Which Concern Is Best Reported Through The High Reliability Platform
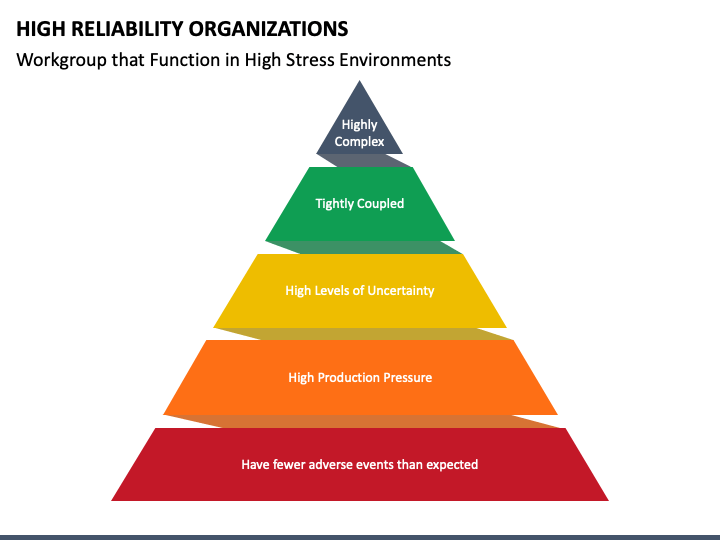
The promise of a safer, more accountable healthcare system hinges increasingly on the effective implementation of High Reliability Organizations (HROs). Yet, amidst the enthusiasm for adopting HRO principles, a critical question persists: which specific patient safety concerns are best addressed through this rigorous framework? Failure to prioritize appropriately risks diluting resources and hindering progress towards meaningful improvement.
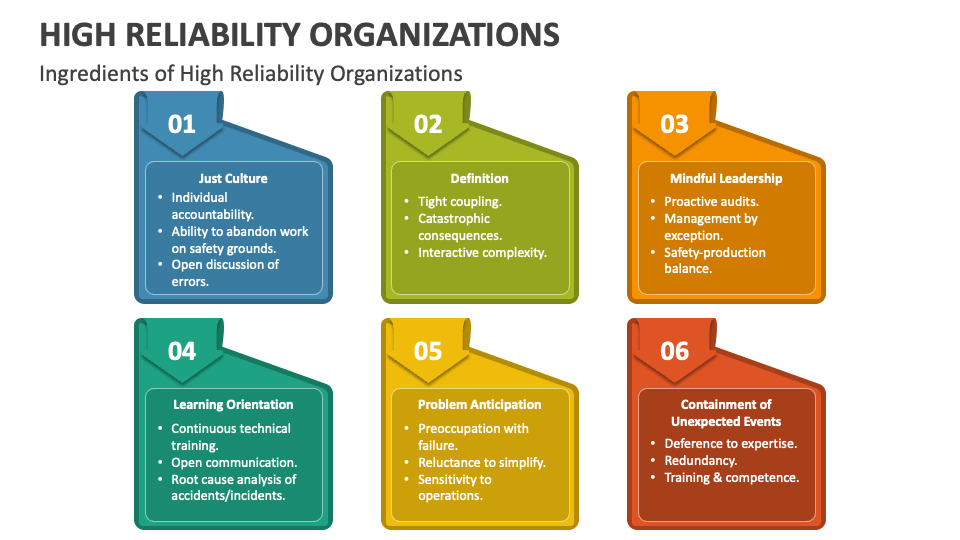
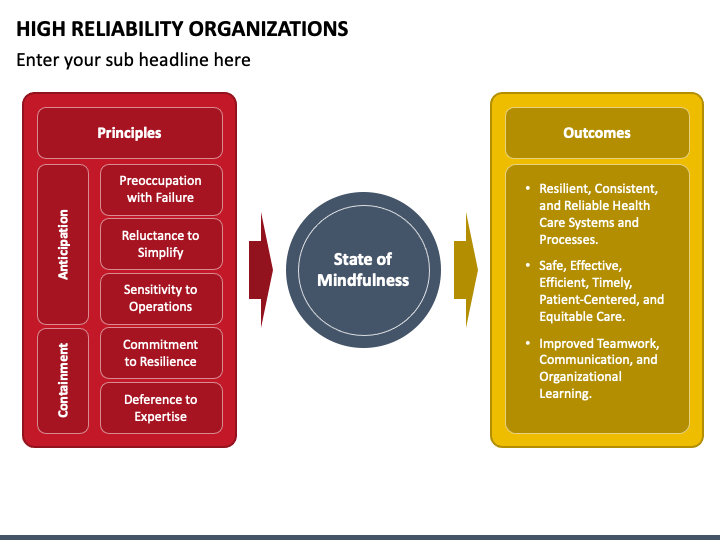
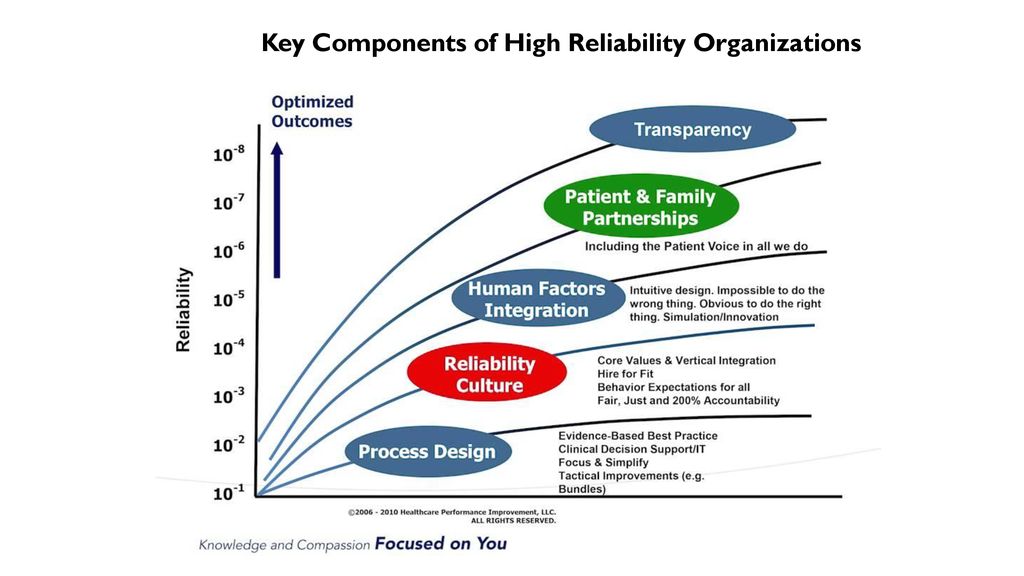
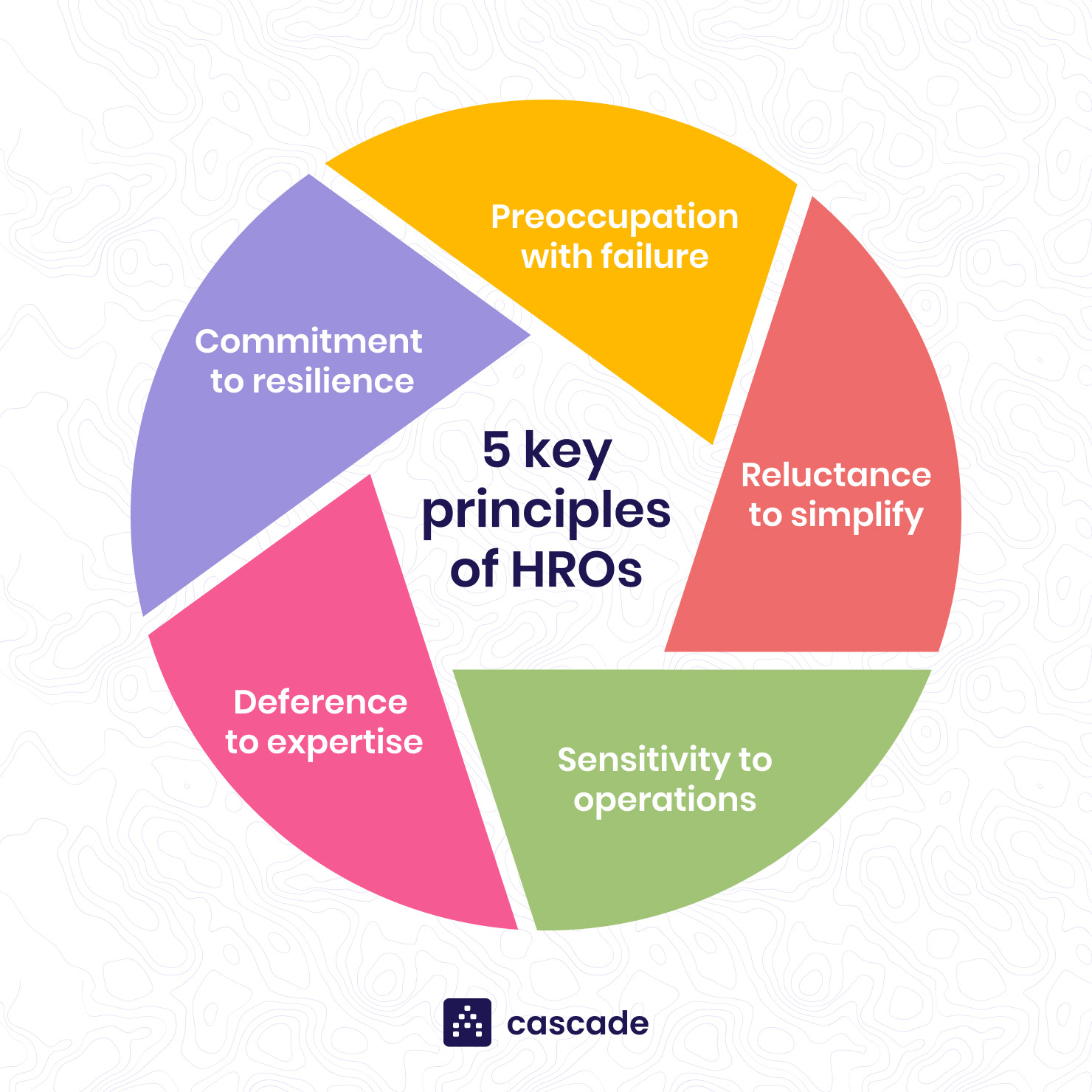
This article examines the optimal application of the High Reliability Platform, focusing on those areas where its principles – preoccupation with failure, reluctance to simplify, sensitivity to operations, commitment to resilience, and deference to expertise – yield the most significant positive impact. It delves into expert opinions, data-driven analysis, and real-world examples to identify the types of concerns for which HRO implementation offers the greatest potential for preventing harm and fostering a culture of continuous learning.
Understanding High Reliability Principles in Practice
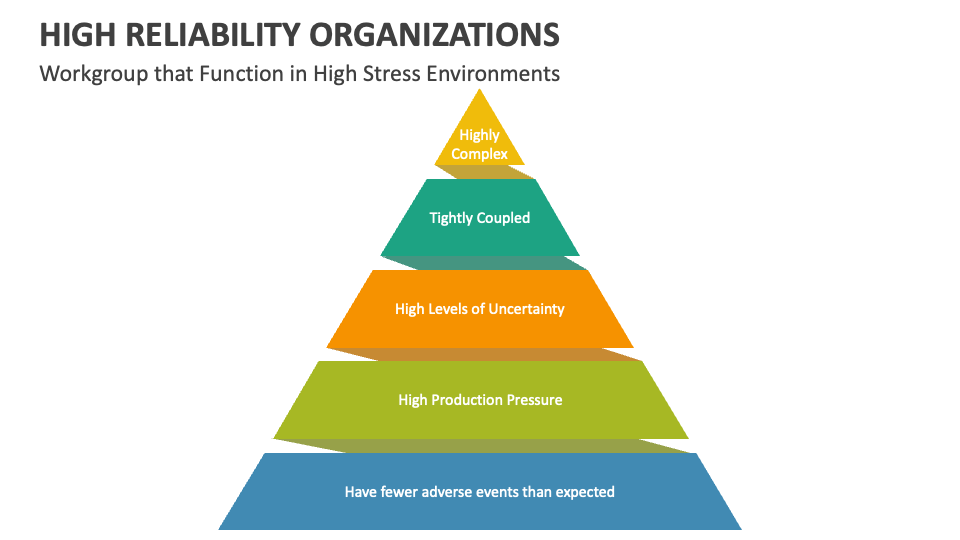
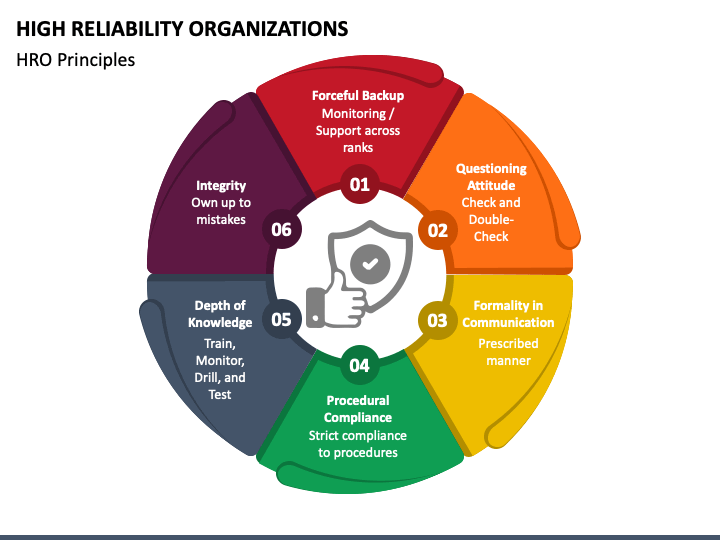
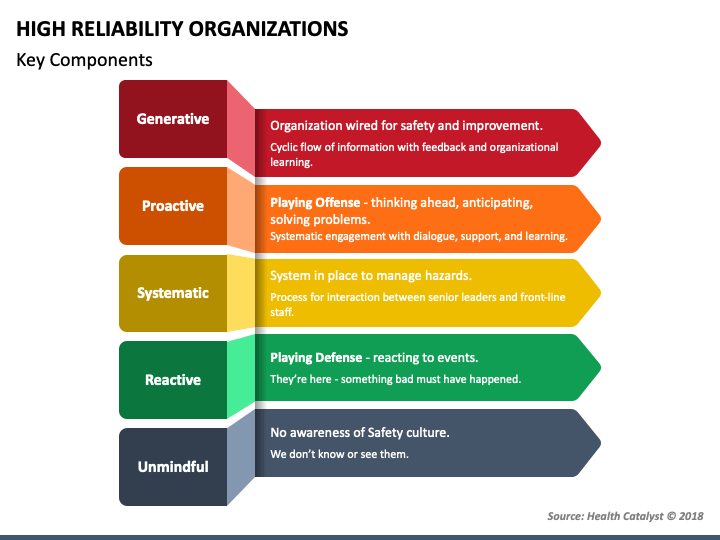
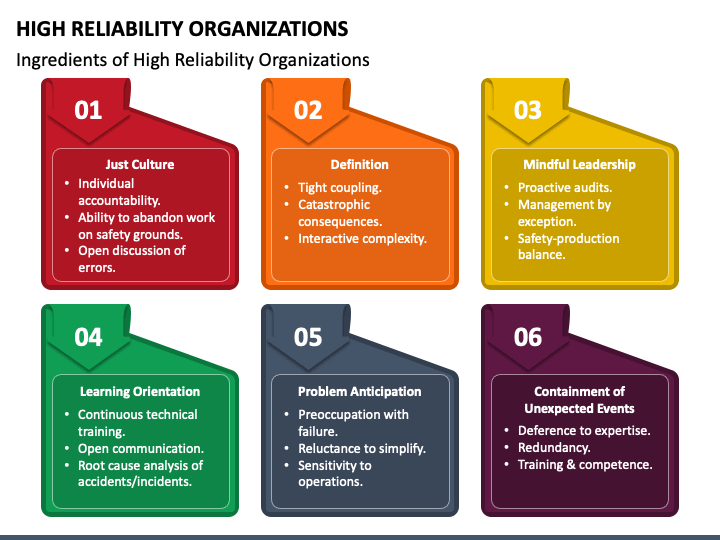
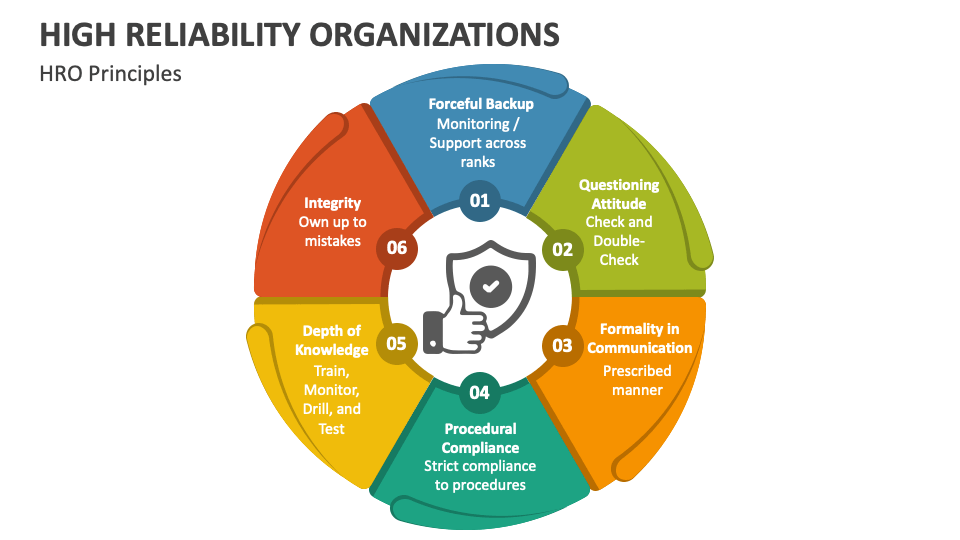
The core tenets of HRO theory are designed to create systems that are exceptionally resistant to errors, especially in complex and high-risk environments. Preoccupation with failure compels organizations to actively seek out and analyze near misses, recognizing them as opportunities for learning and improvement. This proactive approach stands in stark contrast to reactive strategies that only address problems after they occur.
Reluctance to simplify discourages the oversimplification of complex processes, encouraging a deeper understanding of the factors that contribute to errors. Sensitivity to operations emphasizes the importance of situational awareness and continuous monitoring of ongoing activities. This includes paying close attention to subtle changes in the environment that may indicate potential problems.
Commitment to resilience focuses on the ability of the organization to adapt and recover quickly from unexpected events. Deference to expertise empowers individuals with the most relevant knowledge to make decisions, regardless of their position in the organizational hierarchy.
Prioritizing Concerns: Where HROs Excel
While HRO principles can be broadly applied, certain patient safety concerns benefit disproportionately from this structured approach. These often involve complex, high-risk processes with significant potential for harm.
1. Medication Safety
Medication errors represent a pervasive threat to patient safety. HRO principles can be used to improve every stage of the medication use process, from ordering and transcribing to dispensing and administering.
A preoccupation with failure can be fostered by actively tracking and analyzing near misses related to medication errors. This could involve implementing robust systems for reporting and investigating discrepancies, even when no harm reaches the patient.
Reluctance to simplify encourages a thorough understanding of the complexities of medication interactions and patient-specific factors that may increase the risk of adverse events. This might include using decision support tools to help clinicians make informed choices about medication selection and dosing.
2. Surgical Safety
The operating room is a high-risk environment where errors can have catastrophic consequences. HRO principles can significantly enhance surgical safety by improving communication, teamwork, and adherence to established protocols.
Using checklists and standardized procedures promotes sensitivity to operations and reduces the likelihood of errors due to miscommunication or oversight. Regular drills and simulations can enhance commitment to resilience by preparing surgical teams to respond effectively to unexpected events.
Empowering nurses and other members of the surgical team to speak up when they observe potential safety concerns embodies the principle of deference to expertise. This can help prevent errors before they occur, even if the individual raising the concern is lower in the organizational hierarchy.
3. Infection Prevention
Healthcare-associated infections (HAIs) remain a significant challenge for hospitals and other healthcare facilities. HRO principles can be applied to improve infection prevention practices and reduce the incidence of HAIs.
A preoccupation with failure can be fostered by actively monitoring infection rates and investigating potential outbreaks. This involves using data-driven analysis to identify areas where infection prevention practices can be improved.
Implementing standardized hand hygiene protocols and ensuring that healthcare workers have access to appropriate personal protective equipment (PPE) promotes sensitivity to operations. Regular training and education can reinforce the importance of infection prevention and help healthcare workers adhere to established guidelines.
Limitations and Considerations
While HRO principles offer a powerful framework for improving patient safety, it's crucial to acknowledge their limitations. Implementing HRO principles requires a significant investment of resources, including time, money, and personnel.
Moreover, HRO principles are not a panacea for all patient safety problems. They are most effective when applied to complex, high-risk processes where errors can have significant consequences. In situations where the underlying causes of errors are relatively simple and straightforward, other quality improvement methods may be more appropriate.
Furthermore, successful implementation of HRO principles requires a strong organizational culture that supports transparency, accountability, and continuous learning. Organizations must be willing to embrace change and invest in training and education to ensure that their employees understand and embrace HRO principles.
Looking Ahead: Optimizing HRO Implementation
The future of patient safety depends on our ability to effectively translate the theoretical principles of High Reliability Organizations into practical, real-world improvements. This requires a strategic approach that prioritizes concerns based on their potential for harm and the likelihood of success with HRO interventions.
By focusing on areas such as medication safety, surgical safety, and infection prevention, healthcare organizations can maximize the impact of their HRO initiatives and create a safer, more reliable environment for patients. Continuous monitoring and evaluation are essential to ensure that HRO principles are being effectively implemented and that they are leading to measurable improvements in patient safety outcomes.
Ultimately, the goal is to create a culture of safety where everyone in the organization is committed to preventing errors and learning from mistakes. This requires a collaborative effort involving clinicians, administrators, and patients, all working together to create a healthcare system that is truly worthy of our trust.

 (1).jpg)