Which Of The Following Can Contribute To Postoperative Infections
Postoperative infections, a dreaded complication of surgery, cast a long shadow on patient recovery and healthcare systems alike. These infections not only prolong hospital stays and increase healthcare costs but also pose a significant threat to patient well-being, potentially leading to severe complications and even mortality.
Identifying the factors that contribute to postoperative infections is crucial for implementing effective preventive measures and improving surgical outcomes. From the patient's own health status to the surgical environment and postoperative care practices, a multitude of elements can influence the risk of infection.
Understanding the Multifaceted Nature of Postoperative Infections
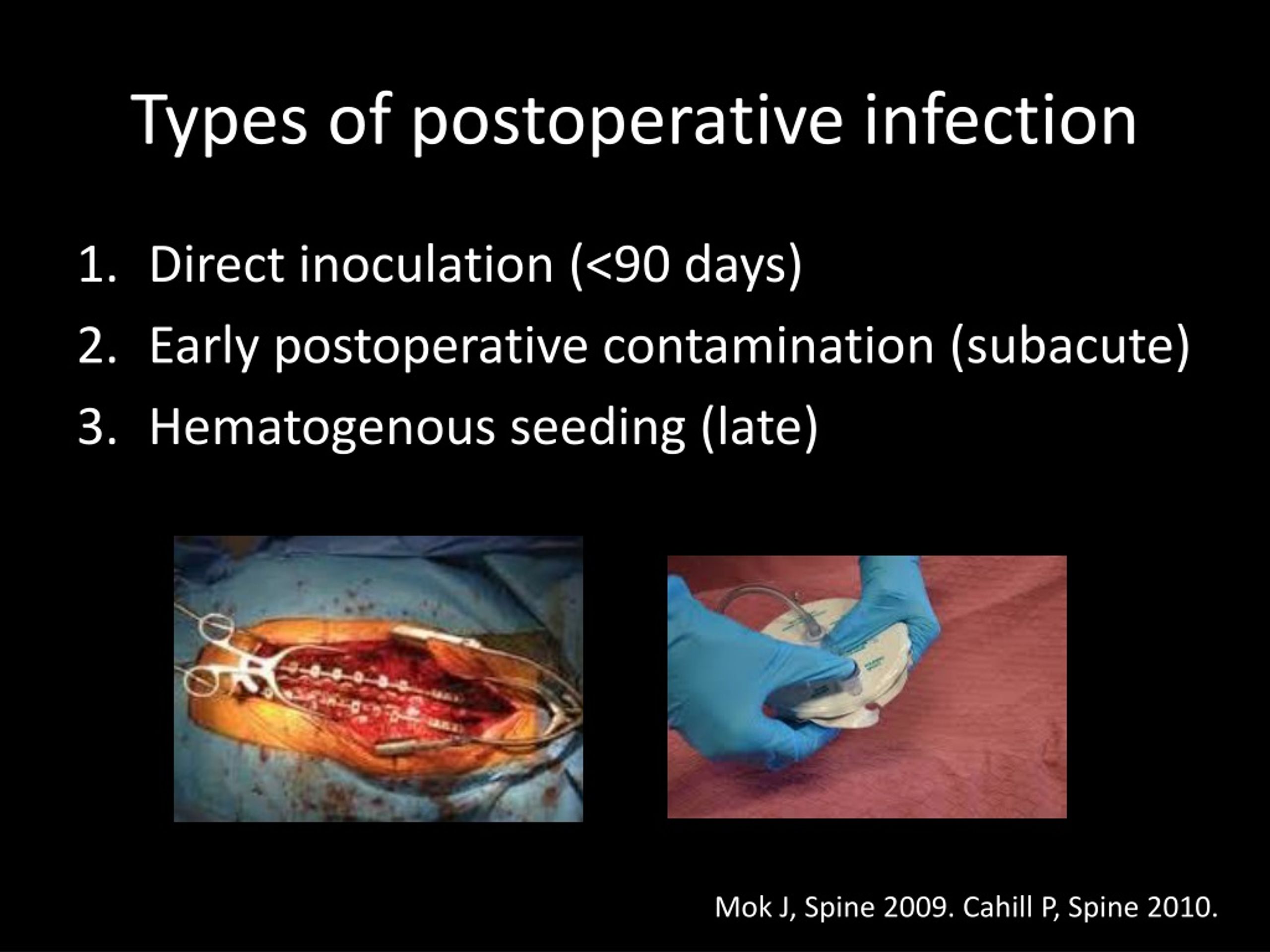
Postoperative infections, also known as surgical site infections (SSIs), occur when bacteria or other microorganisms invade the surgical site during or after an operation. According to the Centers for Disease Control and Prevention (CDC), SSIs are among the most common healthcare-associated infections in the United States, affecting hundreds of thousands of patients each year.
Patient-Related Risk Factors
A patient's overall health status plays a significant role in their susceptibility to postoperative infections. Individuals with pre-existing conditions such as diabetes, obesity, and compromised immune systems are at a higher risk.
Diabetes can impair the body's ability to fight off infection, while obesity can complicate surgical procedures and increase the risk of wound complications. Similarly, patients undergoing immunosuppressive therapy or those with conditions like HIV/AIDS are more vulnerable to infections.
Age is another important factor, with both very young and elderly patients being more susceptible to infection due to their less robust immune systems. Lifestyle choices, such as smoking and alcohol consumption, can also weaken the immune system and increase the risk of postoperative infections.
Surgical Technique and Environment
The surgical technique employed and the environment in which the surgery is performed are critical determinants of infection risk. Poor surgical technique, such as inadequate skin preparation or improper wound closure, can increase the likelihood of bacterial contamination.
A contaminated surgical environment, including improperly sterilized instruments or inadequate ventilation, can also introduce pathogens into the surgical site. Prolonged surgical duration is also a significant risk factor, as it increases the exposure time for the surgical site to potential contaminants.
The type of surgical procedure itself can influence the risk of infection. For instance, surgeries involving the gastrointestinal tract or those requiring the insertion of prosthetic materials are generally associated with a higher risk of infection.
Postoperative Care Practices
The quality of postoperative care significantly impacts the risk of infection. Inadequate wound care, such as infrequent dressing changes or improper hand hygiene, can allow bacteria to colonize the surgical site.
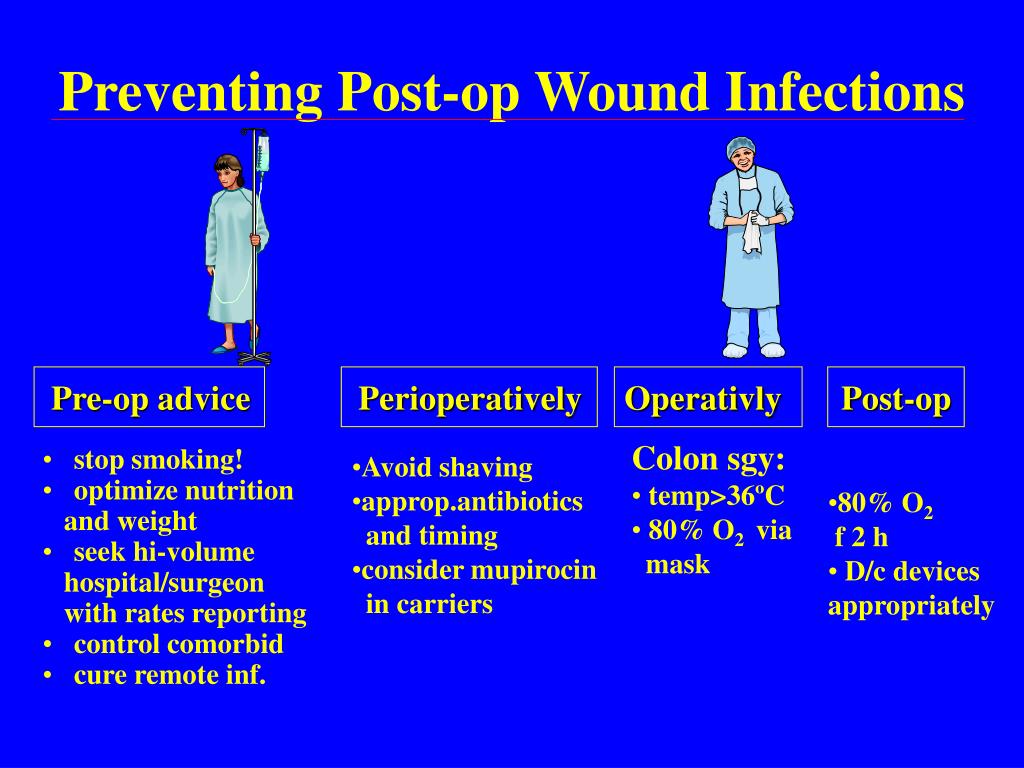
Failure to adhere to recommended antibiotic prophylaxis guidelines can also increase the risk of infection, particularly in high-risk patients or procedures. The CDC recommends that prophylactic antibiotics be administered within a specific timeframe before the incision is made to ensure adequate drug levels in the tissues.
Furthermore, healthcare-associated infections (HAIs) acquired during the postoperative period can contribute to SSIs. These infections can spread through contact with contaminated surfaces, equipment, or healthcare personnel who are not adhering to proper infection control practices.
Specific Contributory Factors in Detail
Several specific factors can significantly increase the risk of postoperative infections:
- Compromised Skin Integrity: Existing skin conditions like eczema or psoriasis can break the skin barrier, making it easier for bacteria to enter.
- Preoperative Shaving: Shaving the surgical site with a razor can create microscopic cuts, providing entry points for bacteria. Clipping hair is a safer alternative.
- Use of Foreign Materials: Implants, sutures, and other foreign materials can provide a surface for bacteria to adhere to and form biofilms, which are resistant to antibiotics.
- Blood Transfusions: Some studies have suggested that blood transfusions can increase the risk of postoperative infections, possibly due to their immunosuppressive effects.
- Hypothermia: Maintaining a patient's body temperature during surgery is crucial, as hypothermia can impair immune function and increase the risk of infection.
Preventive Measures and Future Directions
Preventing postoperative infections requires a multifaceted approach that addresses patient-related, surgical, and postoperative factors. Preoperative optimization of patient health, including controlling blood sugar levels in diabetic patients and encouraging smoking cessation, can significantly reduce the risk of infection.
Strict adherence to aseptic techniques in the operating room, including proper hand hygiene, sterilization of instruments, and appropriate skin preparation, is essential. Minimally invasive surgical techniques, when appropriate, can also reduce the risk of infection by minimizing tissue trauma and exposure.
Postoperative care protocols should emphasize meticulous wound care, adherence to antibiotic prophylaxis guidelines, and vigilant surveillance for signs of infection. Education of patients and their families about proper wound care and infection prevention practices is also crucial.
Ongoing research is focused on developing new strategies for preventing postoperative infections, including novel antimicrobial agents, improved surgical techniques, and enhanced infection control protocols. Furthermore, the development of rapid diagnostic tests for identifying infections early can facilitate prompt treatment and prevent complications.
By understanding the multifaceted nature of postoperative infections and implementing evidence-based preventive measures, healthcare professionals can significantly reduce the risk of these devastating complications and improve surgical outcomes for patients.