Which Product Results From The Breakdown Of Fibrin

The human body, a marvel of biological engineering, constantly works to maintain equilibrium. One critical process, hemostasis – the cessation of bleeding – involves a complex cascade of events. What happens after the clot has served its purpose? What are the resulting products when the body breaks down fibrin, the protein that forms the meshwork of a blood clot?
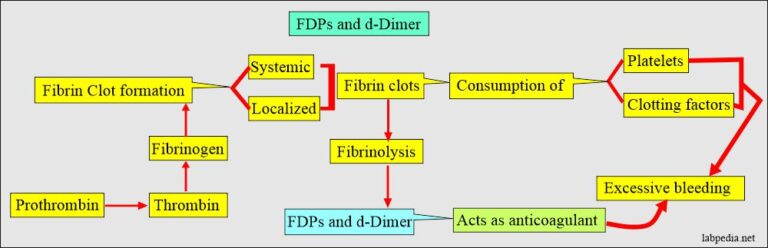
Understanding the breakdown products of fibrin, specifically fibrin degradation products (FDPs) and D-dimer, is crucial in diagnosing and managing various medical conditions. These substances serve as biomarkers, providing valuable insights into the body's coagulation and fibrinolytic systems. Their presence and concentration can indicate conditions ranging from deep vein thrombosis (DVT) to disseminated intravascular coagulation (DIC).
The Role of Fibrin and Its Degradation
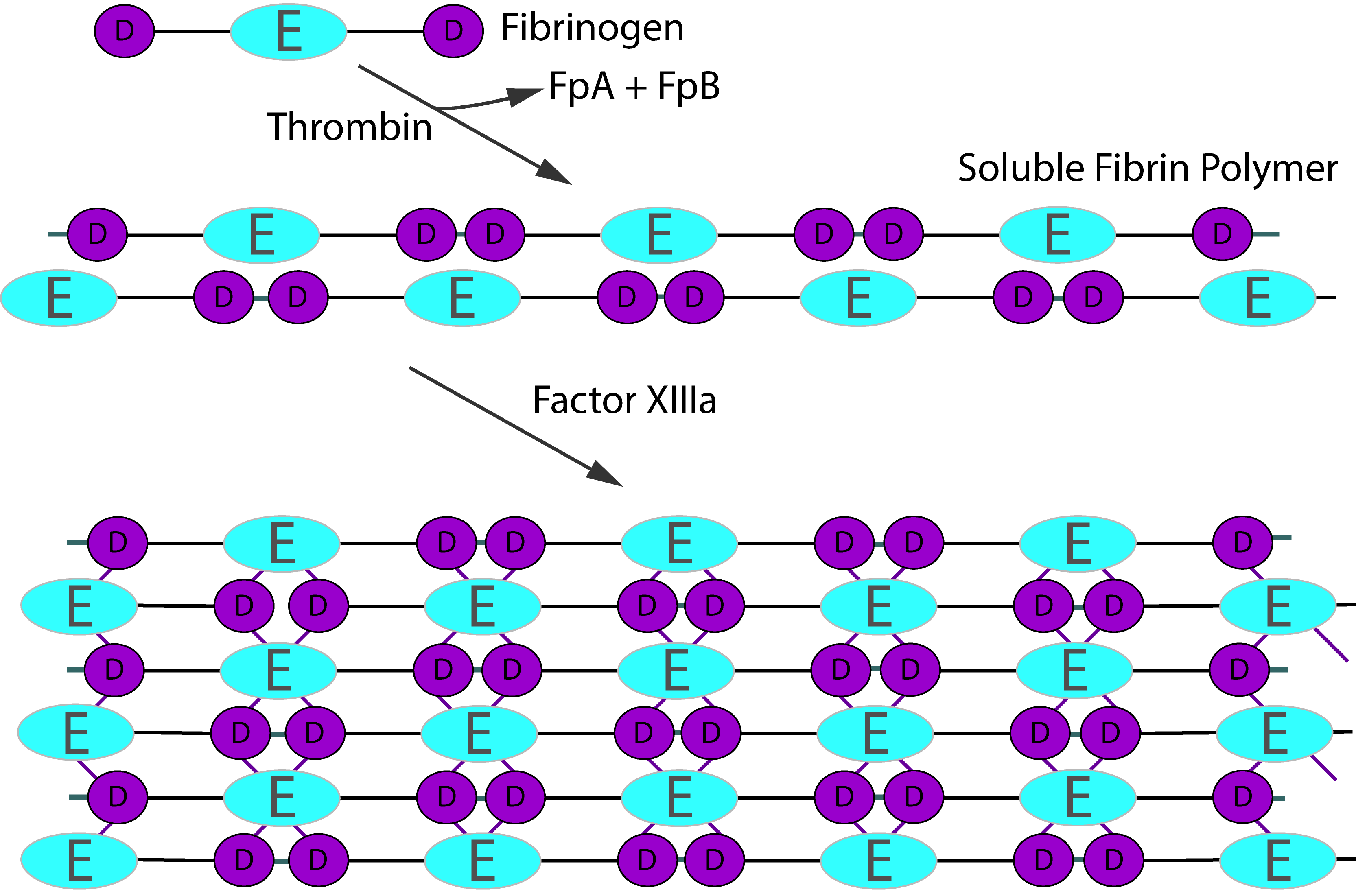
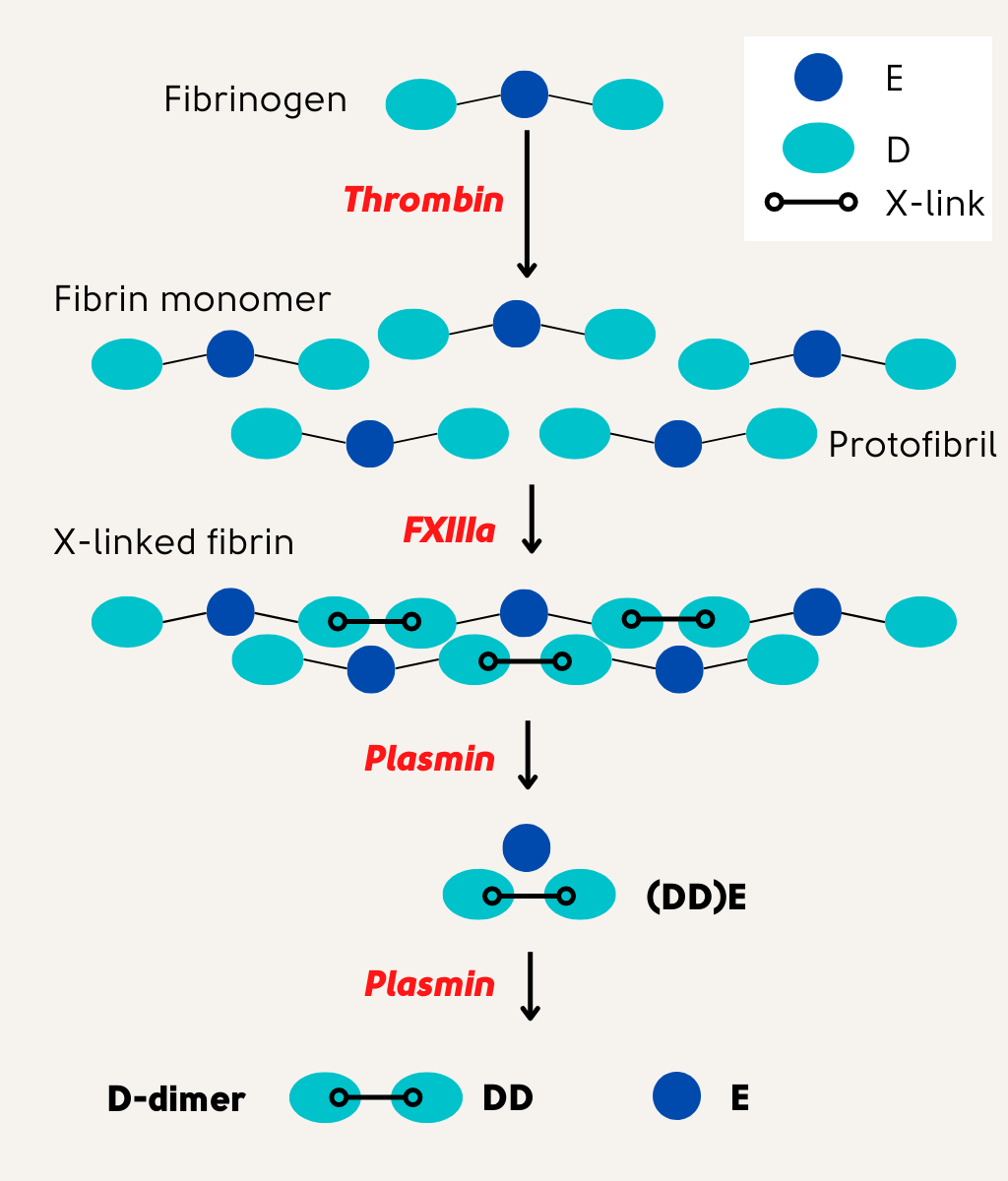
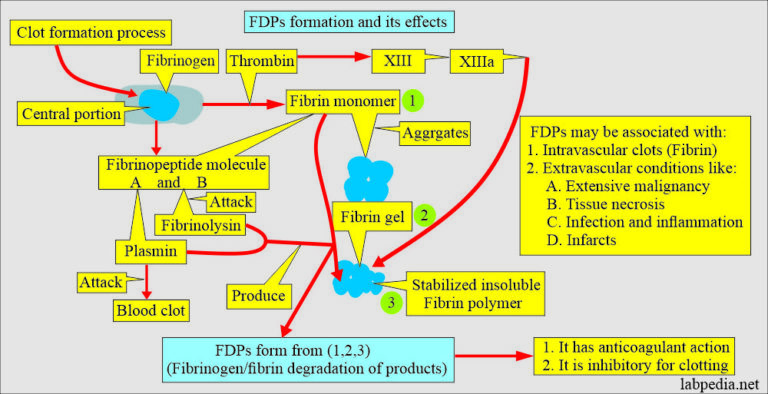
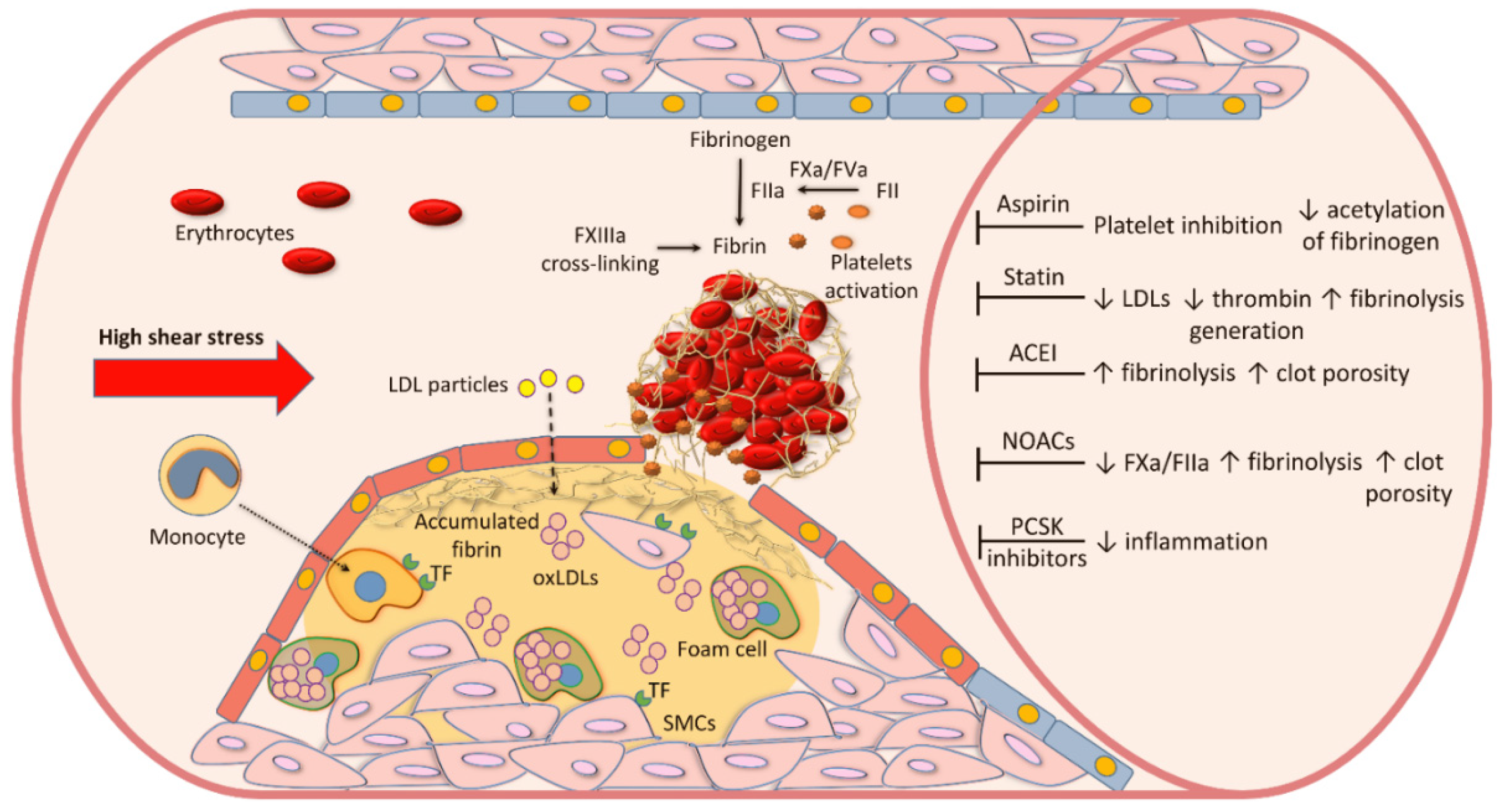
Fibrin is the primary structural component of blood clots. It’s formed from fibrinogen through the action of thrombin during the coagulation cascade. Once a blood vessel is repaired, the clot needs to be broken down in a process known as fibrinolysis.
This process involves plasmin, an enzyme that cleaves fibrin into smaller fragments. These fragments are collectively known as fibrin degradation products (FDPs). The breakdown of fibrin is a tightly regulated process, essential for maintaining vascular patency and preventing excessive clot formation.
Key Fibrin Degradation Products
While the term FDPs encompasses a range of fragments, D-dimer stands out as clinically significant. D-dimer is a specific FDP that results from the breakdown of cross-linked fibrin. Its presence strongly suggests that both coagulation and fibrinolysis have occurred.
Other FDPs include fragments X, Y, D, and E. These fragments are sequentially generated as plasmin digests fibrin. Each fragment contributes to the overall pool of FDPs measured in diagnostic tests, though D-dimer is often assessed separately due to its higher specificity for cross-linked fibrin degradation.
Clinical Significance of FDPs and D-dimer
Elevated levels of FDPs and D-dimer can indicate various underlying medical conditions. These biomarkers are particularly useful in the diagnosis and management of thromboembolic disorders.
Deep vein thrombosis (DVT) and pulmonary embolism (PE) are two common conditions where D-dimer testing plays a crucial role. A negative D-dimer result can effectively rule out these conditions in patients with low to intermediate clinical probability. However, a positive D-dimer requires further investigation, such as imaging studies, to confirm the diagnosis.
D-dimer levels are also elevated in other conditions, including disseminated intravascular coagulation (DIC), a life-threatening condition characterized by widespread activation of the coagulation system. Other conditions that may increase D-dimer include pregnancy, surgery, trauma, and certain cancers.
Diagnostic Testing and Interpretation
D-dimer testing is typically performed using immunoassays. These assays detect and quantify the amount of D-dimer in a blood sample.
The interpretation of D-dimer results requires careful consideration of the patient's clinical context. Factors such as age, pregnancy status, and the presence of other medical conditions can influence D-dimer levels. A healthcare professional must correlate the test results with the patient's symptoms and medical history to arrive at an accurate diagnosis.
Limitations of D-dimer Testing
While D-dimer testing is a valuable diagnostic tool, it has limitations. D-dimer levels can be elevated in various non-thrombotic conditions, leading to false-positive results.
Additionally, the sensitivity of D-dimer assays may vary depending on the specific assay used. Therefore, it is important to use a standardized and validated assay and to interpret the results in conjunction with clinical findings. Age-adjusted D-dimer cutoffs are now commonly used to improve the specificity of the test in older patients.
Future Directions and Research
Ongoing research is focused on improving the accuracy and specificity of D-dimer testing. This includes the development of novel assays that can differentiate between different types of D-dimer fragments.
Researchers are also investigating the potential of using D-dimer levels to monitor the effectiveness of anticoagulant therapy. Furthermore, studies are exploring the role of D-dimer in predicting the risk of recurrent venous thromboembolism.
Understanding the nuances of fibrin degradation and the clinical significance of its products, particularly D-dimer, remains paramount in modern medicine. As research progresses, we can anticipate even more refined diagnostic and therapeutic strategies centered around these vital biomarkers.



-elisa-kit.jpg)



![Which Product Results From The Breakdown Of Fibrin Fibrinogen Degradation Products [FDPs]](https://www.practical-haemostasis.com/images/Images-2/Fibrinolysis/Fibrinogen Degradation by Plasmin.png)

.jpg)