Which Of The Following Statements About Insulin Is True
Confusion and misinformation surrounding insulin, a life-saving hormone for millions, can have serious consequences. Understanding the facts about insulin is crucial for individuals with diabetes, their families, and the general public. This article aims to clarify some common misconceptions and provide accurate information based on scientific evidence and expert consensus.
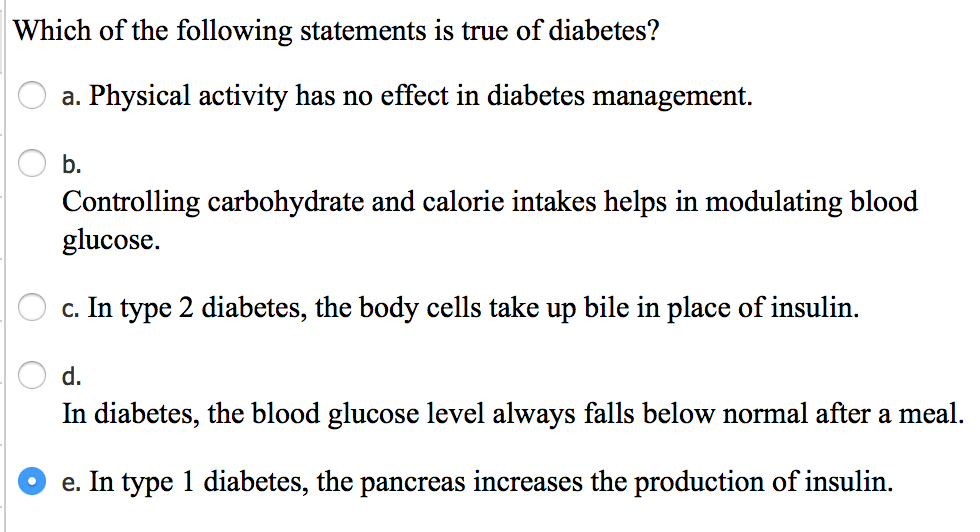
Insulin is a hormone produced by the pancreas that allows glucose, a type of sugar, to enter cells and provide them with energy. In individuals with diabetes, the pancreas either doesn't produce enough insulin (Type 1 diabetes) or the body doesn't respond effectively to the insulin that is produced (Type 2 diabetes). This leads to elevated blood glucose levels, which can cause a range of health problems if left unmanaged.
The Essential Role of Insulin
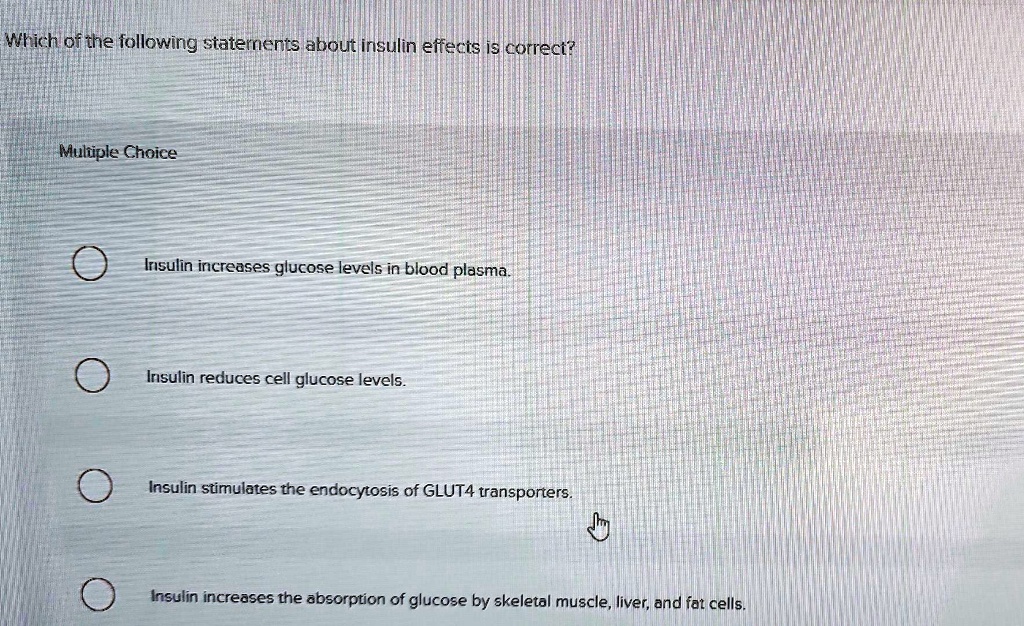
The primary function of insulin is to regulate blood glucose levels. After eating, carbohydrates are broken down into glucose, which then enters the bloodstream. Insulin acts as a key, unlocking cells to allow glucose to enter, thus lowering blood glucose levels.
Without sufficient insulin, glucose remains in the bloodstream, leading to hyperglycemia. Over time, this can damage blood vessels, nerves, and organs, increasing the risk of heart disease, kidney disease, blindness, and nerve damage.
Common Misconceptions About Insulin
One common misconception is that insulin is only for people with severe diabetes. In reality, insulin is essential for managing both Type 1 and Type 2 diabetes when other treatments, such as diet, exercise, and oral medications, are not sufficient to control blood glucose levels.
Another myth is that insulin is a "last resort" or a sign of failure in diabetes management. Initiating insulin therapy when needed is a proactive step to protect against long-term complications. Delaying insulin treatment when indicated can actually lead to more serious health issues.
Insulin Types and Delivery Methods
Several types of insulin are available, each differing in its onset, peak, and duration of action. These include rapid-acting, short-acting, intermediate-acting, and long-acting insulins. The specific type of insulin prescribed depends on individual needs and lifestyle factors.
Insulin can be administered through various methods. These include syringes, insulin pens, and insulin pumps. Insulin pumps provide a continuous infusion of insulin, mimicking the body's natural insulin release more closely.
The Truth About Insulin and Weight Gain
It's true that insulin can contribute to weight gain in some individuals. However, weight gain associated with insulin is often due to improved glucose control. As glucose enters cells, it can be used for energy or stored as glycogen or fat.
Properly managing insulin doses and adopting a healthy lifestyle, including a balanced diet and regular exercise, can help mitigate weight gain associated with insulin therapy. Work closely with your healthcare provider or registered dietitian.
The Importance of Monitoring and Education
Effective insulin therapy requires careful monitoring of blood glucose levels. This allows individuals to adjust their insulin doses as needed to maintain optimal control.
Diabetes education is crucial for people who take insulin. Education programs provide essential information about insulin administration, blood glucose monitoring, carbohydrate counting, and managing hypoglycemia (low blood glucose) and hyperglycemia.
"Empowering patients with knowledge and tools to manage their diabetes is key to achieving positive health outcomes," says Dr. Emily Carter, an endocrinologist at the National Institutes of Health.
Hypoglycemia is a potential side effect of insulin therapy. Recognizing the symptoms of hypoglycemia, such as shakiness, sweating, confusion, and dizziness, is crucial for prompt treatment. Carrying a source of fast-acting glucose, like glucose tablets or juice, is essential.
Advancements in Insulin Therapy
Ongoing research continues to advance insulin therapy. New insulins with improved profiles and more convenient delivery methods are constantly being developed. These advancements aim to improve glucose control, reduce the risk of hypoglycemia, and enhance the quality of life for people with diabetes.
Artificial pancreas systems, also known as closed-loop systems, are becoming increasingly sophisticated. These systems automatically monitor blood glucose levels and adjust insulin delivery accordingly, minimizing the need for manual adjustments.
Conclusion
Insulin is a vital medication for managing diabetes and preventing serious complications. Understanding the facts about insulin, including its role in glucose regulation, different types and delivery methods, and potential side effects, is crucial for effective diabetes management. Open communication with healthcare providers, continuous monitoring, and ongoing education are essential components of successful insulin therapy.