Which Of The Following Patient Beliefs Should The Clinician Identify
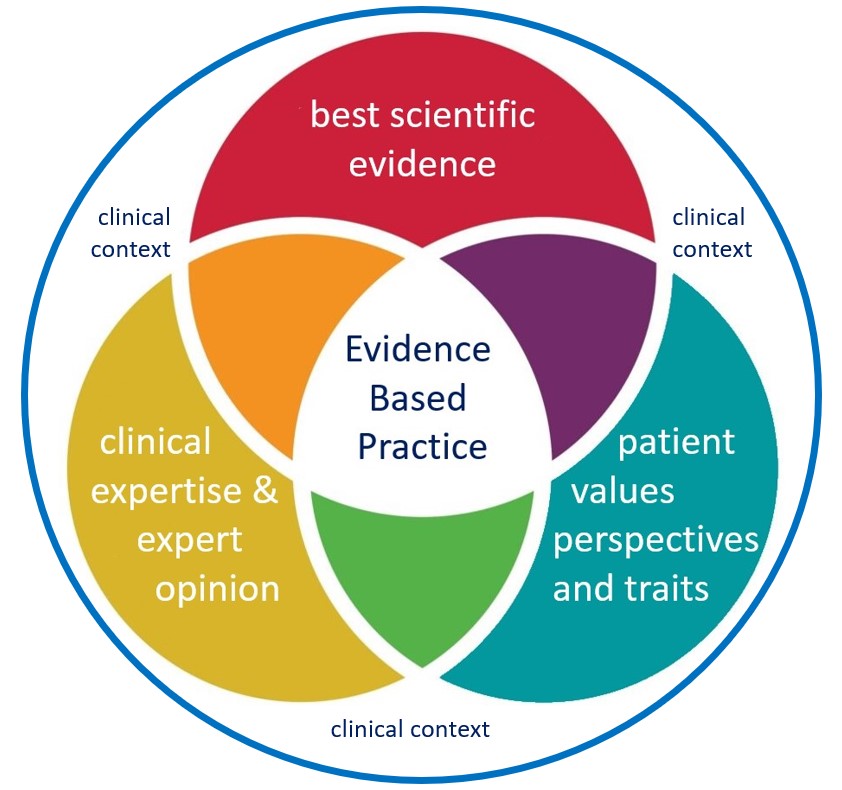
In the delicate dance between patient and clinician, understanding the patient's beliefs is not merely a courtesy, but a critical determinant of treatment success. Misaligned beliefs can lead to poor adherence, increased anxiety, and ultimately, worse health outcomes.
This article explores the key patient beliefs that clinicians should identify, focusing on their impact and offering insights into effective assessment and management strategies. It examines the intersection of patient perspectives, medical evidence, and the clinician's role in navigating these complex interactions, ultimately aiming to improve patient care and outcomes.
The Nut Graf: Unveiling Beliefs for Better Care
The goal of identifying patient beliefs isn't about imposing a medical worldview, but rather understanding the lens through which individuals perceive their health. This understanding allows clinicians to tailor interventions, improve communication, and foster trust, ultimately leading to better outcomes.
Specifically, clinicians should focus on beliefs about the illness itself, the proposed treatment, the healthcare system, and the clinician's role. By actively exploring these belief systems, healthcare providers can bridge the gap between medical knowledge and patient experience, creating a more collaborative and effective therapeutic alliance.
Illness Perceptions: Understanding the "Why" Behind the Symptoms
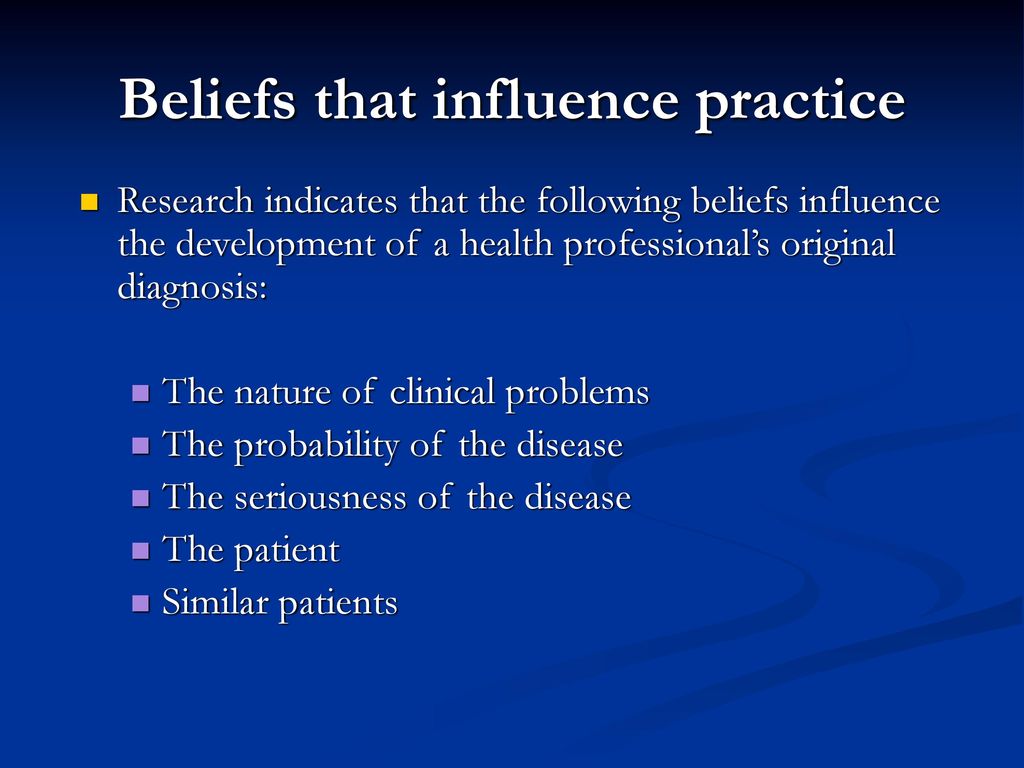
A patient's perception of their illness, including its cause, severity, and consequences, significantly impacts their behavior. For instance, a patient who believes their back pain is due to a minor muscle strain will likely behave differently than someone who fears a more serious spinal condition.
The Common Sense Model of Self-Regulation (CSM) highlights several key dimensions of illness perceptions, including identity (labels and symptoms), cause, timeline, consequences, and controllability/curability. Understanding these dimensions allows clinicians to predict and address potential barriers to adherence and self-management.
Tools like the Brief Illness Perception Questionnaire (BIPQ) can help assess these perceptions efficiently. Such assessment allows the clinician to quickly understand the patient's perspective.
Treatment Beliefs: Navigating Expectations and Concerns
Beliefs about the proposed treatment, including its effectiveness, potential side effects, and necessity, are crucial predictors of adherence. Patients often hold pre-conceived notions about medications, therapies, or lifestyle changes, which can stem from personal experiences, anecdotes, or media reports.
Addressing these beliefs proactively is essential. For example, a patient with negative beliefs about statins due to concerns about muscle pain is less likely to take the medication as prescribed, even if it's medically necessary.
Clinicians should engage in open and honest discussions, providing evidence-based information and addressing specific concerns. This helps align patient expectations with the realities of treatment.
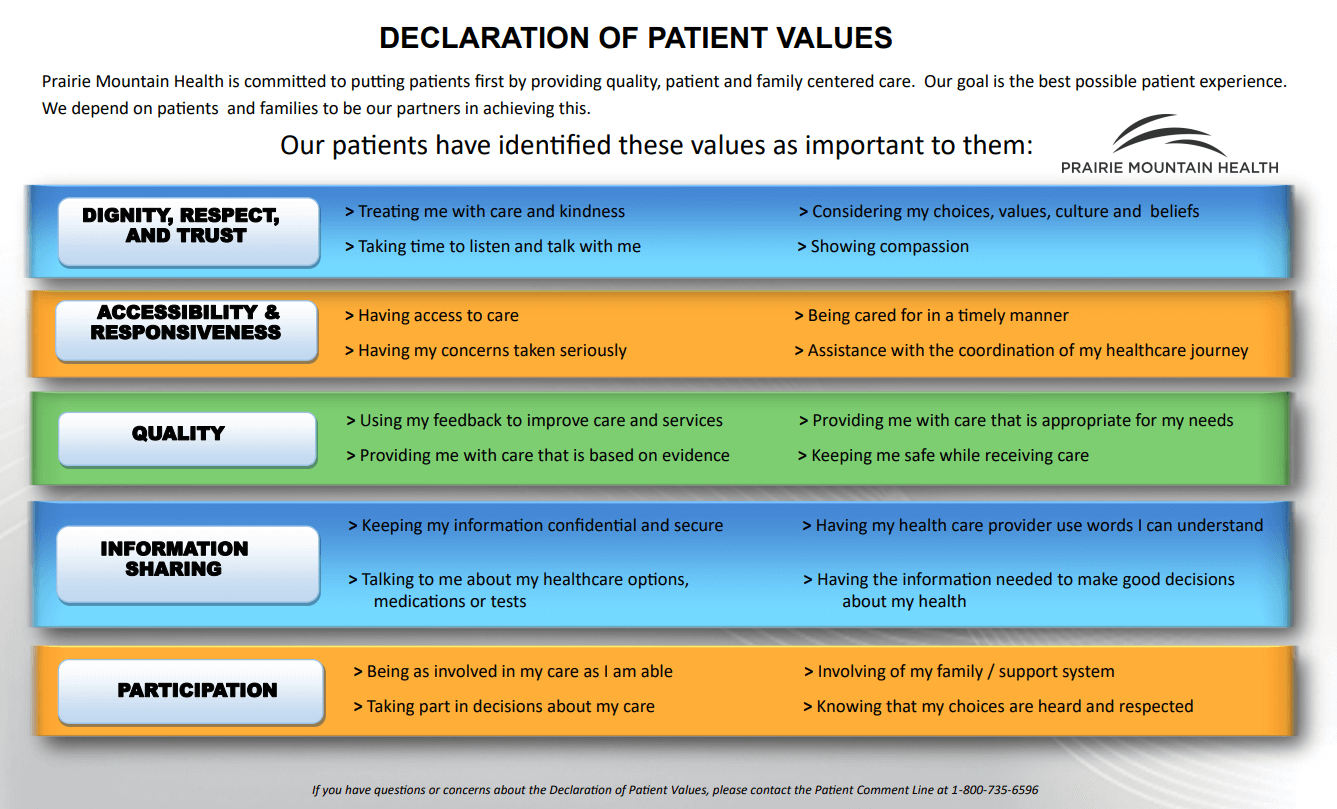
Beliefs About the Healthcare System: Trust and Access
A patient's beliefs about the healthcare system can significantly influence their engagement and trust. Experiences with previous healthcare encounters, cultural beliefs, and socioeconomic factors can shape these perceptions. These can profoundly impact the success of medical treatment.
Distrust in the medical system, often rooted in historical injustices or perceived biases, can lead to reluctance to seek care or follow medical advice. Financial barriers, language difficulties, and lack of access to transportation can also create significant obstacles.
Building rapport and demonstrating empathy can help overcome these barriers. Culturally sensitive communication and advocacy for improved access are essential for fostering trust and promoting equitable healthcare.
Beliefs About the Clinician: The Power of the Therapeutic Relationship
Patients' beliefs about their clinician's competence, empathy, and trustworthiness play a vital role in the therapeutic relationship. A strong and positive relationship is often associated with improved adherence, satisfaction, and outcomes.
Patients are more likely to adhere to recommendations from clinicians they perceive as knowledgeable, caring, and respectful. Conversely, negative perceptions can lead to skepticism and resistance.
Active listening, clear communication, and shared decision-making are crucial for building a strong clinician-patient relationship. Transparency and honesty contribute significantly to establishing trust and facilitating open dialogue.
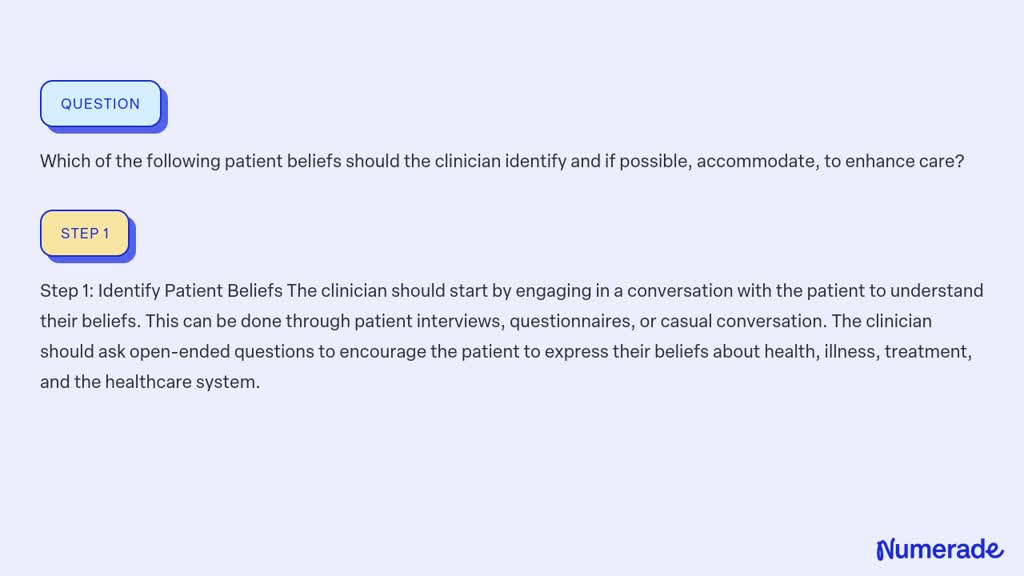
Strategies for Identifying and Addressing Patient Beliefs
Several strategies can help clinicians identify and address patient beliefs effectively. One is active listening, involving paying attention to both verbal and nonverbal cues, asking clarifying questions, and reflecting back what the patient has said.
Using open-ended questions, such as "What are your thoughts about this medication?" or "What are your biggest concerns about this treatment?" can encourage patients to express their beliefs freely. The use of simple language is also helpful.
Motivational Interviewing (MI) is a patient-centered communication style that can help explore and resolve ambivalence about treatment. MI emphasizes collaboration, empathy, and autonomy support.
The Ethical Considerations
It's crucial to remember that identifying and addressing patient beliefs must be done ethically. Respect for patient autonomy and cultural sensitivity are paramount. Clinicians should not attempt to impose their own beliefs or values on patients.
Shared decision-making, where the clinician and patient collaboratively weigh the evidence-based options and the patient's values, is the ethical standard. This helps ensure that treatment decisions are aligned with the patient's goals and preferences.
Documenting the patient's beliefs and the strategies used to address them in the medical record ensures continuity of care and facilitates communication among healthcare providers.
Looking Ahead: The Future of Belief-Centered Care
As healthcare becomes increasingly patient-centered, the importance of understanding patient beliefs will only grow. Future research should focus on developing more effective tools and strategies for assessing and addressing these beliefs in diverse populations.
Integrating belief-centered care into medical education and training is also essential. This will equip future clinicians with the skills and knowledge to engage in meaningful conversations with patients about their beliefs and values.
Ultimately, by recognizing and respecting the diverse belief systems of our patients, we can create a more compassionate, effective, and equitable healthcare system. This system must ensure better health outcomes for all.