What Glp1 Is Covered By Insurance For Weight Loss
Weight loss medications, specifically GLP-1 receptor agonists, are generating intense interest. But the crucial question remains: which ones are covered by insurance for weight management?
Navigating insurance coverage for these drugs can be complex. This article breaks down current coverage landscapes for prominent GLP-1 medications like Ozempic, Wegovy, Mounjaro, and Zepbound, helping you understand your options and access potentially life-changing treatments.
Understanding GLP-1 Medications
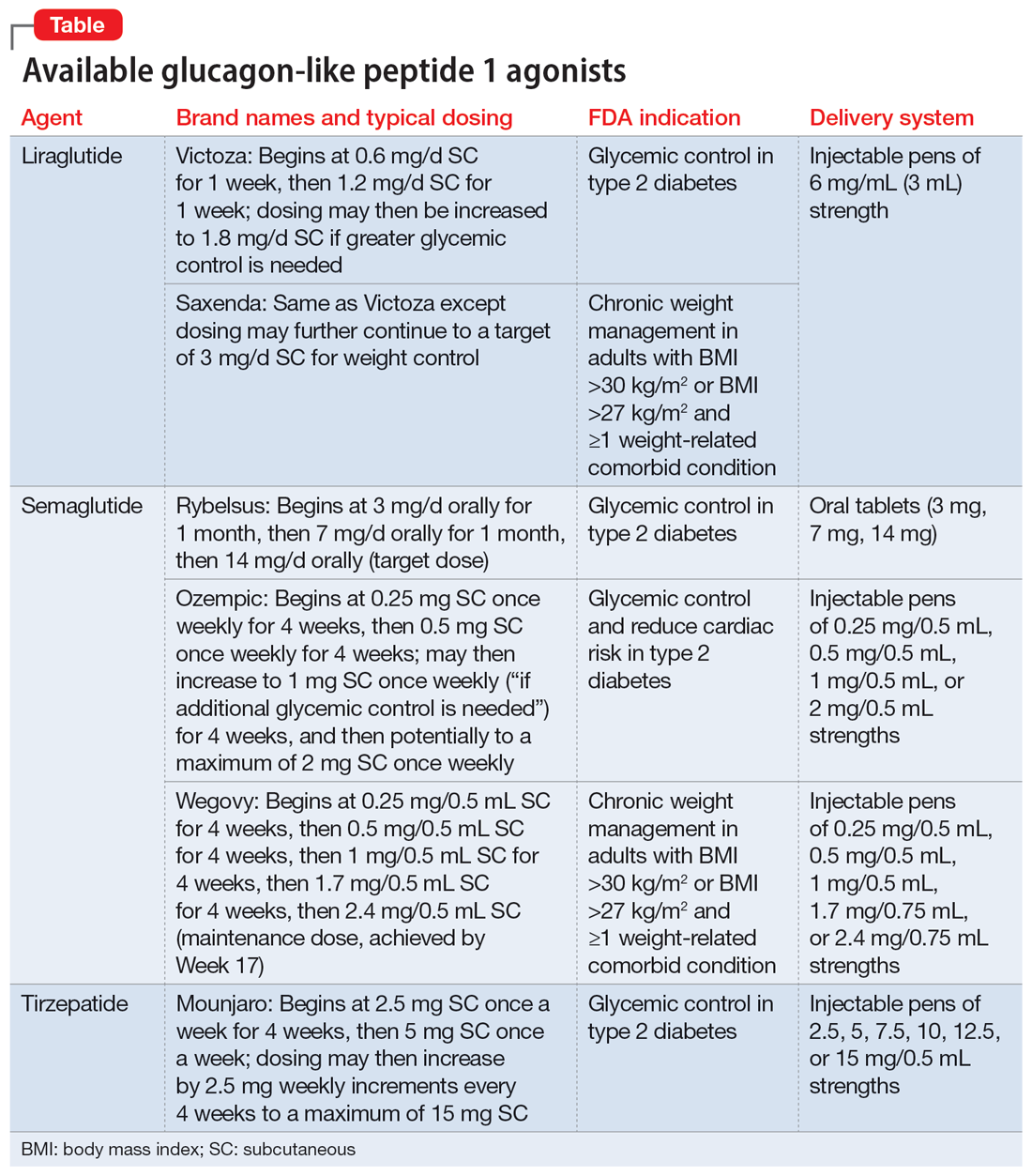
GLP-1 receptor agonists are a class of drugs initially developed for type 2 diabetes. They mimic the effects of the GLP-1 hormone, regulating blood sugar, slowing gastric emptying, and reducing appetite.
This has led to significant weight loss in many patients, prompting their use, and demand, for obesity management.
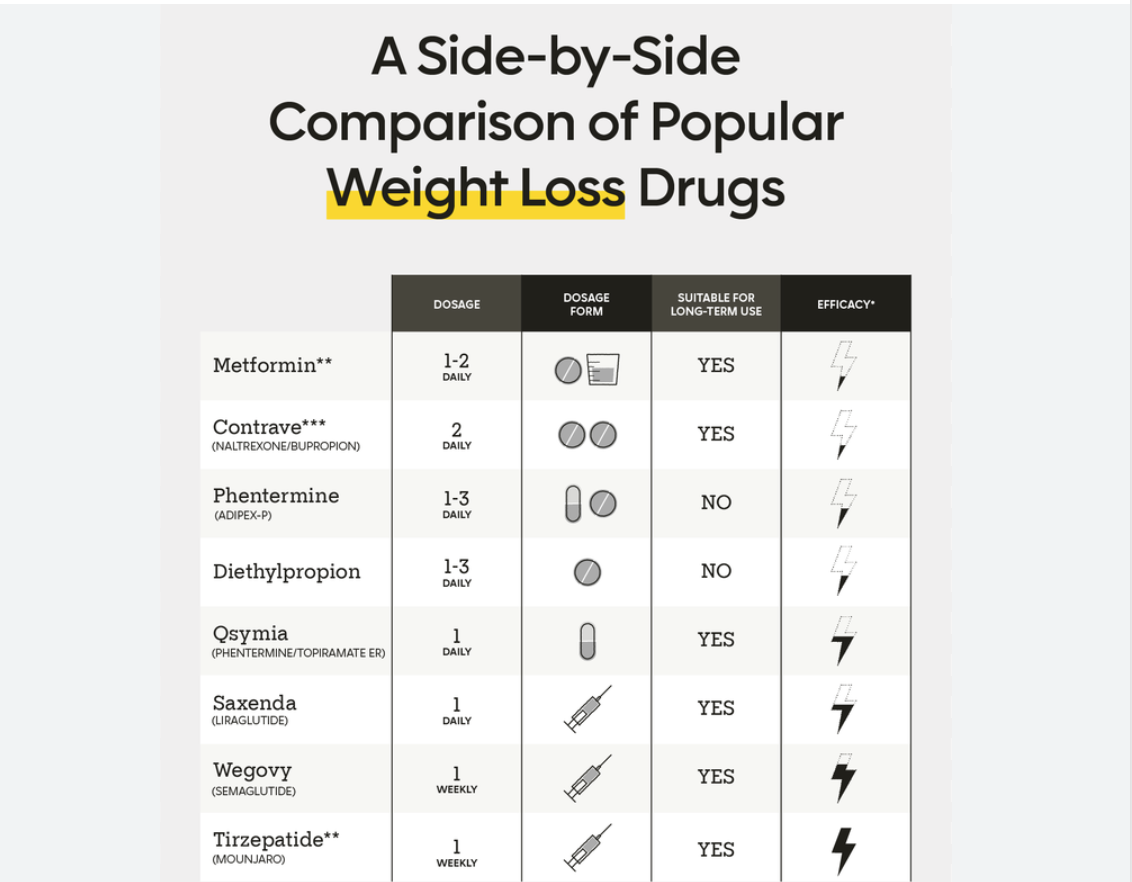
Key Medications and Their FDA Approvals
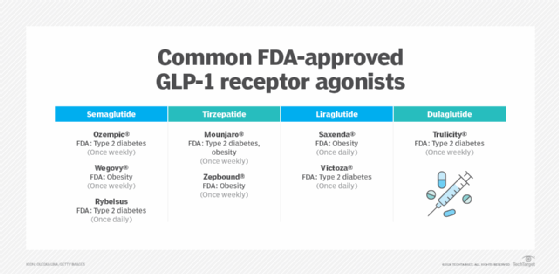
Ozempic (semaglutide) is FDA-approved for treating type 2 diabetes. However, it's frequently prescribed off-label for weight loss, though insurance coverage is less consistent in this scenario.
Wegovy (semaglutide), also from Novo Nordisk, is specifically FDA-approved for chronic weight management in adults and adolescents with obesity or overweight with at least one weight-related condition.
Mounjaro (tirzepatide) is approved for type 2 diabetes and shows promising weight loss results in clinical trials. It works on both GLP-1 and GIP receptors.
Zepbound (tirzepatide) is FDA-approved for weight loss and contains the same active ingredient as Mounjaro, but is specifically marketed for obesity treatment.
Insurance Coverage Landscape
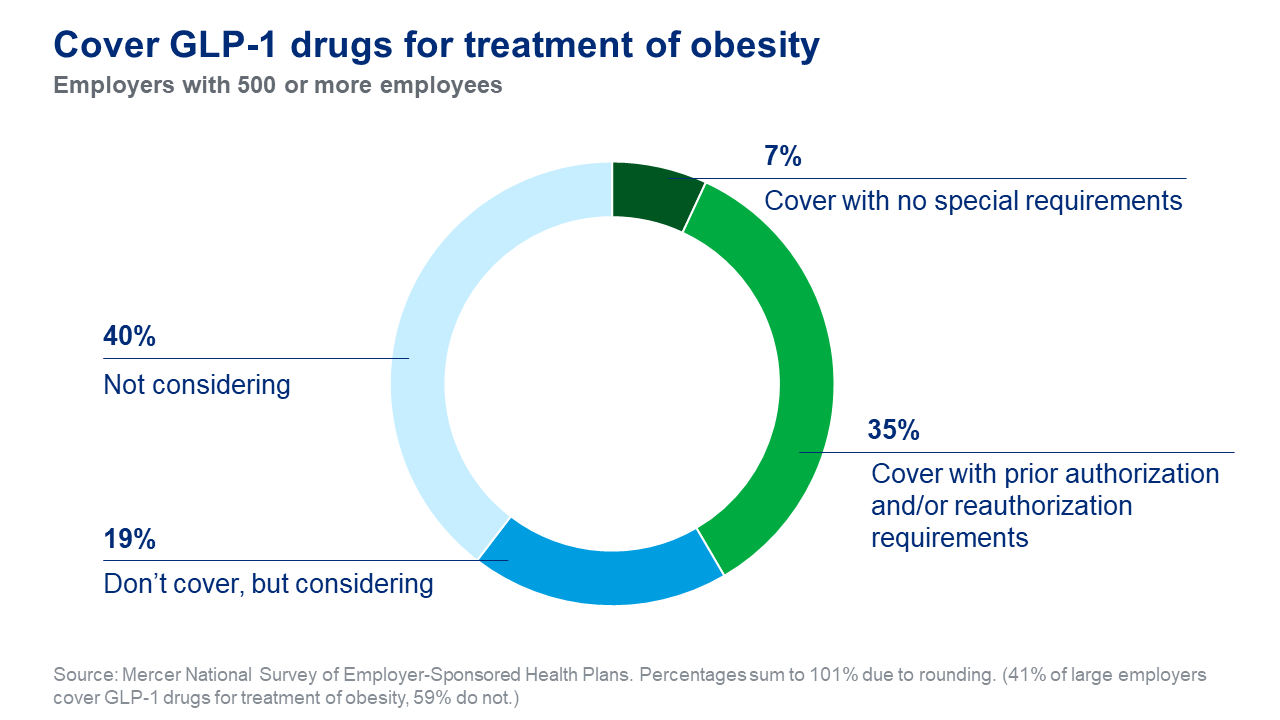
Coverage for GLP-1 medications varies widely depending on the insurance provider, plan type, and individual health circumstances.
Many insurers require prior authorization, meaning your doctor must demonstrate medical necessity. This often includes a diagnosis of type 2 diabetes or a BMI meeting specific criteria (e.g., BMI of 30 or higher, or BMI of 27 or higher with a weight-related condition).
Some employers and insurance companies have excluded weight loss medications from their formularies altogether.
Medicare Coverage
Historically, Medicare has not covered weight loss drugs. However, there are ongoing efforts to change this policy, potentially expanding access to GLP-1 medications for beneficiaries.
Currently, Medicare Part D may cover Ozempic and Mounjaro if prescribed for diabetes, but not for weight loss alone.
Medicaid Coverage
Medicaid coverage varies by state. Some states offer coverage for weight loss medications, while others do not.
Eligibility criteria and prior authorization requirements also differ significantly between state Medicaid programs.
Commercial Insurance Coverage
Commercial insurance plans offer the most diverse range of coverage options. Some plans cover Wegovy and Zepbound for weight loss, particularly if prior authorization criteria are met.
Others may only cover Ozempic or Mounjaro if prescribed for diabetes.
It is critical to contact your insurance provider directly to confirm coverage details and specific requirements.
Factors Influencing Coverage Decisions
Insurers consider several factors when determining coverage for GLP-1 medications. These include the drug's FDA approval status, the patient's diagnosis, and the presence of co-existing medical conditions.
Step therapy is often required. This means patients must first try and fail on other, less expensive weight loss treatments before being approved for a GLP-1 medication.
The increasing demand and high cost of these drugs are also influencing coverage decisions.
Appealing Denials
If your insurance claim for a GLP-1 medication is denied, you have the right to appeal. Work closely with your doctor to gather supporting documentation demonstrating the medical necessity of the medication.
This may include lab results, medical history, and documentation of previous weight loss attempts.
Persistence is key, as successful appeals are possible.
Cost Considerations
Even with insurance coverage, GLP-1 medications can be expensive. Co-pays and deductibles can add up, making them unaffordable for some patients.
Manufacturer discount programs and patient assistance programs may be available to help lower the cost.
Consider exploring all available options to determine the most affordable pathway.
Next Steps and Ongoing Developments
Consult with your healthcare provider to discuss whether a GLP-1 medication is right for you. Contact your insurance company to verify coverage details and requirements.
Monitor ongoing policy changes, as coverage for these medications is evolving rapidly.
Advocacy efforts are underway to expand access to these potentially life-saving treatments for all who need them.