What Can I Take For Bv Besides Flagyl

Women experiencing bacterial vaginosis (BV) often face a frustrating situation: needing effective treatment alternatives to the commonly prescribed antibiotic, Flagyl (metronidazole), due to side effects, resistance, or personal preference.
This article explores alternative treatment options for BV beyond Flagyl, focusing on evidence-based solutions and addressing the pressing need for diverse management strategies.
Understanding the Need for Alternatives
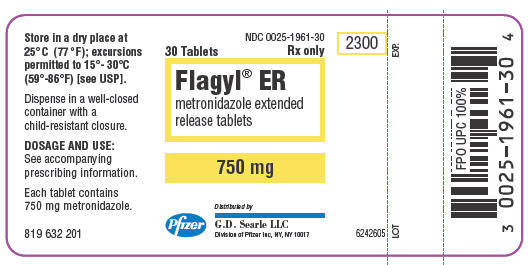
Flagyl, while effective for many, isn't a perfect solution. Common side effects include nausea, metallic taste, and digestive upset, impacting adherence and quality of life.
Moreover, some women experience recurrent BV even after Flagyl treatment, suggesting potential resistance or the need for a more comprehensive approach.
Alternative Antibiotic Treatments
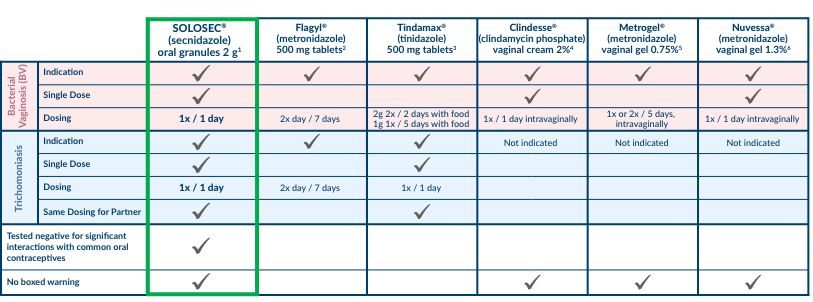
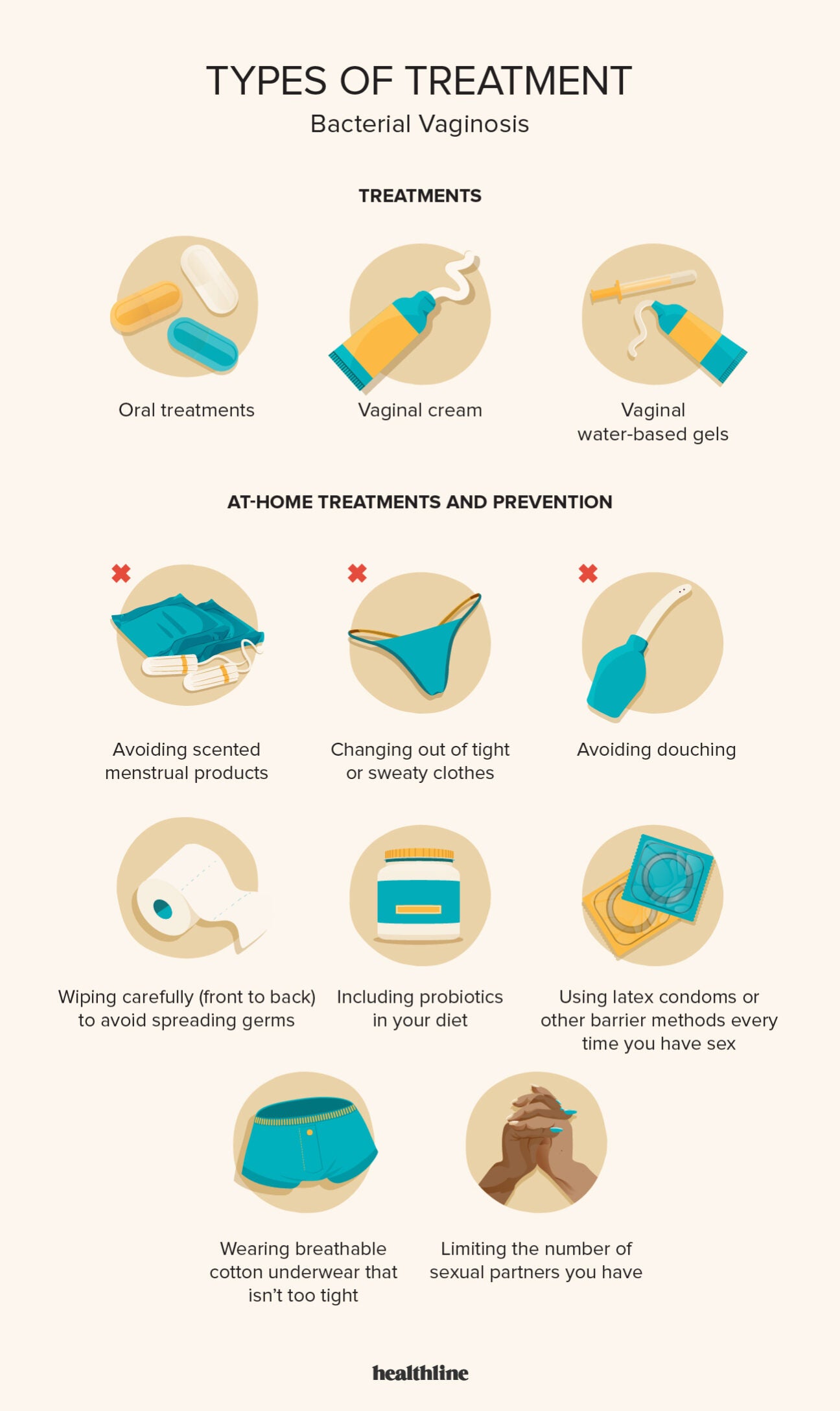
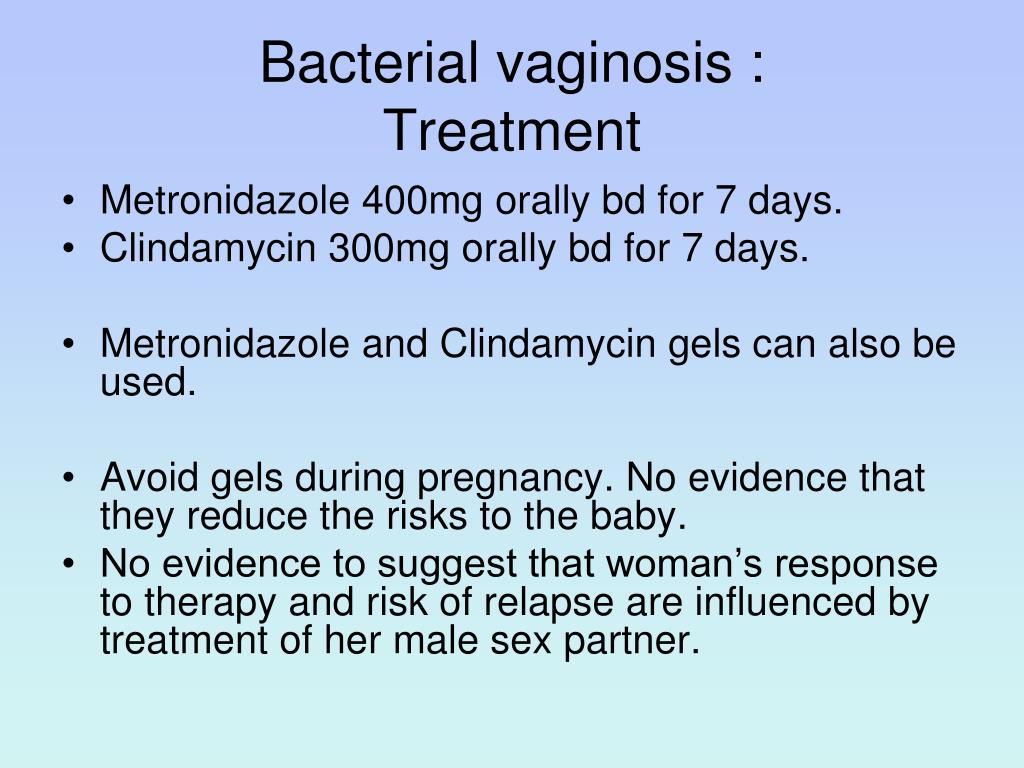
Clindamycin is another antibiotic frequently prescribed for BV. It's available as a cream or oral medication.
Research suggests clindamycin is generally as effective as Flagyl. It could be a suitable option for those unable to tolerate metronidazole.
Another option is Secnidazole, a single-dose oral antibiotic. It offers a convenient treatment schedule compared to the multi-day regimens of Flagyl and clindamycin.
Non-Antibiotic Treatments and Prevention Strategies
While antibiotics target the bacteria causing BV, other approaches focus on restoring a healthy vaginal microbiome. These include the use of probiotics.
Probiotics containing Lactobacillus strains aim to re-establish beneficial bacteria in the vagina. This can help to prevent recurrence.
Some studies show that using probiotics, either orally or vaginally, can be effective in managing BV. Look for products specifically formulated for vaginal health.
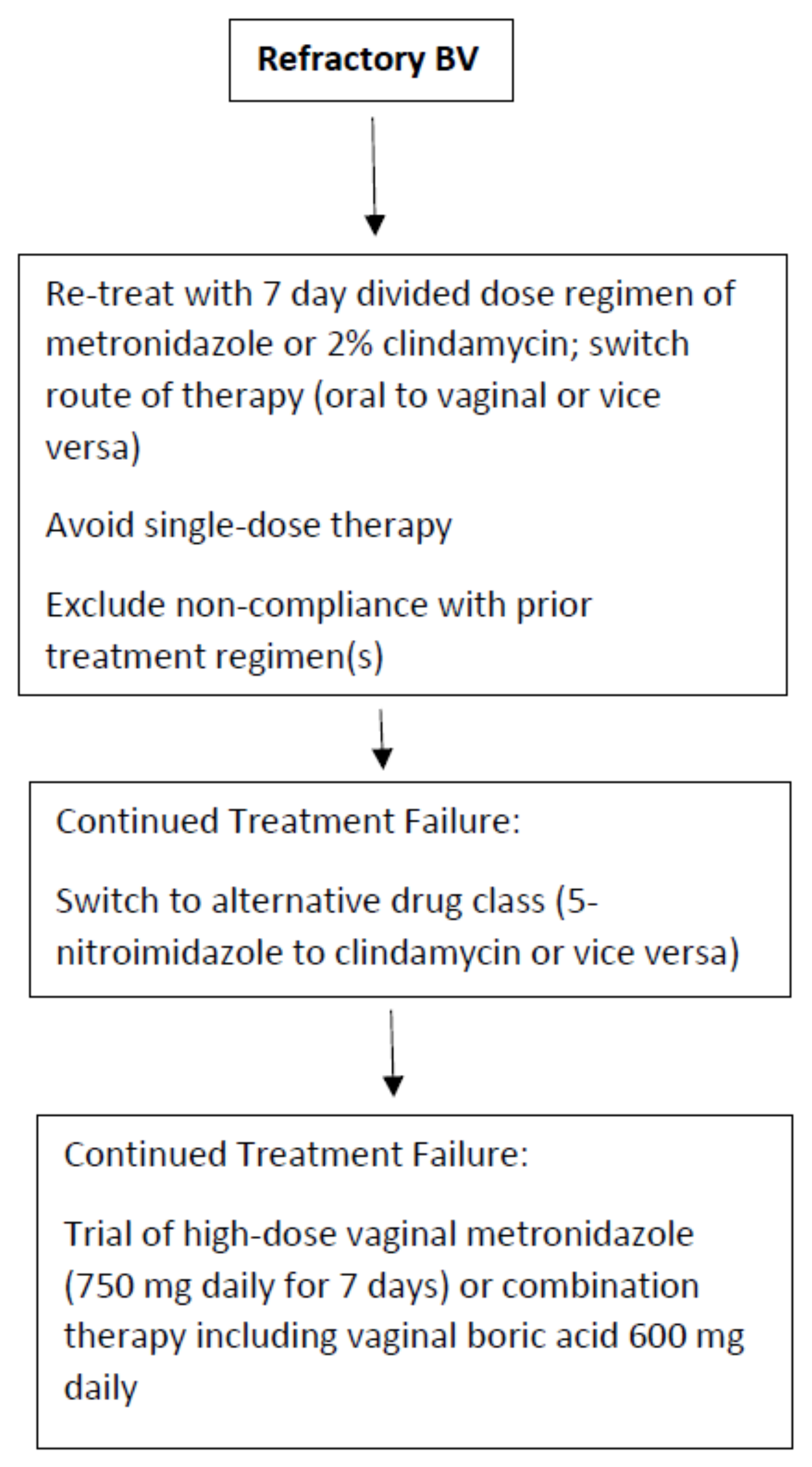
Boric acid suppositories are another non-antibiotic option. They can help to normalize the vaginal pH, creating an environment less favorable to harmful bacteria.
However, boric acid is for vaginal use only and should not be ingested. It is also not safe for pregnant women.
Lifestyle Modifications and Preventive Measures
Beyond treatment, lifestyle changes play a vital role in preventing BV recurrence. This includes practicing good hygiene and avoiding douching.
Douching disrupts the natural balance of bacteria in the vagina. That increased the risk of BV.
Wearing breathable cotton underwear can also help. It reduces moisture and creating a less hospitable environment for bacteria.
Safe sex practices, such as using condoms, are crucial. BV can be associated with sexual activity, although it's not strictly a sexually transmitted infection (STI).
When to Seek Medical Advice
It's essential to consult a healthcare provider for proper diagnosis and treatment of BV. Self-treating can mask underlying conditions or lead to ineffective management.
A doctor can determine the most appropriate treatment plan based on individual circumstances. This plan takes into account medical history and potential drug interactions.
If symptoms persist despite treatment, further evaluation is necessary. This might involve testing for other infections or exploring alternative treatment strategies.
Ongoing Research and Future Directions
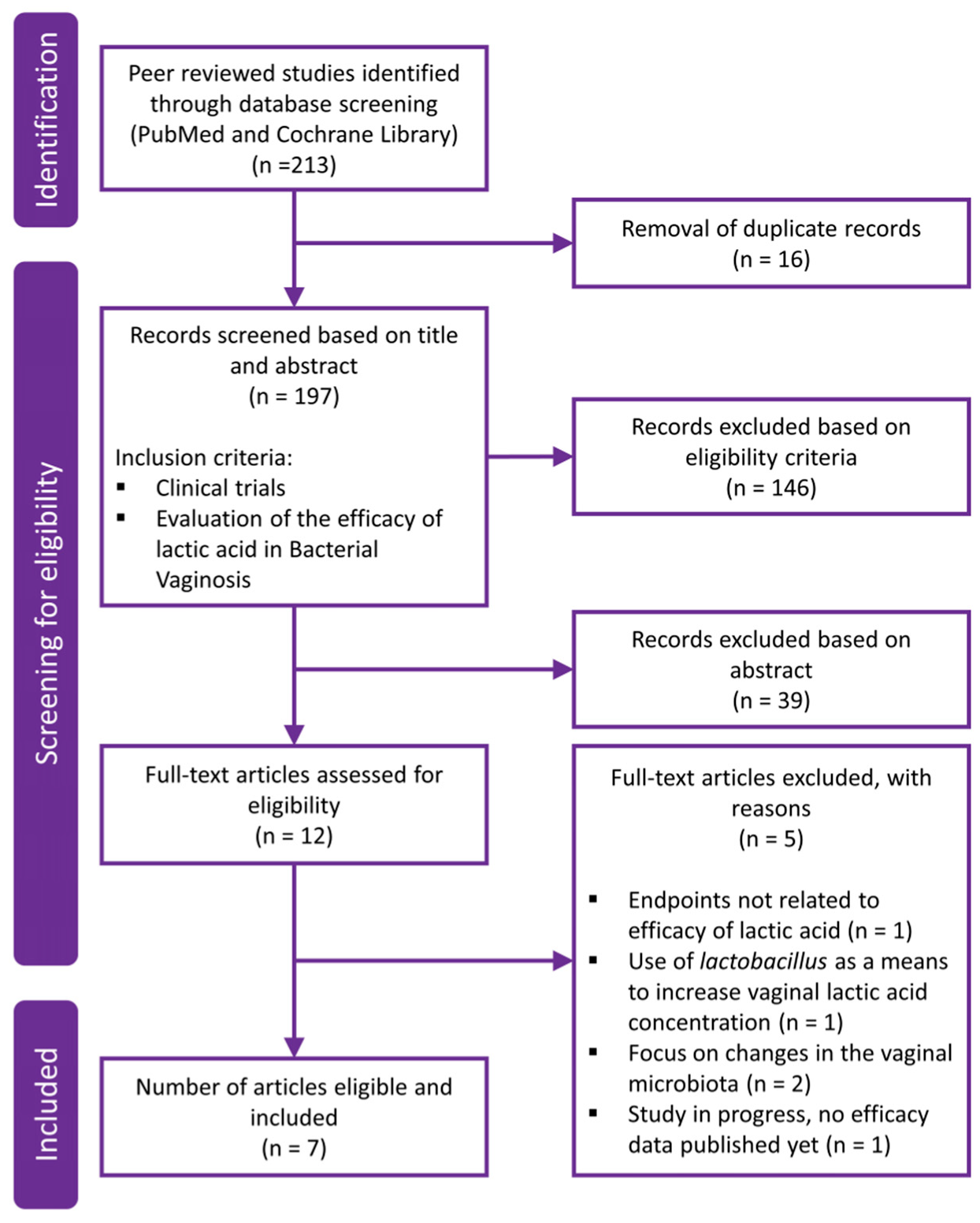
Research continues to explore novel approaches for BV treatment and prevention. This includes investigating new probiotic strains and exploring the role of the vaginal microbiome in women's health.
Stay informed about the latest advancements in BV management. This ensures access to the most effective and evidence-based strategies.
Talk to your doctor. Your doctor can help to develop a personalized approach to address your specific needs.