What Effect Would A Decreased Hematocrit Have On Blood Flow
Urgent reports indicate a significant link between decreased hematocrit levels and altered blood flow, raising concerns among medical professionals. Reduced hematocrit, the percentage of red blood cells in blood, directly impacts blood viscosity and oxygen delivery, potentially leading to severe complications.
This article breaks down the critical effects of lowered hematocrit on blood flow, detailing the mechanisms, consequences, and what healthcare providers are doing to mitigate these risks.
Understanding Hematocrit and Blood Flow
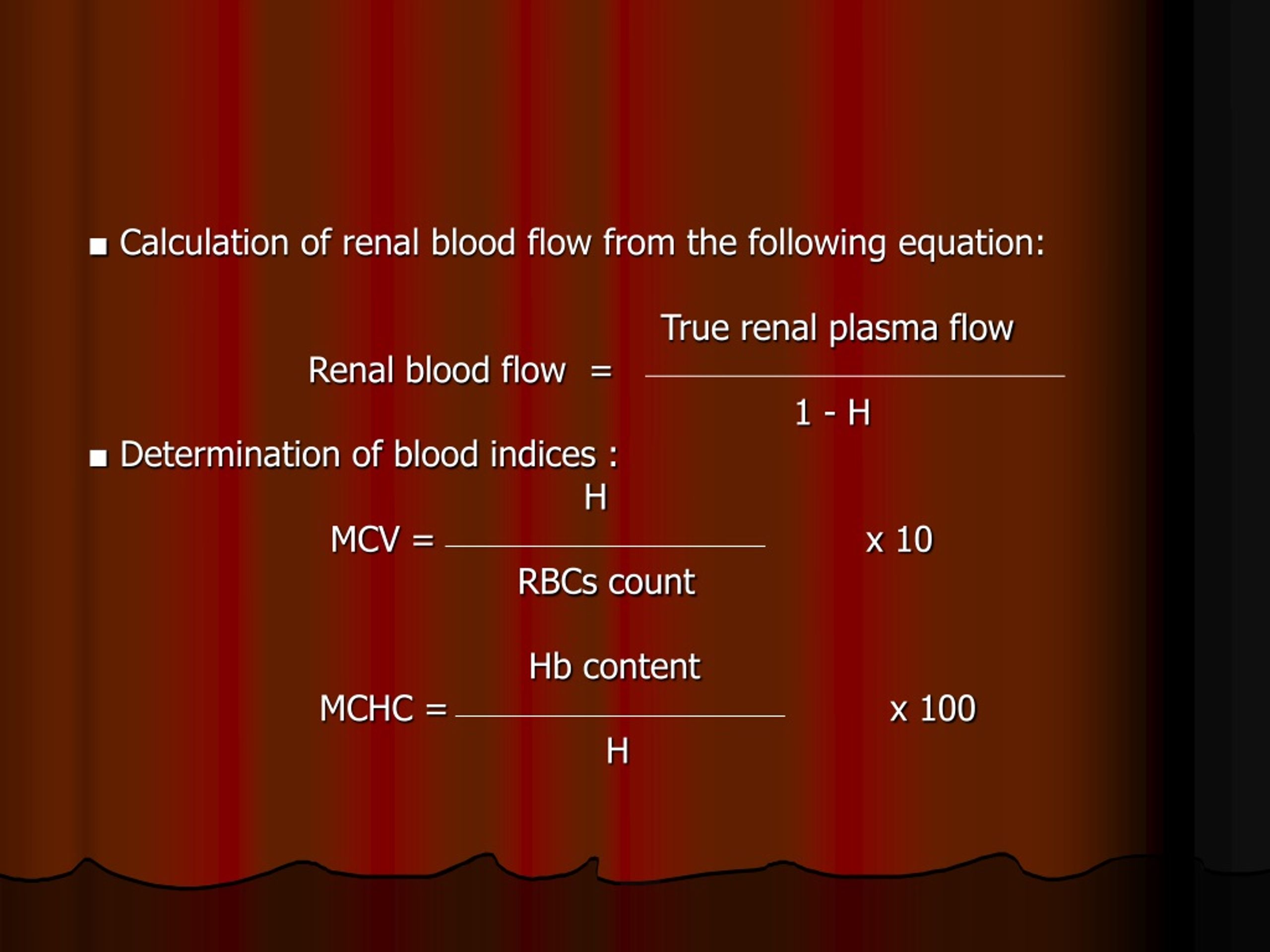
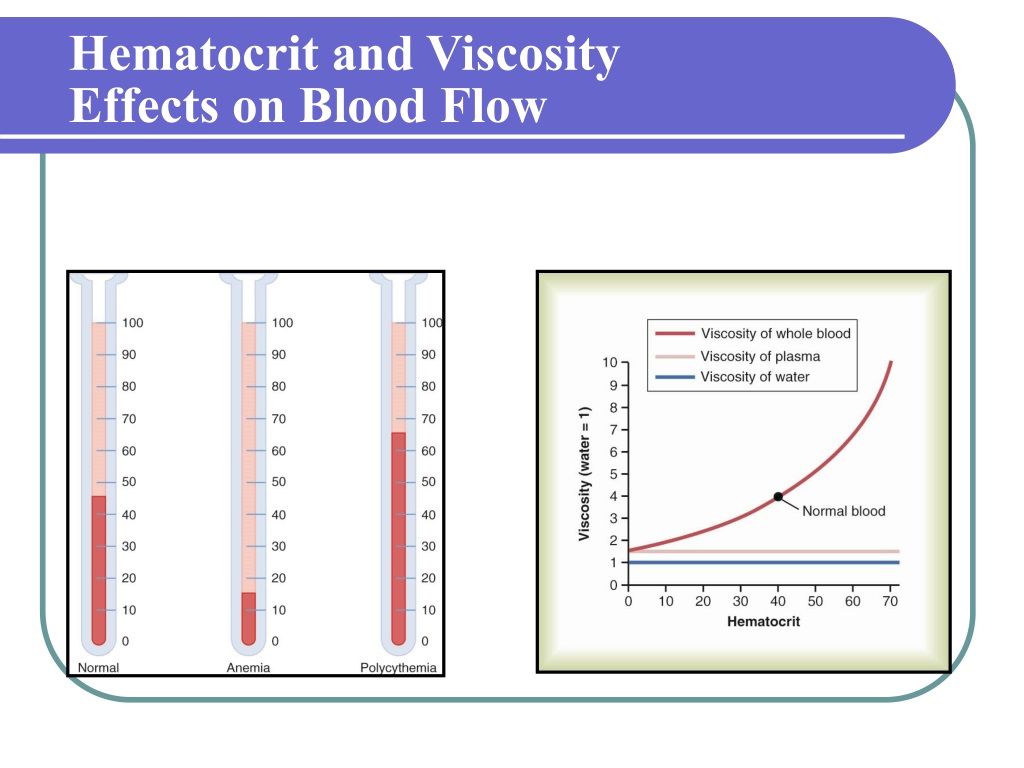
Hematocrit is a crucial blood measurement reflecting the proportion of red blood cells to total blood volume. A typical hematocrit range is 38.3-48.6% for men and 35.5-44.9% for women.
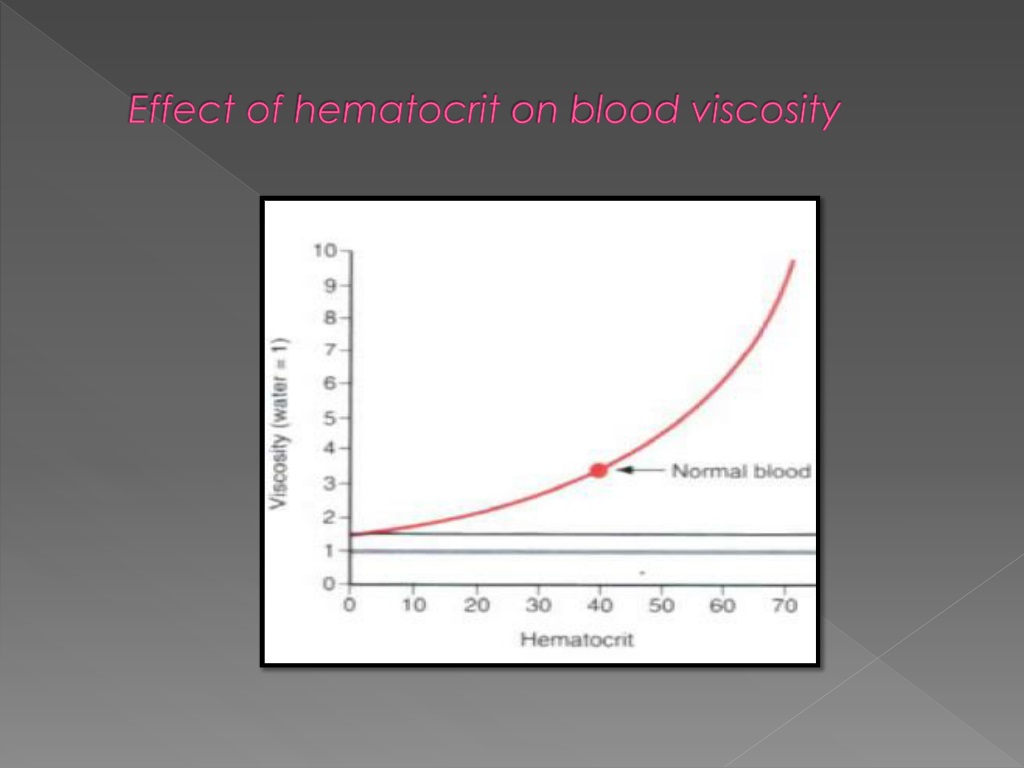
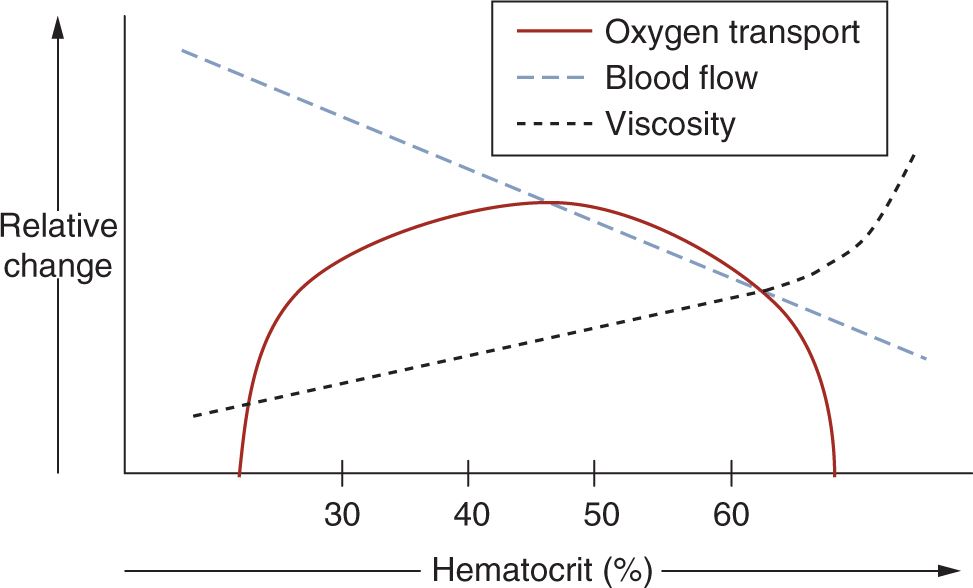
When hematocrit decreases, blood becomes less viscous, altering how it flows through the circulatory system. This change impacts oxygen transport and overall cardiovascular function.
The Impact on Blood Viscosity
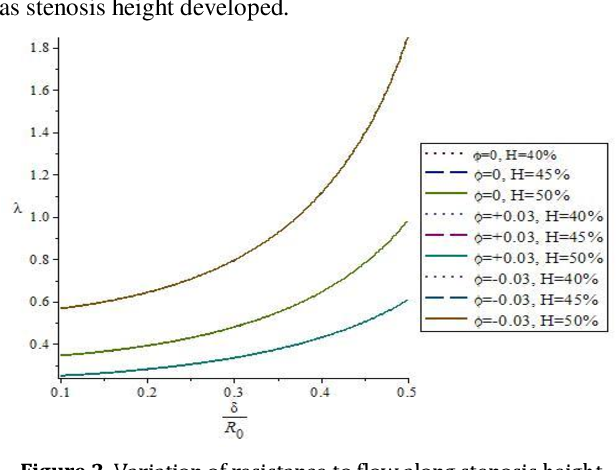
Blood viscosity is a key determinant of blood flow resistance.
A lower hematocrit reduces the number of red blood cells, leading to decreased viscosity and potentially turbulent blood flow. This can impair efficient oxygen delivery to tissues and organs.
Oxygen Delivery Concerns
Red blood cells are essential for carrying oxygen from the lungs to the body's tissues.
With fewer red blood cells due to decreased hematocrit, the oxygen-carrying capacity of blood diminishes. This can result in tissue hypoxia, particularly in active or metabolically demanding organs.
Specific Physiological Effects
Decreased hematocrit can manifest in various physiological alterations.
These include altered cardiac output, changes in blood pressure, and potential damage to the endothelium.
Cardiac Output Adjustments
The heart may compensate for reduced oxygen-carrying capacity by increasing cardiac output.
This compensation may lead to increased heart rate and stroke volume to maintain adequate oxygen supply. Chronic elevation in cardiac output can strain the heart, leading to complications.
Blood Pressure Changes
Blood pressure regulation is also affected by alterations in hematocrit.
Reduced viscosity may initially lower blood pressure, but compensatory mechanisms can lead to fluctuations. Maintaining stable blood pressure becomes challenging with significantly altered hematocrit levels.
Endothelial Impact
The endothelium, the inner lining of blood vessels, is susceptible to damage from altered blood flow.
Turbulent flow caused by decreased viscosity can promote endothelial dysfunction and inflammation, increasing the risk of atherosclerosis and other vascular diseases.
Who is Affected?
Individuals with certain medical conditions or undergoing specific treatments are more prone to decreased hematocrit.
These include patients with anemia, kidney disease, chemotherapy recipients, and those experiencing blood loss from trauma or surgery.
Anemia
Anemia, characterized by low red blood cell count or hemoglobin, is a common cause of decreased hematocrit. Iron deficiency anemia, vitamin deficiency anemia, and anemia of chronic disease are examples that directly impact hematocrit levels.
Kidney Disease
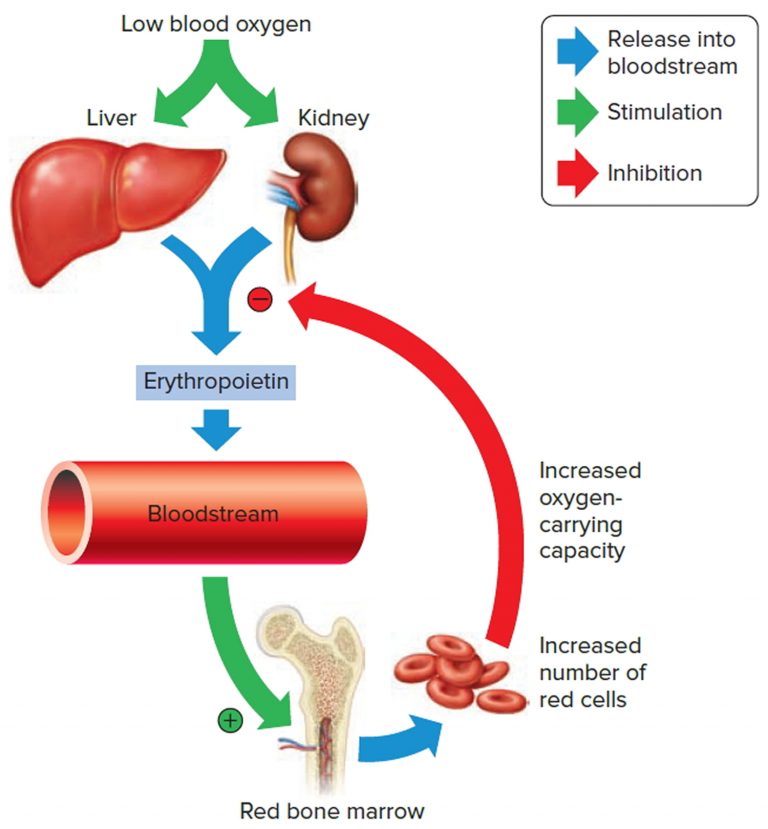
The kidneys produce erythropoietin, a hormone that stimulates red blood cell production.
In kidney disease, erythropoietin production is often impaired, leading to decreased hematocrit and subsequent effects on blood flow and oxygen delivery. Patients with chronic kidney disease frequently require erythropoietin-stimulating agents to manage their anemia.
Chemotherapy
Chemotherapy drugs can suppress bone marrow function, resulting in reduced red blood cell production.
This often leads to anemia and decreased hematocrit. Managing anemia during chemotherapy involves blood transfusions and erythropoiesis-stimulating agents to maintain adequate oxygenation and reduce the impact on blood flow.
Mitigation Strategies
Healthcare providers employ various strategies to mitigate the effects of decreased hematocrit on blood flow and tissue oxygenation.
These include blood transfusions, iron supplementation, and erythropoiesis-stimulating agents.
Blood Transfusions
Blood transfusions are used to rapidly increase hematocrit and oxygen-carrying capacity.
They are typically reserved for severe cases of anemia with significant symptoms. Transfusions can quickly improve oxygen delivery to tissues, but they also carry risks, including transfusion reactions and infections.
Iron Supplementation
Iron supplementation is a common treatment for iron deficiency anemia.
Oral or intravenous iron can help restore iron stores and stimulate red blood cell production, gradually increasing hematocrit levels. Monitoring iron levels and adjusting the dosage are crucial to avoid adverse effects.
Erythropoiesis-Stimulating Agents (ESAs)
ESAs stimulate the bone marrow to produce more red blood cells.
These are often used in patients with kidney disease or those undergoing chemotherapy. Monitoring hemoglobin levels and adjusting the ESA dose are essential to avoid overcorrection, which can lead to adverse cardiovascular events.
Ongoing Developments
Research continues to focus on optimizing strategies for managing decreased hematocrit and its effects on blood flow.
Current studies are exploring novel therapies to improve red blood cell production and enhance oxygen delivery to tissues. Further research is also investigating the long-term impact of altered hematocrit on cardiovascular health and endothelial function.
Next Steps: Healthcare professionals are urged to closely monitor hematocrit levels in at-risk patients. Early intervention is crucial to mitigate the adverse effects of decreased hematocrit on blood flow and oxygen delivery.



+7.+What+effect+does+dehydration+have+on+an+individual+s+hematocrit.jpg)