What Information Should Be Documented On The Daily Restorative Documentation

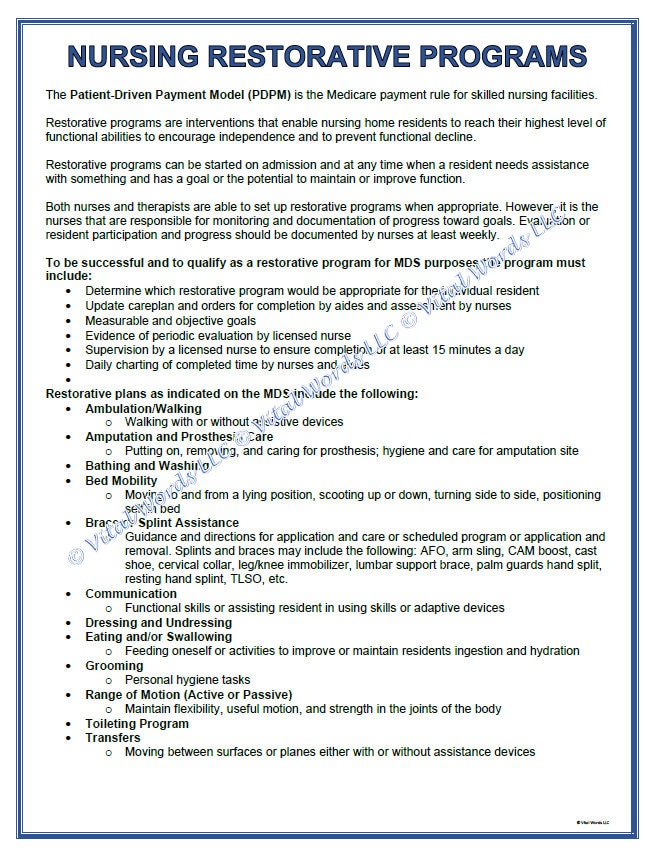
Accurate and comprehensive documentation is the cornerstone of effective restorative care in healthcare settings. The daily restorative documentation serves as a critical communication tool among healthcare professionals. It ensures continuity of care and tracks patient progress.
The Importance of Daily Restorative Documentation
Restorative care focuses on helping individuals regain or maintain their highest practicable level of physical, mental, and psychosocial well-being. Meticulous documentation allows healthcare providers to monitor the effectiveness of interventions. It adjusts treatment plans as needed.
Clear documentation also plays a vital role in regulatory compliance. It protects healthcare facilities from potential legal challenges. It also contributes to improved patient outcomes and enhanced quality of life.
Key Information to Document
Several essential data points should be included in daily restorative documentation. These details paint a comprehensive picture of the patient's current condition and progress.
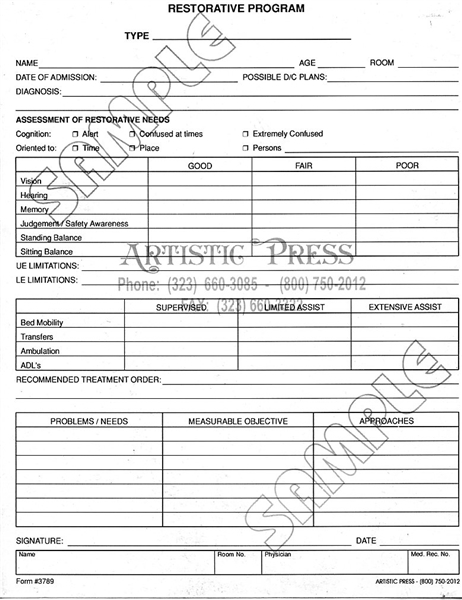
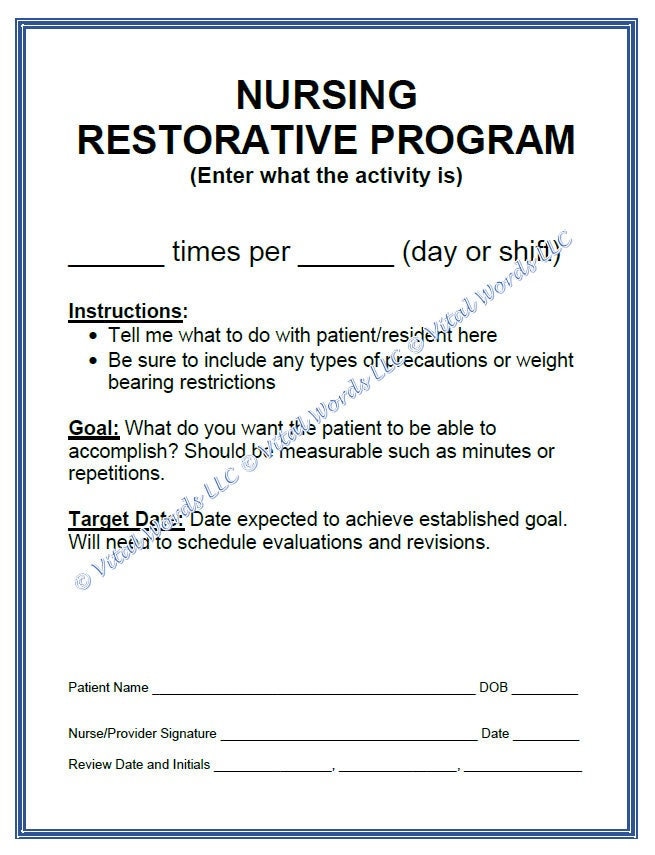
Patient Demographics and Identification
The patient's full name, date of birth, and medical record number are crucial for proper identification. This prevents errors and ensures that the documentation pertains to the correct individual.
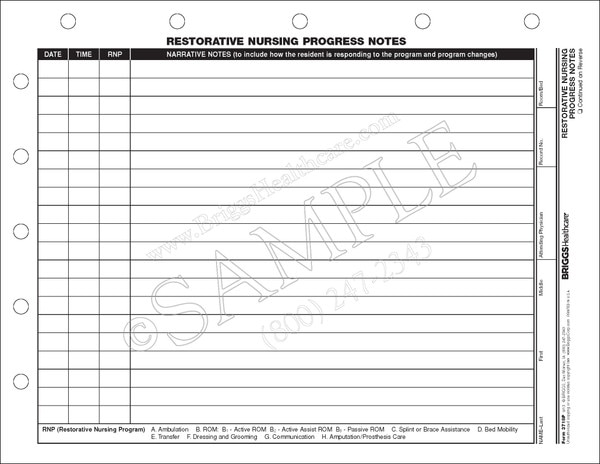
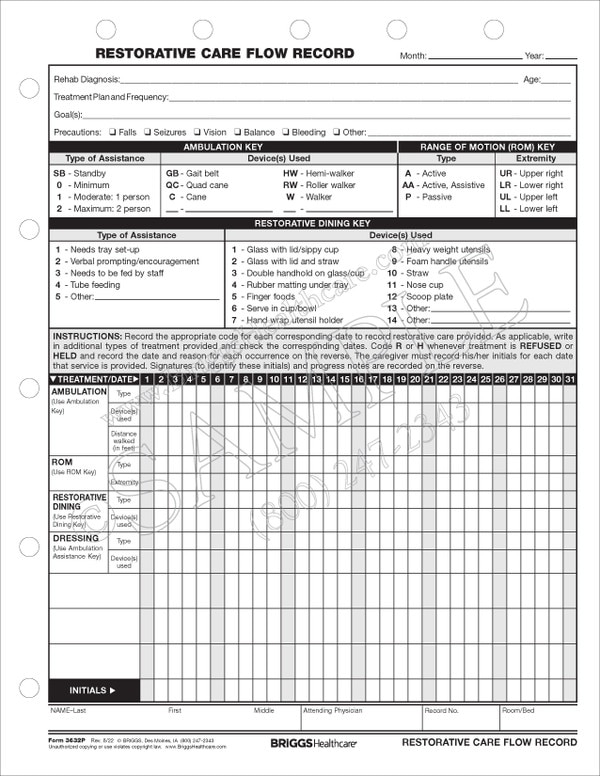
Date and Time of Intervention
Accurate recording of the date and time each restorative intervention occurred is necessary. This establishes a clear timeline of care provided.
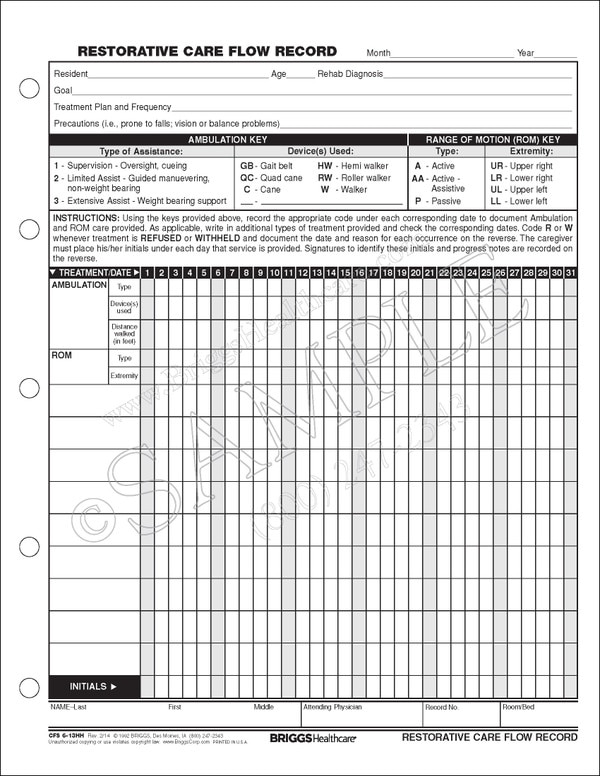
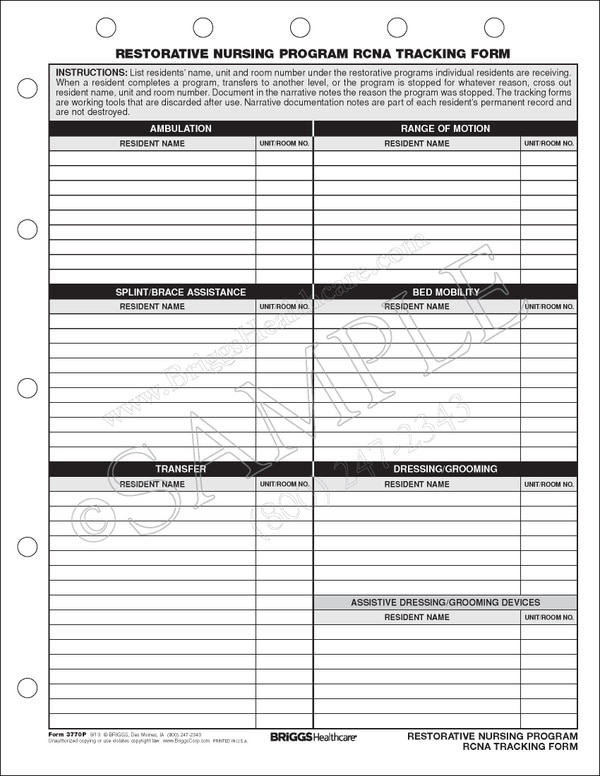
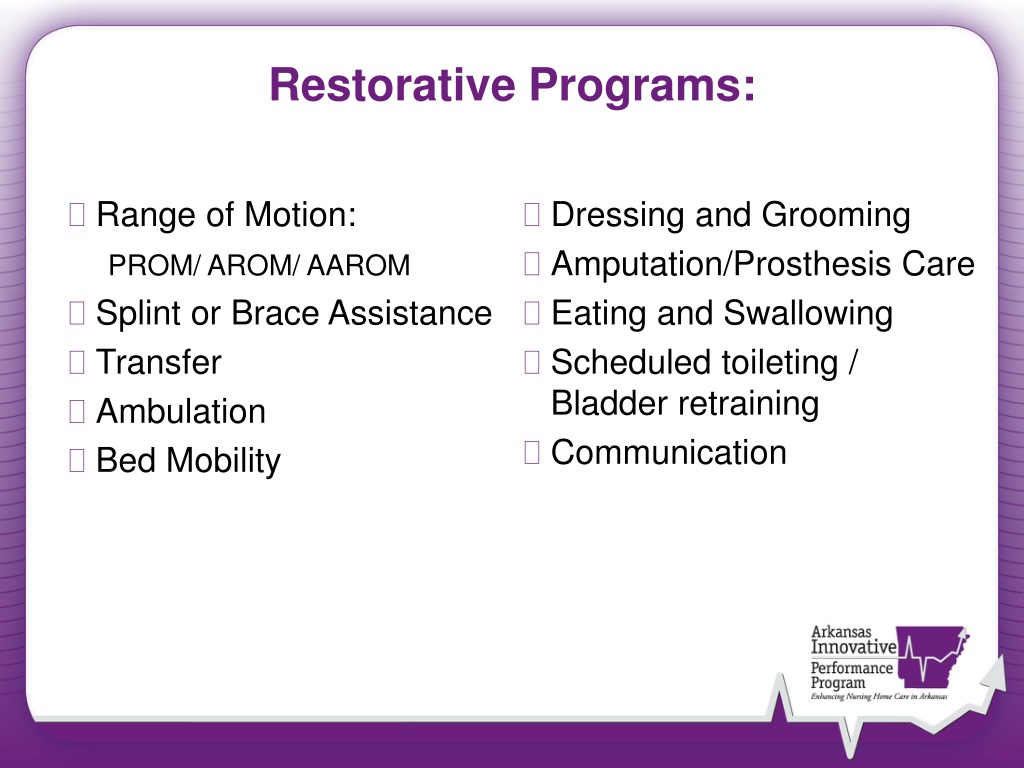
Specific Restorative Interventions Performed
Detailed descriptions of all restorative interventions performed must be documented. This includes exercises, ambulation assistance, activities of daily living (ADL) support, and any other specific therapies or techniques used. The level of assistance required by the patient should also be noted. For example, independent, stand-by assistance, minimal assistance, moderate assistance, or total assistance.
The type of equipment used during the intervention, such as walkers, wheelchairs, or assistive devices, should be recorded.
Patient's Response to Intervention
Objectively documenting the patient's response to each intervention is critical. Note any improvements, declines, or lack of change in their physical or cognitive abilities. Any pain experienced during the intervention should be documented. The pain's location, intensity (using a pain scale), and alleviating factors are important.
Document any changes in the patient’s mood or affect during or after the intervention.
Objective Measurements and Data
Include measurable data such as vital signs (heart rate, blood pressure, oxygen saturation). Also note range of motion measurements, weight-bearing status, and distance ambulated. Standardized assessment tools, like the Functional Independence Measure (FIM), should be used and documented according to protocol.
Observations of Skin Integrity
Regularly assess and document the patient's skin integrity. Note the presence of any pressure ulcers, skin tears, or other skin conditions. Documenting the location, size, and stage of any skin breakdown is crucial for monitoring healing and preventing complications.
Communication with Other Healthcare Professionals
Record any communication with other members of the healthcare team regarding the patient's care. This includes physician orders, consultations with therapists, and discussions with nurses or nursing assistants.
Barriers to Participation
Document any factors that may have hindered the patient's participation in restorative interventions. This includes physical limitations, cognitive impairments, pain, fatigue, or emotional distress.
Goals and Progress Toward Goals
Clearly state the established goals for the patient's restorative care. Document the patient's progress toward achieving those goals. Adjustments to the treatment plan should be noted, along with the rationale for the changes.
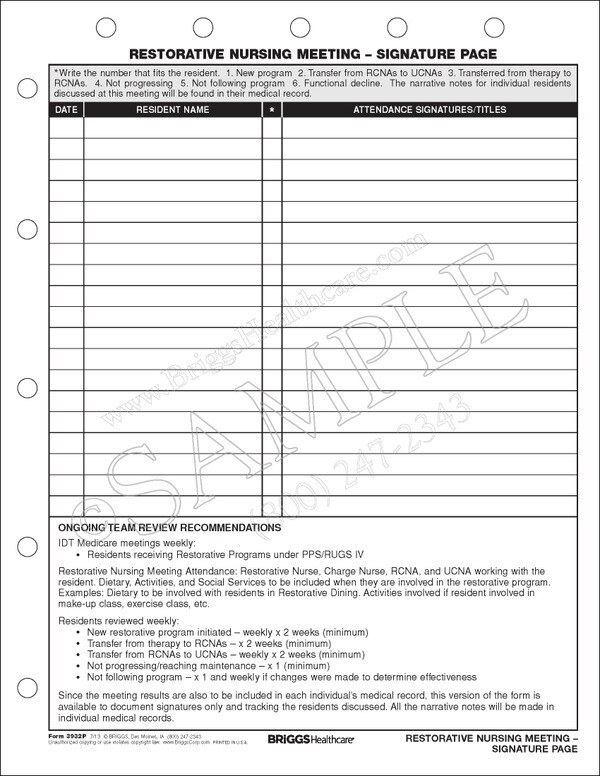
Signature and Credentials of the Documenting Professional
The documenting healthcare professional must sign and include their credentials on each entry. This ensures accountability and allows for easy identification of the individual responsible for the documentation.
The Role of Technology in Documentation
Electronic health records (EHRs) are increasingly used in healthcare settings. They streamline the documentation process. EHRs can improve accuracy, enhance communication, and facilitate data analysis.
However, proper training and adherence to established documentation protocols are still essential. EHRs also help facilities adhere to HIPAA regulations.
Potential Impact and Benefits
Comprehensive daily restorative documentation has significant benefits. It promotes better patient care. It improves communication among healthcare providers. It ensures regulatory compliance.
Accurate documentation allows for data-driven decision-making. It helps healthcare professionals identify trends, evaluate the effectiveness of interventions, and optimize treatment plans. This ultimately leads to improved patient outcomes and a higher quality of life.
When restorative documentation is consistent, it can also lead to better facility ratings. This can help attract new patients and better manage facility resources.