What Is The First Line Treatment For Ventricular Tachycardia

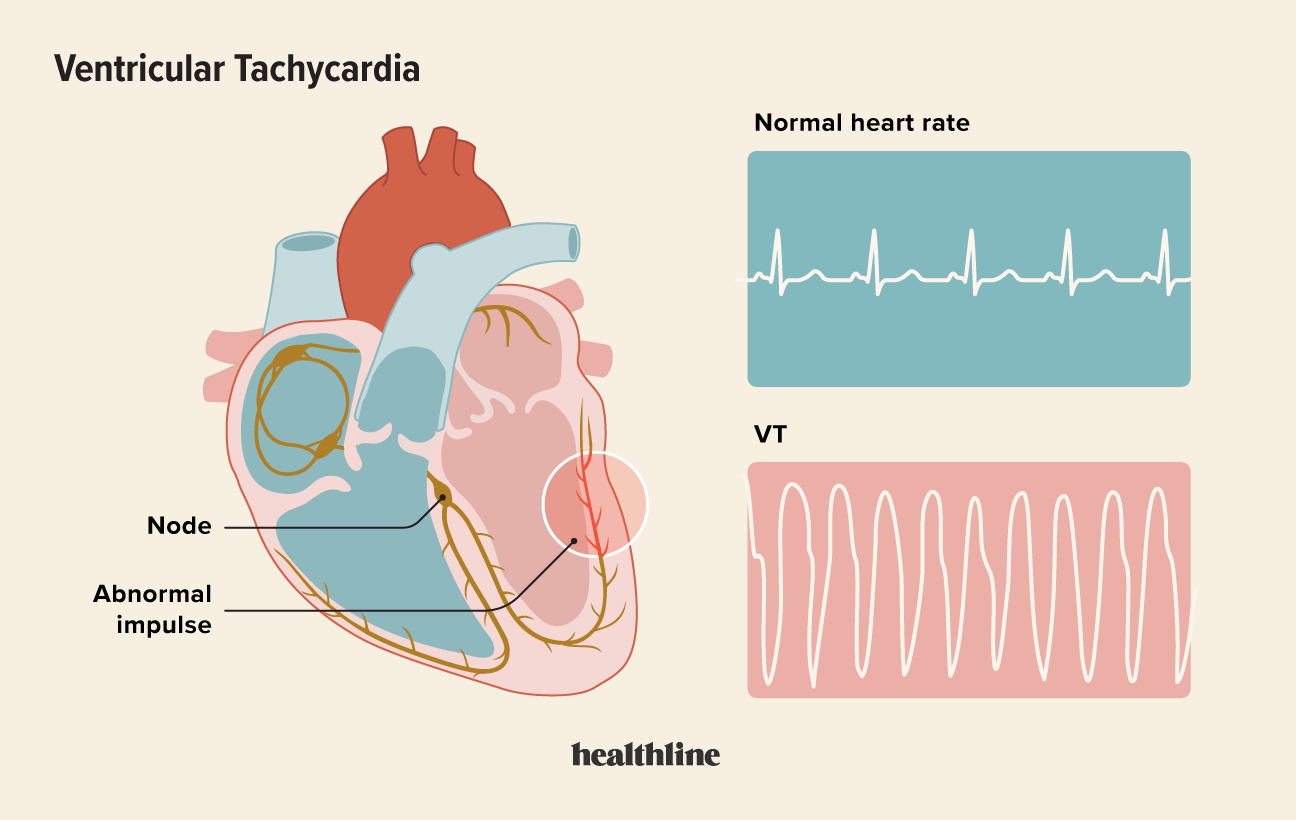
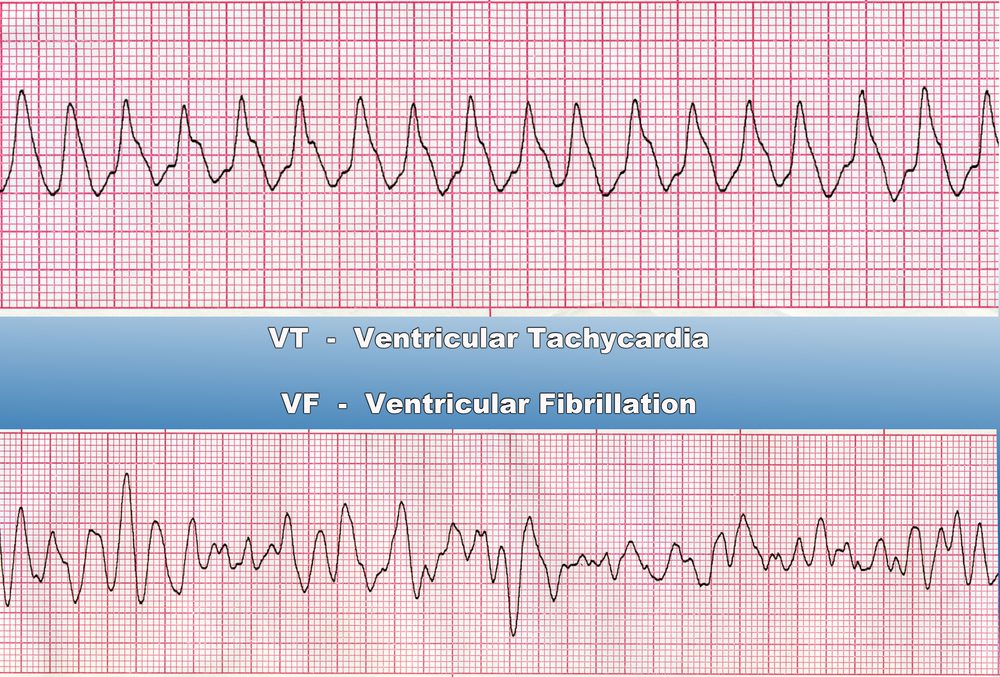
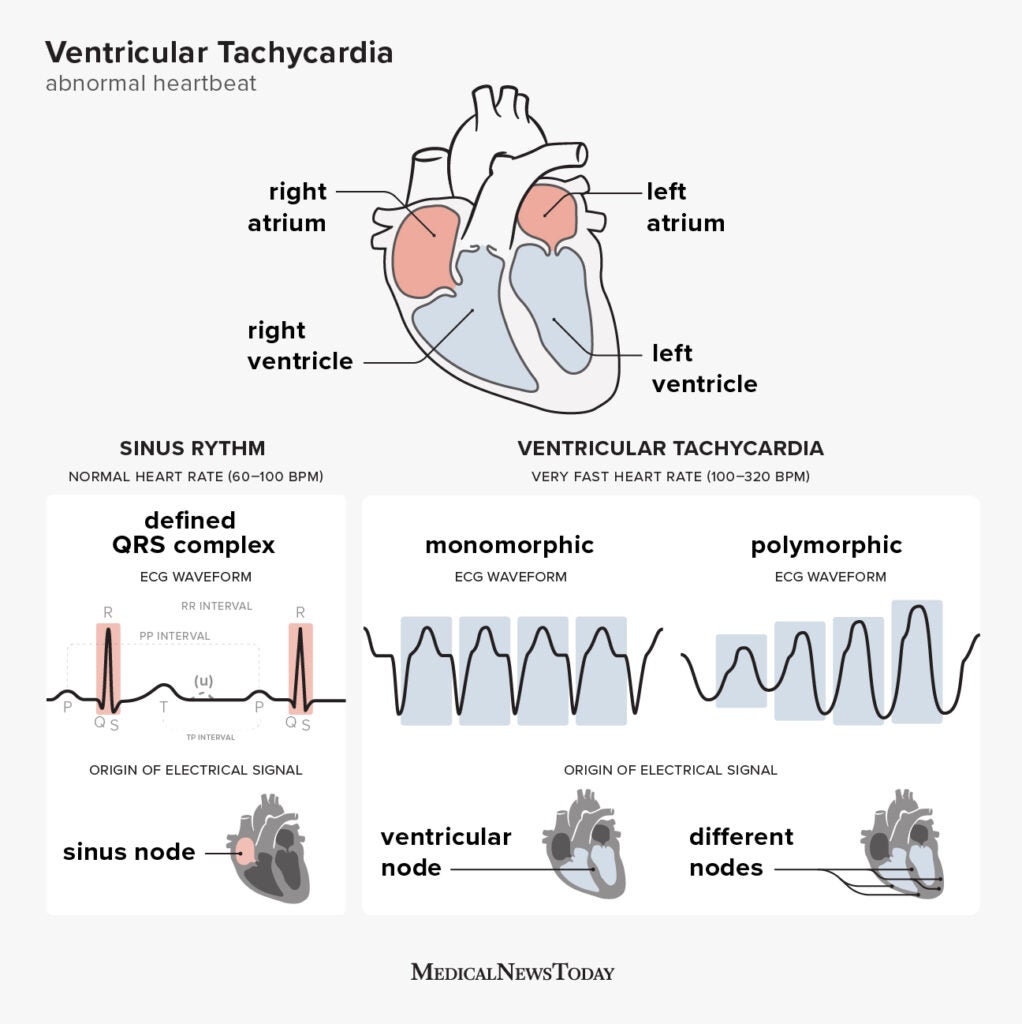
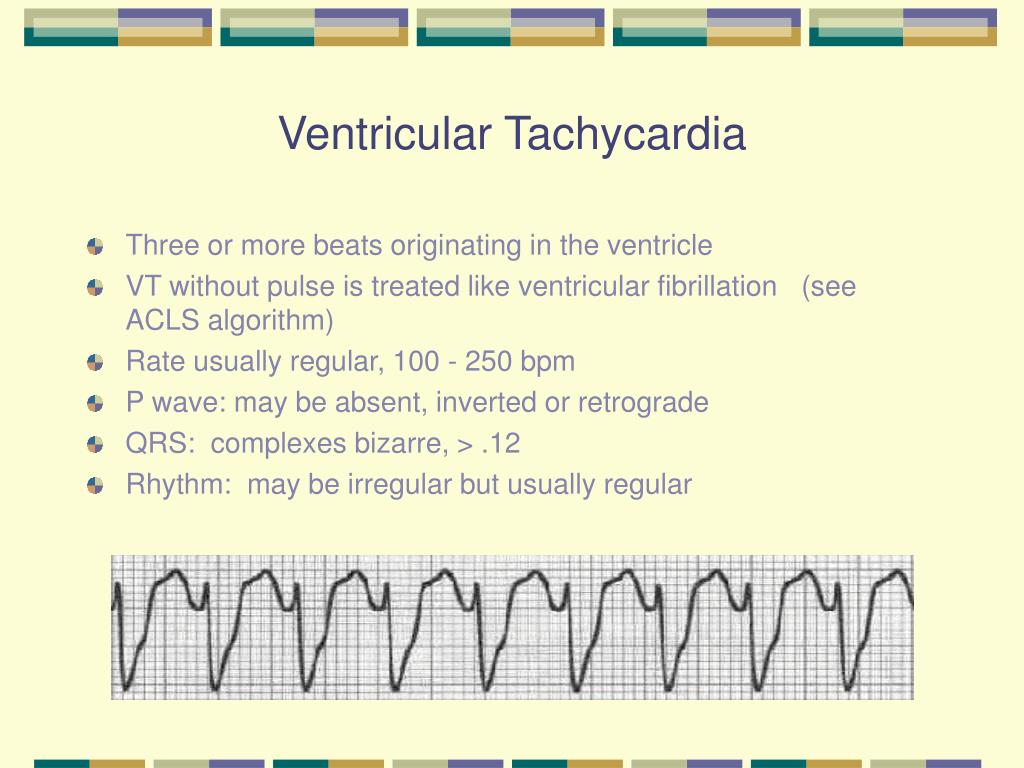
Ventricular tachycardia (VT), a rapid and potentially life-threatening heart rhythm originating in the ventricles, demands swift and decisive action. Left untreated, VT can quickly degenerate into ventricular fibrillation, leading to sudden cardiac arrest and death. Understanding the immediate steps to manage this perilous condition is critical for healthcare professionals and can significantly impact patient outcomes.
This article delves into the first-line treatments for ventricular tachycardia, focusing on the initial strategies employed to restore a stable heart rhythm and prevent further complications. We will explore the use of medications, specifically antiarrhythmics, and the role of electrical cardioversion in acutely managing VT. Furthermore, we will discuss the factors that influence treatment decisions and the importance of identifying the underlying cause of the arrhythmia to guide long-term management strategies.
Initial Assessment and Stabilization
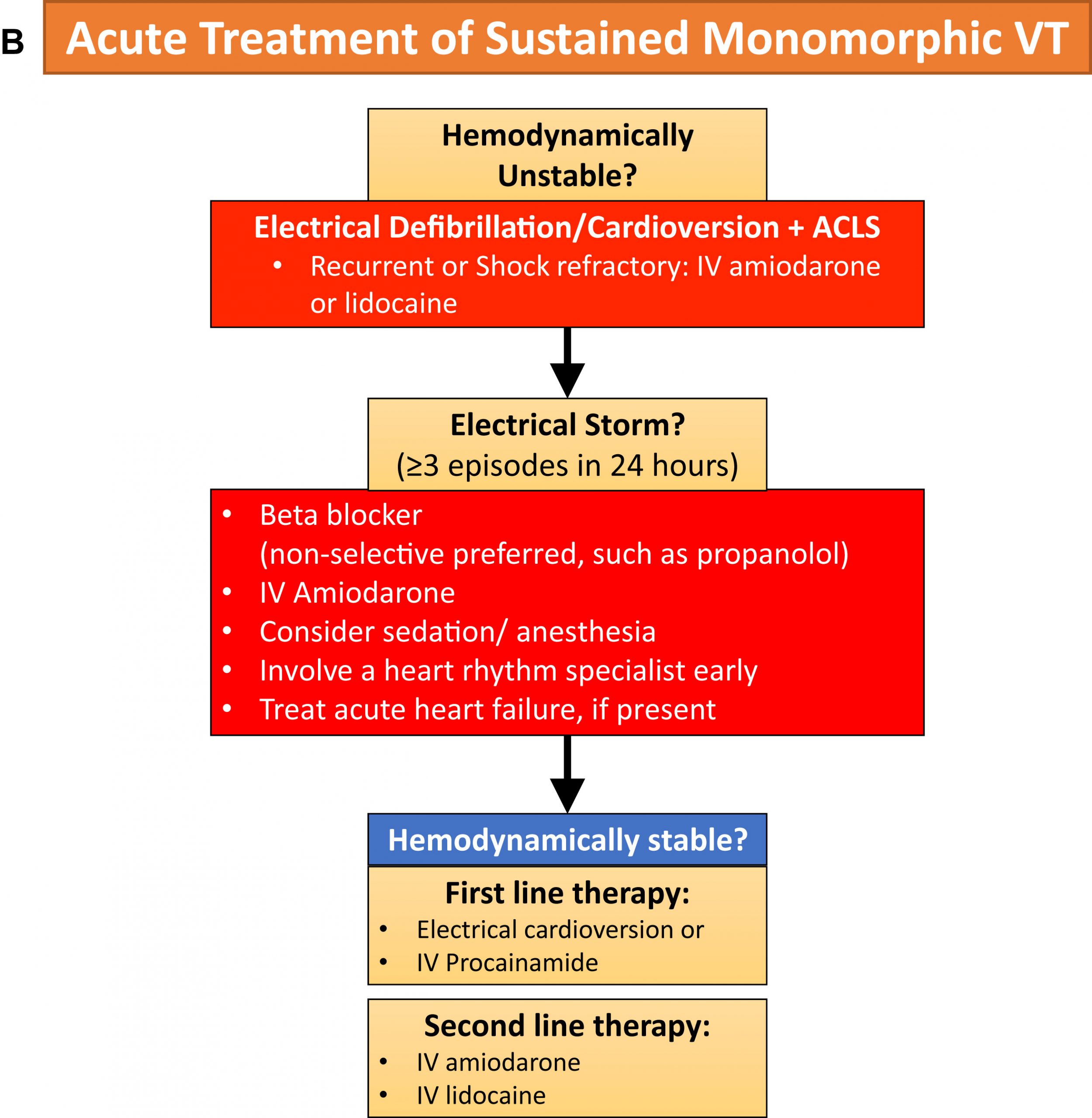
The first step in managing ventricular tachycardia is a rapid assessment of the patient's hemodynamic stability. Is the patient conscious? Is there a palpable pulse? These initial observations dictate the urgency and approach to treatment.
If the patient is unstable – hypotensive, experiencing chest pain, shortness of breath, or altered mental status – immediate intervention is required. This typically involves synchronized cardioversion, an electrical shock delivered to the heart to reset the rhythm.
Synchronized Cardioversion: The Primary Intervention
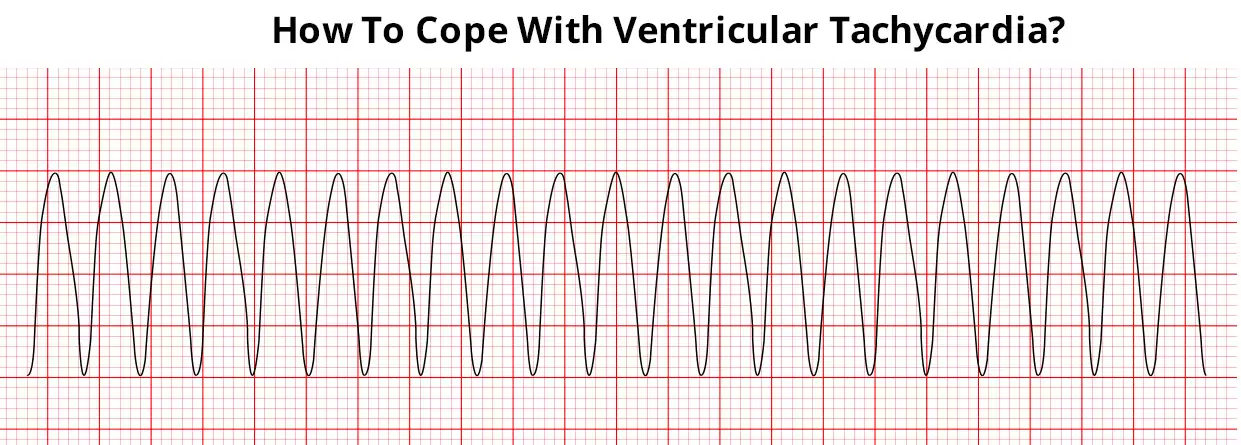
Synchronized cardioversion is the delivery of an electrical shock timed to coincide with the R wave of the QRS complex on the electrocardiogram (ECG). This timing is crucial to avoid delivering the shock during the heart's vulnerable period (T wave), which could potentially induce ventricular fibrillation.
The initial energy level for cardioversion depends on the type of defibrillator being used (monophasic or biphasic) and the specific clinical scenario. Typically, healthcare providers start with lower energy levels and escalate as needed until a stable rhythm is achieved.
According to the American Heart Association (AHA) guidelines, for monophasic defibrillators, the initial energy dose is typically 100 joules, whereas biphasic defibrillators may start at a lower energy level, such as 50-100 joules.
Pharmacological Interventions
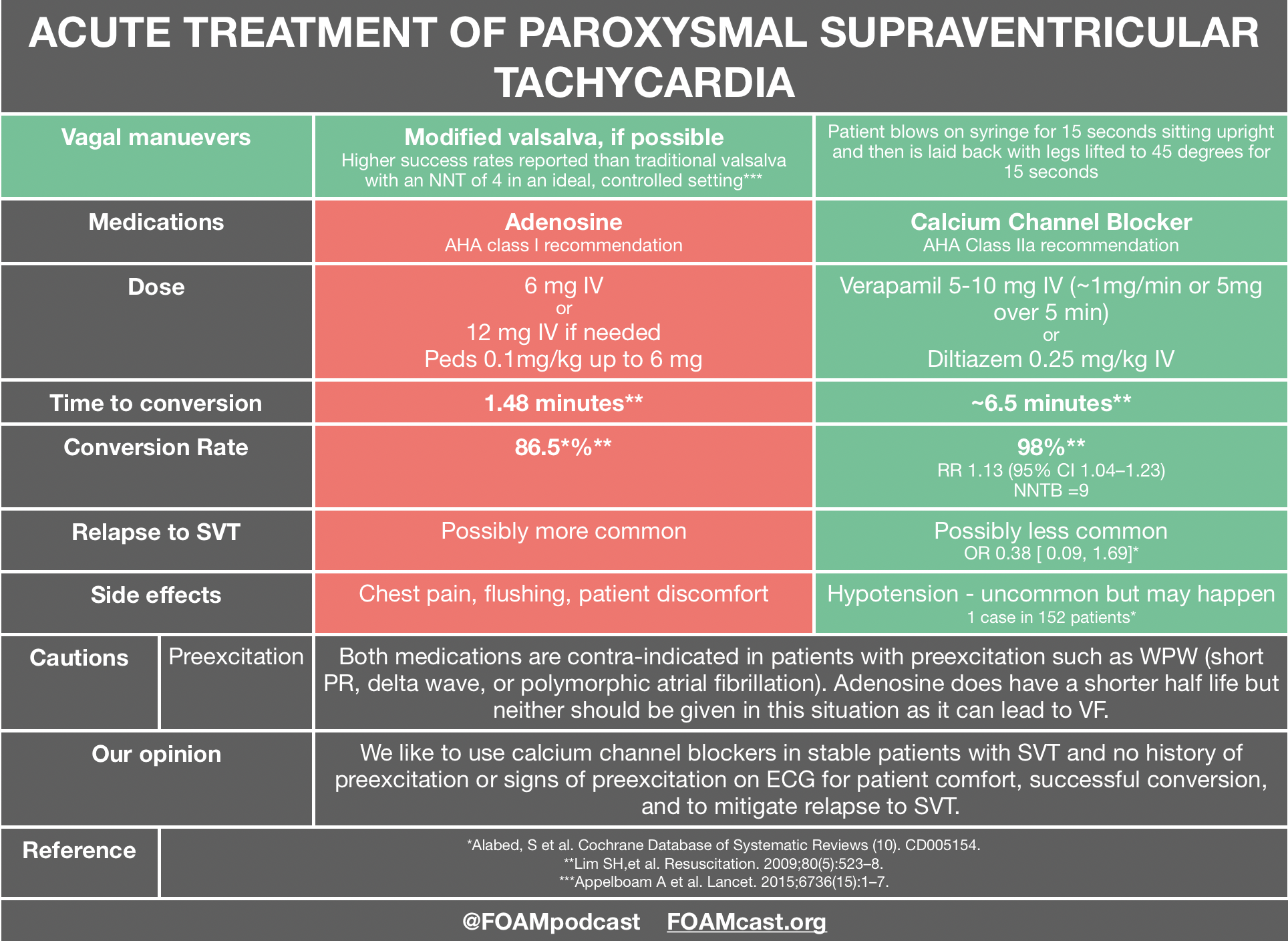
While synchronized cardioversion is the primary treatment for unstable VT, pharmacological interventions play a vital role in both acute management and long-term prevention. Antiarrhythmic medications are used to suppress the abnormal electrical activity in the heart and restore a normal sinus rhythm.
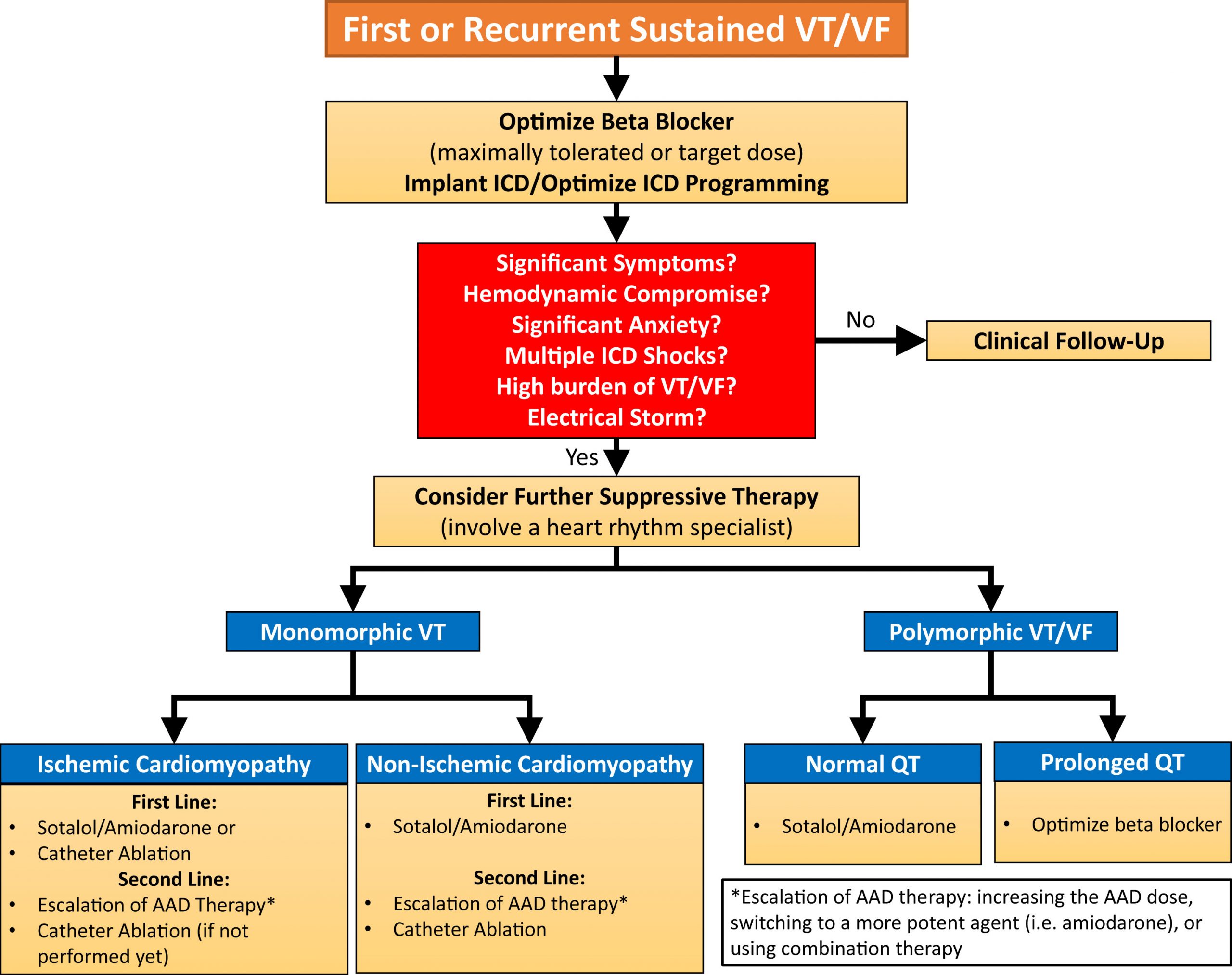
The choice of antiarrhythmic drug depends on several factors, including the type of VT (monomorphic vs. polymorphic), the patient's underlying cardiac condition, and the presence of any contraindications. Common first-line antiarrhythmics include amiodarone and lidocaine.
Amiodarone: A Broad-Spectrum Antiarrhythmic
Amiodarone is a broad-spectrum antiarrhythmic agent effective in treating a wide range of ventricular arrhythmias, including VT. It works by affecting multiple ion channels in the heart, prolonging the refractory period and slowing down the heart rate.
Amiodarone can be administered intravenously (IV) in the acute setting to terminate VT. It is often the preferred drug for patients with structural heart disease, as it is generally better tolerated than other antiarrhythmics in this population.
However, amiodarone has a long half-life and can cause a variety of side effects, including thyroid abnormalities, pulmonary toxicity, and liver dysfunction. Therefore, it should be used with caution and close monitoring.
Lidocaine: An Alternative Option
Lidocaine is another antiarrhythmic drug that can be used to treat VT, particularly in the setting of acute myocardial infarction. It works by blocking sodium channels in the heart, slowing down conduction velocity and suppressing ectopic activity.
Lidocaine is typically administered intravenously as a bolus followed by a continuous infusion. It is generally well-tolerated but can cause neurological side effects such as confusion, tremors, and seizures at higher doses.
Lidocaine may be less effective than amiodarone in terminating VT, especially in patients with structural heart disease. The European Resuscitation Council (ERC) guidelines acknowledges that lidocaine can be considered if amiodarone is unavailable or contraindicated.
Stable Ventricular Tachycardia
If the patient is hemodynamically stable, a more deliberate approach can be taken. This involves obtaining a 12-lead ECG to determine the morphology of the VT and assess the patient's overall cardiac function.
In stable VT, antiarrhythmic medications are typically the first-line treatment. Amiodarone is often the preferred choice, but other options, such as procainamide, may also be considered.
Cardioversion may still be necessary if the medication is ineffective or if the patient's condition deteriorates. Consulting with a cardiologist or electrophysiologist is crucial to determine the most appropriate management strategy.
Underlying Causes and Long-Term Management
Identifying and addressing the underlying cause of VT is essential for preventing recurrence. Common causes include coronary artery disease, heart failure, cardiomyopathy, and electrolyte imbalances.
Long-term management strategies may include medications to control heart rate and rhythm, lifestyle modifications, and implantable cardioverter-defibrillators (ICDs). An ICD is a device implanted in the chest that can detect and treat life-threatening arrhythmias, including VT and ventricular fibrillation.
According to studies published in the New England Journal of Medicine, ICDs have been shown to significantly reduce the risk of sudden cardiac death in patients with a history of VT or those at high risk for developing it.
Conclusion
The initial management of ventricular tachycardia requires a rapid and systematic approach, prioritizing the patient's hemodynamic stability. Synchronized cardioversion remains the cornerstone of treatment for unstable VT, while antiarrhythmic medications play a crucial role in both acute management and long-term prevention.
Understanding the various treatment options and the factors that influence their selection is paramount for healthcare professionals managing this potentially life-threatening arrhythmia. A thorough assessment of the underlying cause and appropriate long-term management strategies are essential to prevent recurrence and improve patient outcomes.
Continued research and advancements in cardiac electrophysiology are constantly refining our understanding and treatment of ventricular tachycardia, offering hope for improved outcomes in the future.