Which Statement About Schizophrenia Is True

Imagine a world where whispers turn into shouts, shadows dance with menacing intent, and the very fabric of reality seems to fray at the edges. This is a glimpse into the lives of individuals living with schizophrenia, a complex and often misunderstood brain disorder. It’s a world far removed from the caricatures often portrayed in popular culture, a world that deserves our empathy and understanding.
The persistent myths surrounding schizophrenia often overshadow the reality of those affected. This article aims to dispel these misconceptions by addressing a crucial question: Which statement about schizophrenia is true? Understanding the truth is the first step towards fostering a more supportive and informed community.
Unraveling the Misconceptions
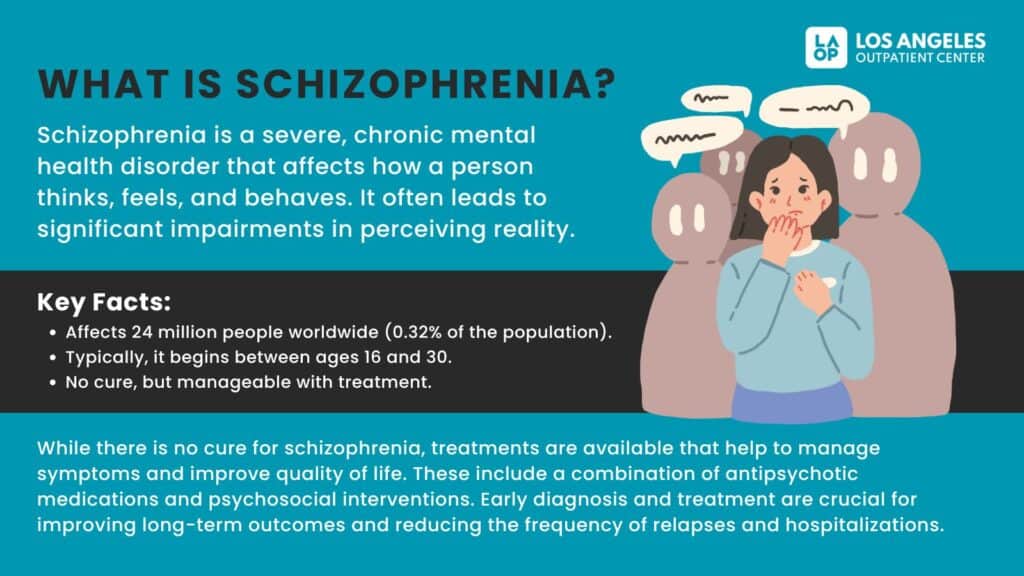
Schizophrenia is a chronic brain disorder that affects a person's ability to think, feel, and behave clearly. According to the National Institute of Mental Health (NIMH), it is characterized by a combination of positive symptoms (like hallucinations and delusions), negative symptoms (like blunted emotions and social withdrawal), and cognitive symptoms (like difficulties with memory and attention).
One of the most damaging misconceptions is that schizophrenia is synonymous with a "split personality" or multiple personality disorder (now known as Dissociative Identity Disorder). This is absolutely false. Schizophrenia involves a disruption in thought processes, perception, and emotional responsiveness, not the presence of distinct personalities.
Another common myth paints those with schizophrenia as inherently violent. While individuals experiencing psychosis may, in rare instances, exhibit agitated behavior, studies show they are more likely to be victims of violence than perpetrators. The American Psychiatric Association emphasizes that violence is not a core symptom of schizophrenia, and many individuals with the condition live peaceful, productive lives.
The belief that schizophrenia is untreatable is also deeply inaccurate. While there is no cure, a combination of medication, therapy, and psychosocial support can significantly improve a person's quality of life and ability to manage their symptoms. Early intervention is key to better outcomes.
The True Statement: A Multifaceted Approach to Understanding
So, which statement about schizophrenia is true? The most accurate statement is this: Schizophrenia is a treatable brain disorder characterized by a range of symptoms that can be effectively managed with a combination of medication, therapy, and psychosocial support, allowing individuals to lead meaningful and fulfilling lives.
This statement acknowledges the complexity of the condition, highlighting its biological basis and the importance of comprehensive treatment. It moves away from stigmatizing labels and emphasizes the potential for recovery and well-being. But to fully grasp the significance of this statement, we need to delve deeper into the roots of the disorder and the advancements in its treatment.
A Look at the Past
Historically, individuals with schizophrenia faced unimaginable hardships. Before the advent of antipsychotic medications in the mid-20th century, treatment options were limited, often involving institutionalization and harsh, ineffective procedures.
Mental asylums, often overcrowded and understaffed, became repositories for those deemed "insane," with little hope for recovery. The stigma surrounding mental illness was pervasive, leading to social isolation and discrimination. It was a dark chapter in the history of mental health care.
The development of chlorpromazine in the 1950s marked a turning point. This first-generation antipsychotic medication helped to reduce positive symptoms like hallucinations and delusions, offering a glimmer of hope for those who had previously been considered beyond help.
Advances in Treatment and Understanding
Since then, significant strides have been made in understanding the neurobiological basis of schizophrenia. Brain imaging studies have revealed structural and functional differences in the brains of individuals with the disorder, particularly in areas related to thinking, perception, and emotion. Research suggests that genetic factors, environmental influences, and neurochemical imbalances all play a role.
Second-generation antipsychotics, introduced in the 1990s, offer improved side effect profiles compared to their predecessors. These medications target a wider range of neurotransmitters, potentially addressing both positive and negative symptoms. However, they can still cause metabolic side effects, such as weight gain and increased risk of diabetes, requiring careful monitoring.
Therapy plays a crucial role in helping individuals with schizophrenia manage their symptoms and improve their quality of life. Cognitive Behavioral Therapy (CBT) can help individuals challenge and modify distorted thought patterns, while social skills training can improve communication and social interaction.
The Importance of Psychosocial Support
Psychosocial support, including family therapy, supported employment, and peer support groups, is essential for promoting recovery and reducing relapse rates. Creating a supportive environment can help individuals regain a sense of purpose and belonging.
Early intervention programs, particularly for young people experiencing their first episode of psychosis, have shown promising results. These programs provide coordinated care, including medication management, therapy, and social support, with the aim of preventing long-term disability.
Beyond the Diagnosis: Human Stories
It's crucial to remember that behind every diagnosis is a human being with hopes, dreams, and aspirations. Individuals with schizophrenia are not defined by their illness. They are students, artists, employees, parents, and friends.
Many individuals with schizophrenia have achieved remarkable success in their chosen fields, demonstrating resilience and determination in the face of adversity. Their stories serve as a powerful reminder that recovery is possible, and that individuals with schizophrenia can lead fulfilling lives.
Elyn Saks, a renowned professor of law, has openly shared her experiences with schizophrenia in her memoir, "The Center Cannot Hold." Her story is a testament to the power of treatment and the importance of challenging stigma.
Moving Forward: Towards a More Compassionate Future
The journey of understanding and treating schizophrenia is ongoing. Continued research is needed to develop more effective medications, improve therapeutic interventions, and reduce the stigma associated with the condition.
Increased access to mental health care is crucial, particularly in underserved communities. Early intervention programs, comprehensive treatment options, and supportive services should be readily available to all who need them.
Ultimately, creating a more compassionate future for individuals with schizophrenia requires a shift in societal attitudes. By challenging misconceptions, promoting understanding, and fostering empathy, we can create a world where everyone has the opportunity to thrive.
Let us remember that mental health is an integral part of overall well-being. By embracing this truth, we can begin to build a society that values and supports the mental health of all its members.