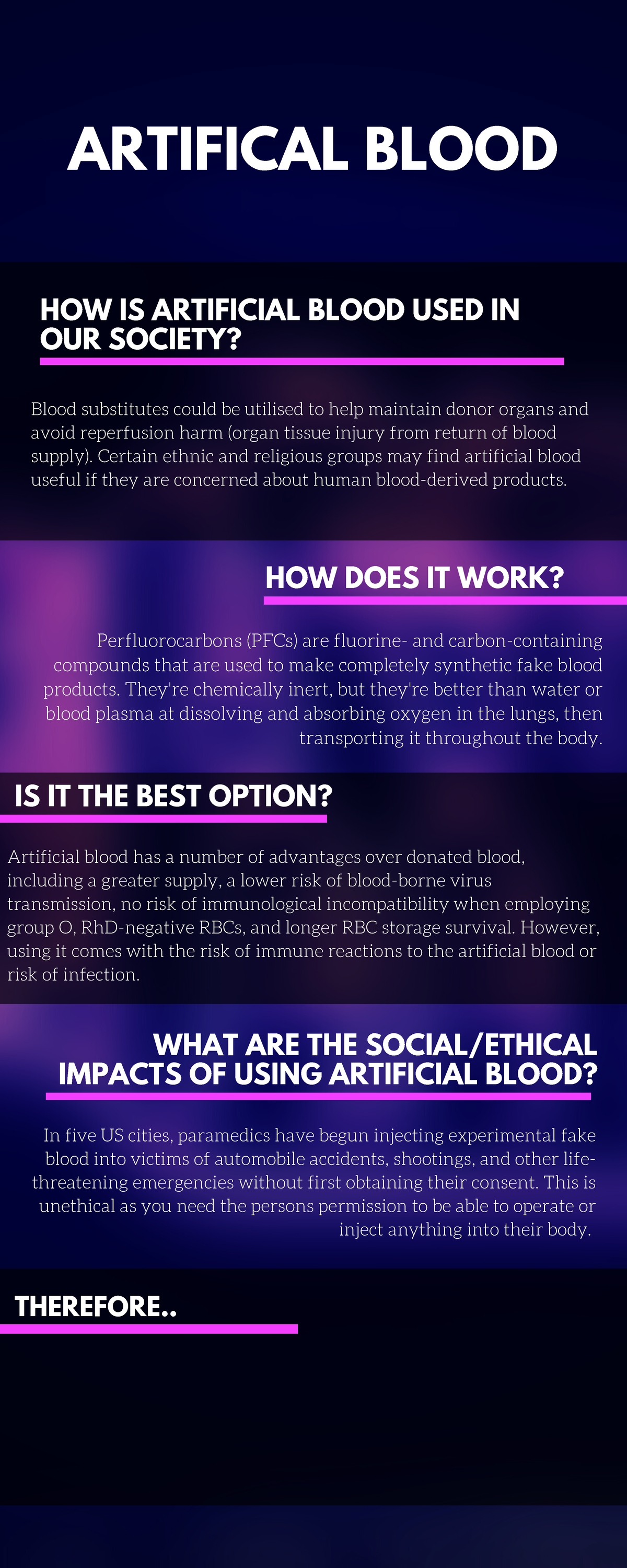
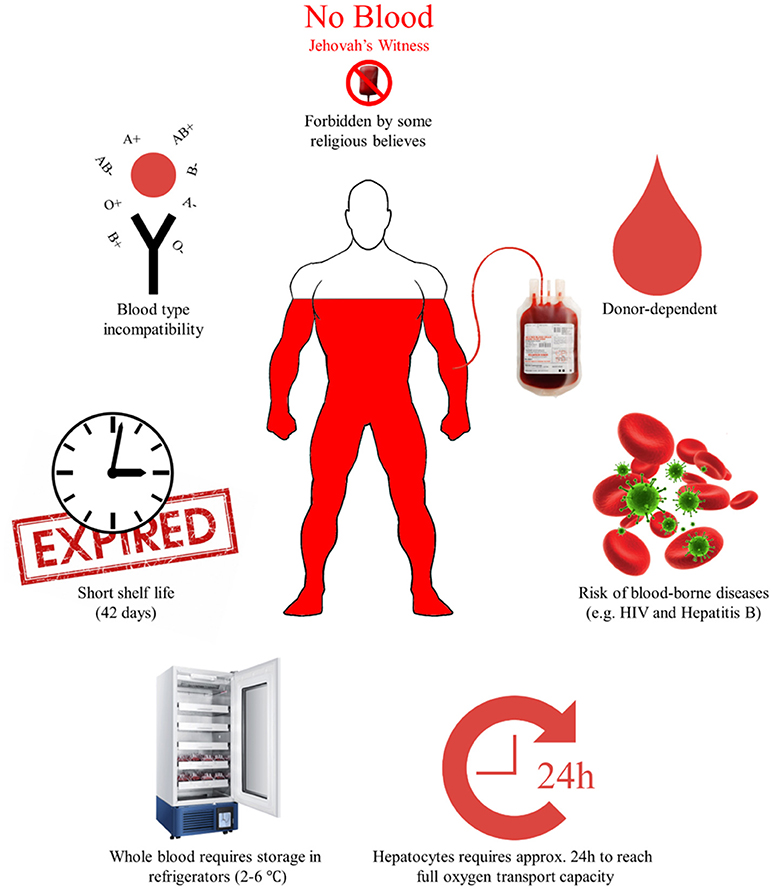
The quest for artificial blood has been ongoing for decades, driven by the urgent need to address the limitations of human blood transfusions. The risks associated with traditional blood, such as infections, transfusion reactions, and logistical challenges in sourcing and storing compatible blood types, are well documented.
Early research focused on two main types of blood substitutes: perfluorocarbons (PFCs) and hemoglobin-based oxygen carriers (HBOCs). PFCs are synthetic inert chemicals with a high capacity to dissolve oxygen. HBOCs, on the other hand, utilize hemoglobin extracted from human or animal blood, or produced through recombinant technology.
These carriers are then modified to increase their stability and compatibility within the body. The initial optimism surrounding these blood substitutes, however, was tempered by a series of clinical trials that revealed unexpected and sometimes severe side effects.
Navigating the Downsides: What Makes Artificial Blood Risky?
One of the most significant concerns surrounding artificial blood is its potential for toxicity. PFCs, for instance, can persist in the body for extended periods, accumulating in organs like the liver and spleen. This accumulation may lead to long-term health consequences, although the full extent of these effects is still under investigation.
HBOCs, despite their promise, have been linked to vasoconstriction – the narrowing of blood vessels. This effect can lead to increased blood pressure and reduced blood flow to vital organs, potentially exacerbating the condition of patients already in critical condition.
Furthermore, some HBOCs have been associated with an increased risk of heart attack and stroke in certain patient populations. Researchers are actively working to modify the structure of hemoglobin to minimize these vasoactive effects.
Another critical consideration is the potential for triggering immune responses. Although artificial blood is designed to be compatible with all blood types, the body's immune system can still recognize it as foreign and mount an attack. This immune response can manifest as inflammation, fever, and other adverse reactions, potentially negating the benefits of the blood substitute.
The development of immunologically inert artificial blood remains a significant challenge, requiring sophisticated engineering and meticulous testing.
The Oxygen-Carrying Conundrum
While PFCs and HBOCs can carry oxygen, their oxygen-carrying capacity is often lower than that of natural blood. This limitation means that larger volumes of artificial blood may be required to deliver the same amount of oxygen to the tissues, potentially placing a strain on the circulatory system.
Moreover, the efficiency of oxygen delivery from artificial blood to the tissues can be affected by various factors, such as blood flow rate and the presence of other medical conditions. Researchers are exploring strategies to enhance the oxygen-carrying capacity and delivery efficiency of artificial blood, including the use of nanoparticles and other advanced materials.
The development of nano-based oxygen carriers promises greater oxygen-carrying capacity and targeted delivery, but faces challenges in terms of biocompatibility and long-term safety.
Manufacturing Complexities and Cost
The manufacturing of artificial blood is a complex and expensive process. The synthesis of PFCs requires specialized equipment and expertise, while the production of HBOCs involves careful extraction, purification, and modification of hemoglobin.
Scaling up production to meet potential demand presents a significant logistical and financial challenge. The high cost of artificial blood could limit its accessibility, particularly in resource-poor settings where the need for blood substitutes is often greatest.
Furthermore, the storage and handling requirements for artificial blood can be demanding, potentially requiring specialized equipment and trained personnel. The development of cost-effective and easily scalable manufacturing processes is essential for the widespread adoption of artificial blood.
Ethical Considerations and Regulatory Hurdles
The use of artificial blood raises important ethical considerations. For instance, the potential for unforeseen side effects necessitates careful informed consent and robust monitoring during clinical trials.
Furthermore, the allocation of scarce resources, particularly in the early stages of development, requires careful prioritization and transparency. The regulatory pathway for artificial blood is also complex, requiring rigorous safety and efficacy testing before approval can be granted.
Agences like the Food and Drug Administration (FDA) play a crucial role in ensuring that artificial blood products meet stringent standards before they can be made available to the public.
Looking Ahead: A Cautious Optimism
Despite the challenges, research on artificial blood continues to advance, driven by the compelling need for a safe and readily available alternative to human blood. Ongoing studies are focusing on addressing the limitations of existing blood substitutes, developing new and improved formulations, and exploring novel approaches to oxygen delivery.
Areas of active research include the development of bio-compatible polymers, the use of stem cells to generate red blood cells, and the engineering of artificial blood with enhanced oxygen-carrying capacity and reduced toxicity.
The future of artificial blood hinges on overcoming these challenges and demonstrating its safety, efficacy, and cost-effectiveness in clinical trials. While artificial blood may not be a perfect replacement for natural blood, it holds the potential to save lives in situations where conventional blood transfusions are not possible or practical.
The path forward requires continued research, rigorous testing, and a commitment to addressing the ethical and practical considerations associated with this promising but complex technology. The development of artificial blood is a marathon, not a sprint, and success will depend on sustained effort and collaboration among scientists, clinicians, and policymakers.