Which Vitamin Deficiency Leads To Hemolytic Anemia
Imagine a vibrant garden, teeming with life and color. Each bloom, a testament to the sun's nourishment and the soil's rich bounty. Now, picture that garden slowly fading, the leaves yellowing, the blooms withering, a consequence of a missing nutrient. Our bodies, much like that garden, require specific vitamins to thrive. When one is deficient, the effects can be devastating, leading to conditions like hemolytic anemia, a condition where red blood cells are destroyed faster than they can be made.
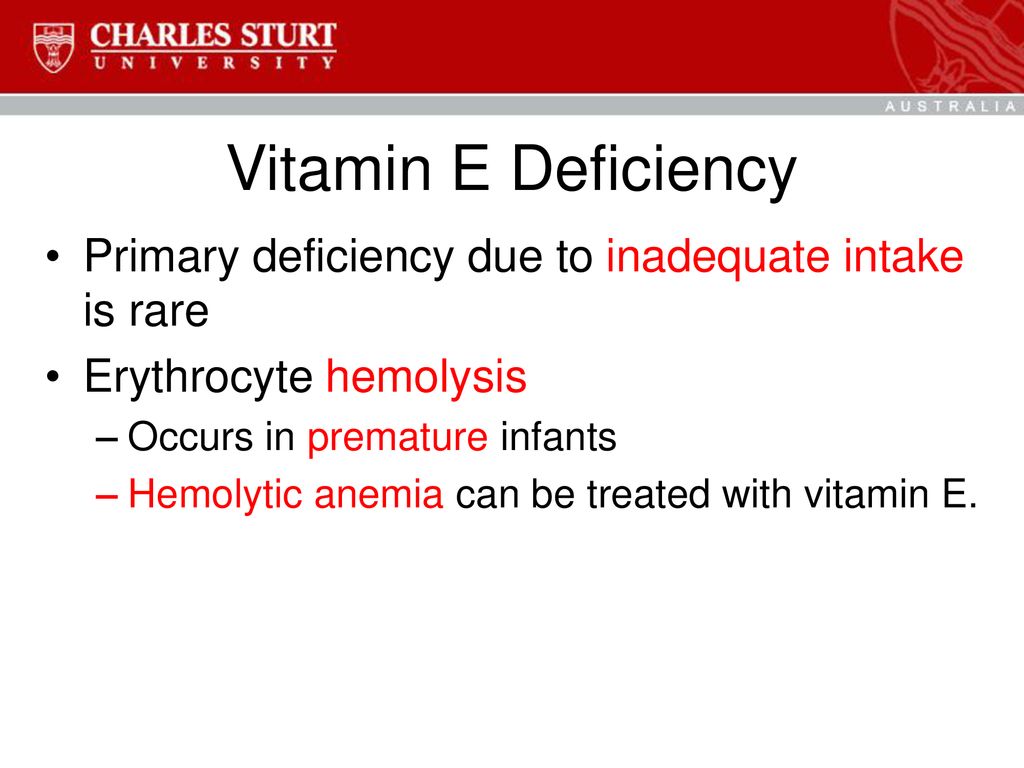
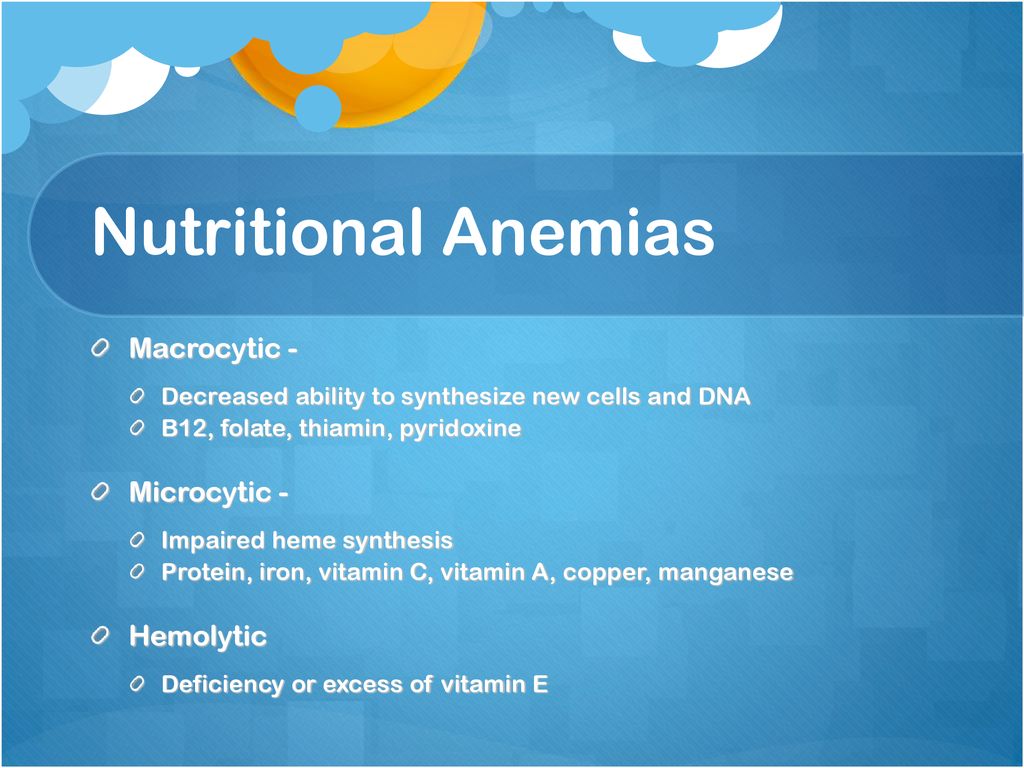
The spotlight of this article shines on Vitamin E, a fat-soluble nutrient often overlooked, yet crucial for protecting our red blood cells. Understanding the connection between Vitamin E deficiency and hemolytic anemia is essential for maintaining optimal health, particularly for vulnerable populations like premature infants and individuals with certain malabsorption conditions.
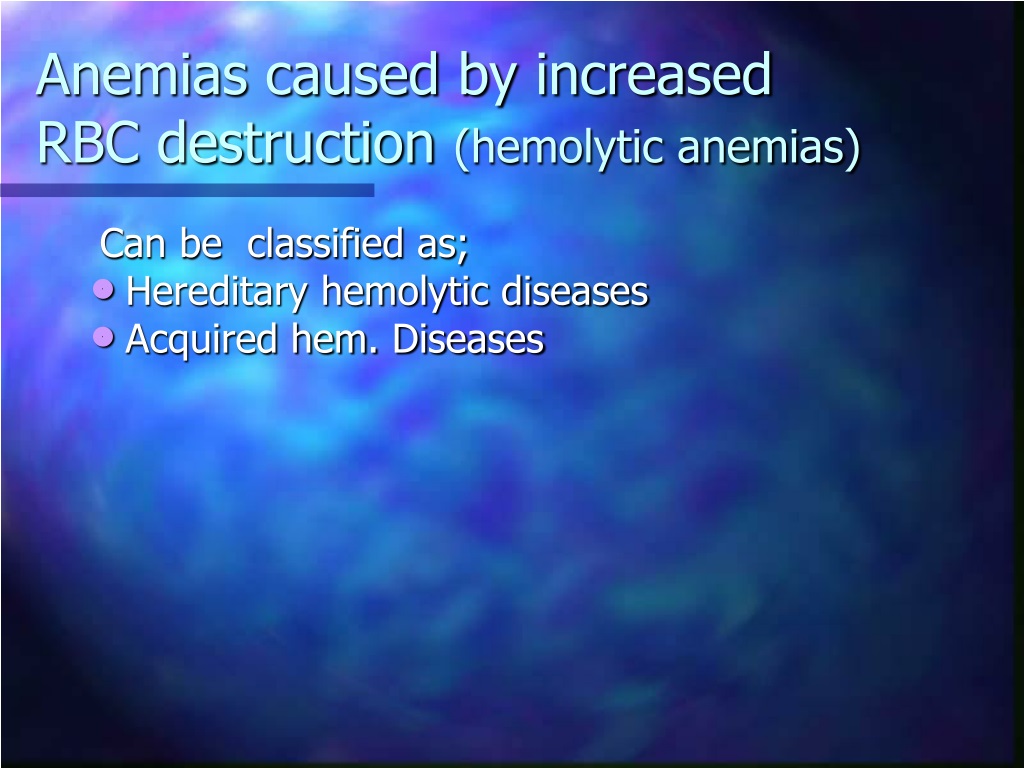
Hemolytic anemia, at its core, is a condition characterized by the premature destruction of red blood cells. Red blood cells, the tireless transporters of oxygen throughout our bodies, have a lifespan of roughly 120 days. In hemolytic anemia, this lifespan is significantly shortened, leading to a shortage of red blood cells. This shortage deprives tissues and organs of the oxygen they need, resulting in fatigue, weakness, shortness of breath, and jaundice (yellowing of the skin and eyes).
The Role of Vitamin E
Vitamin E, a potent antioxidant, plays a critical role in protecting the integrity of cell membranes. It acts as a shield, defending the delicate lipids within these membranes from the damaging effects of oxidation caused by free radicals. Red blood cells, constantly exposed to oxygen, are particularly vulnerable to oxidative stress. Vitamin E stands guard, preventing these cells from becoming fragile and prematurely destroyed.
Without sufficient Vitamin E, the cell membranes of red blood cells become susceptible to damage. This damage leads to hemolysis, the bursting of red blood cells, triggering hemolytic anemia.
Who is at Risk?
While Vitamin E deficiency is relatively rare in healthy adults, certain groups face a higher risk. Premature infants, who are born with limited stores of Vitamin E, are particularly vulnerable. Their immature digestive systems also struggle to absorb fats effectively, further hindering Vitamin E absorption.
Individuals with fat malabsorption disorders, such as cystic fibrosis, Crohn's disease, and short bowel syndrome, also struggle to absorb Vitamin E effectively. These conditions impair the body's ability to break down and absorb fats from food, leading to a deficiency of fat-soluble vitamins like Vitamin E.
Rare genetic disorders, such as abetalipoproteinemia, can also disrupt the absorption and transport of fats, leading to severe Vitamin E deficiency and subsequent hemolytic anemia.
Diagnosing and Treating Vitamin E Deficiency-Induced Hemolytic Anemia
Diagnosing Vitamin E deficiency-induced hemolytic anemia involves a comprehensive evaluation. Doctors will typically assess a patient's medical history, conduct a physical examination, and order blood tests to measure Vitamin E levels and evaluate red blood cell counts and other relevant markers.
Treatment for Vitamin E deficiency-induced hemolytic anemia primarily involves Vitamin E supplementation. The dosage and duration of supplementation will depend on the severity of the deficiency and the underlying cause.
For premature infants, Vitamin E supplementation is often administered carefully under medical supervision. For individuals with fat malabsorption disorders, addressing the underlying condition and optimizing fat absorption are crucial alongside Vitamin E supplementation.
Foods Rich in Vitamin E
While supplementation is often necessary to correct a deficiency, incorporating Vitamin E-rich foods into the diet is a proactive way to maintain healthy levels. Excellent sources of Vitamin E include vegetable oils (wheat germ, sunflower, safflower), nuts (almonds, hazelnuts, peanuts), seeds (sunflower seeds), and green leafy vegetables (spinach, broccoli).
Consuming a balanced diet rich in these foods can contribute to overall health and well-being, helping to prevent Vitamin E deficiency and its associated complications.
Maintaining adequate Vitamin E levels is crucial not only for preventing hemolytic anemia but also for supporting overall health. Its antioxidant properties extend beyond red blood cell protection, contributing to immune function, eye health, and potentially even reducing the risk of chronic diseases.
Looking Ahead
Continued research into the intricate relationship between Vitamin E and red blood cell health is essential. Further studies are needed to better understand the optimal Vitamin E intake for various populations and to develop more effective strategies for preventing and treating Vitamin E deficiency-induced hemolytic anemia.
Raising awareness about the importance of Vitamin E and its potential impact on red blood cell health is key. Educating healthcare professionals and the public about the risk factors, symptoms, and treatment options for Vitamin E deficiency-induced hemolytic anemia can help ensure timely diagnosis and intervention.
Just like that garden, our bodies flourish with the right nourishment. Vitamin E, a seemingly small nutrient, plays a monumental role in protecting our red blood cells and ensuring that our bodies receive the oxygen they need to thrive. By understanding its significance and taking proactive steps to maintain healthy levels, we can cultivate a vibrant inner garden, rich with vitality and well-being.



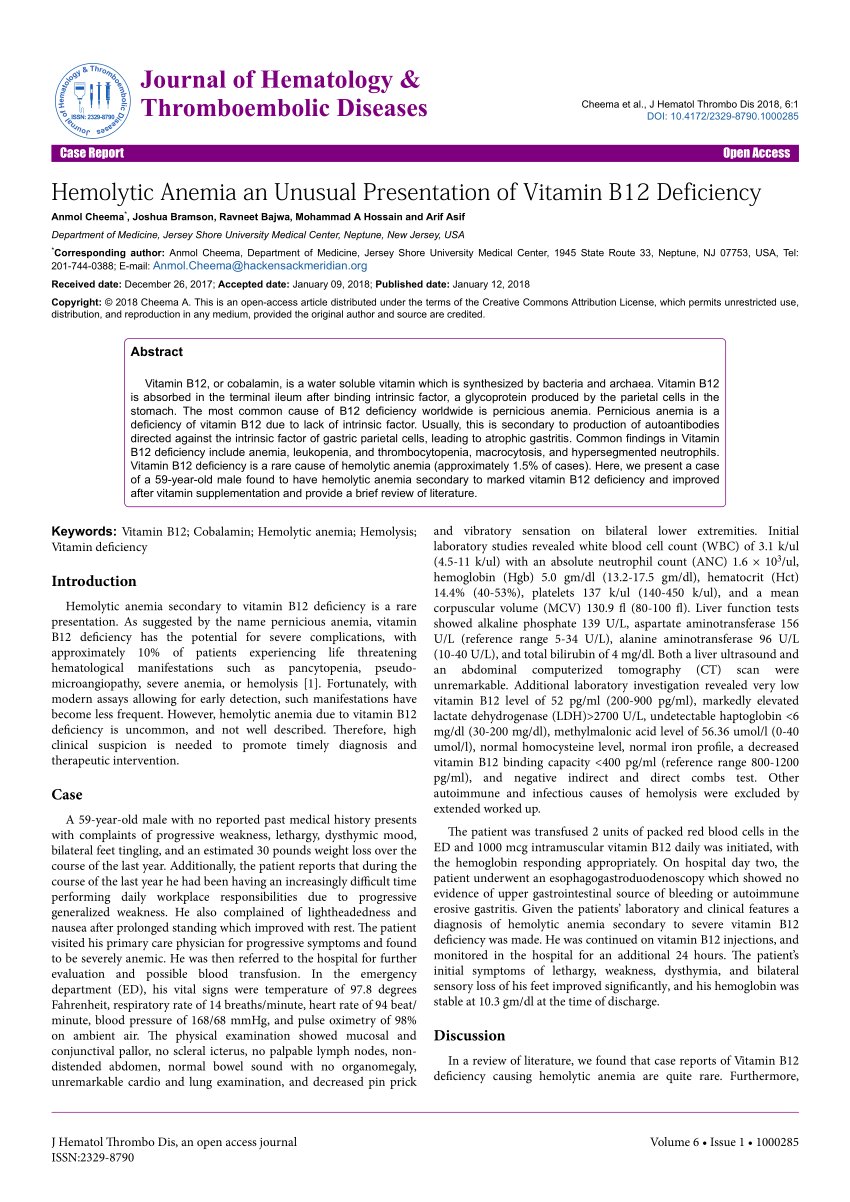
.jpg)






.jpg)
