Why Do Underserved Populations Have Trouble Sticking To Treatment Plans
In the heart of bustling cities and remote rural communities, a silent crisis unfolds daily: the struggle of underserved populations to adhere to prescribed medical treatment plans. This isn't merely a matter of individual willpower; it's a complex web of socio-economic barriers, systemic inequities, and deep-seated mistrust that undermines health outcomes and perpetuates cycles of disadvantage.
This article delves into the multifaceted reasons why underserved communities face significant challenges in sticking to treatment regimens. It will explore the socioeconomic factors, systemic issues, and cultural considerations that contribute to this pervasive problem, drawing upon expert opinions and data from reputable organizations to paint a comprehensive picture.
Socioeconomic Barriers: The Weight of Daily Life
Poverty is a primary driver of non-adherence. Individuals struggling to afford basic necessities often prioritize food and shelter over medication.
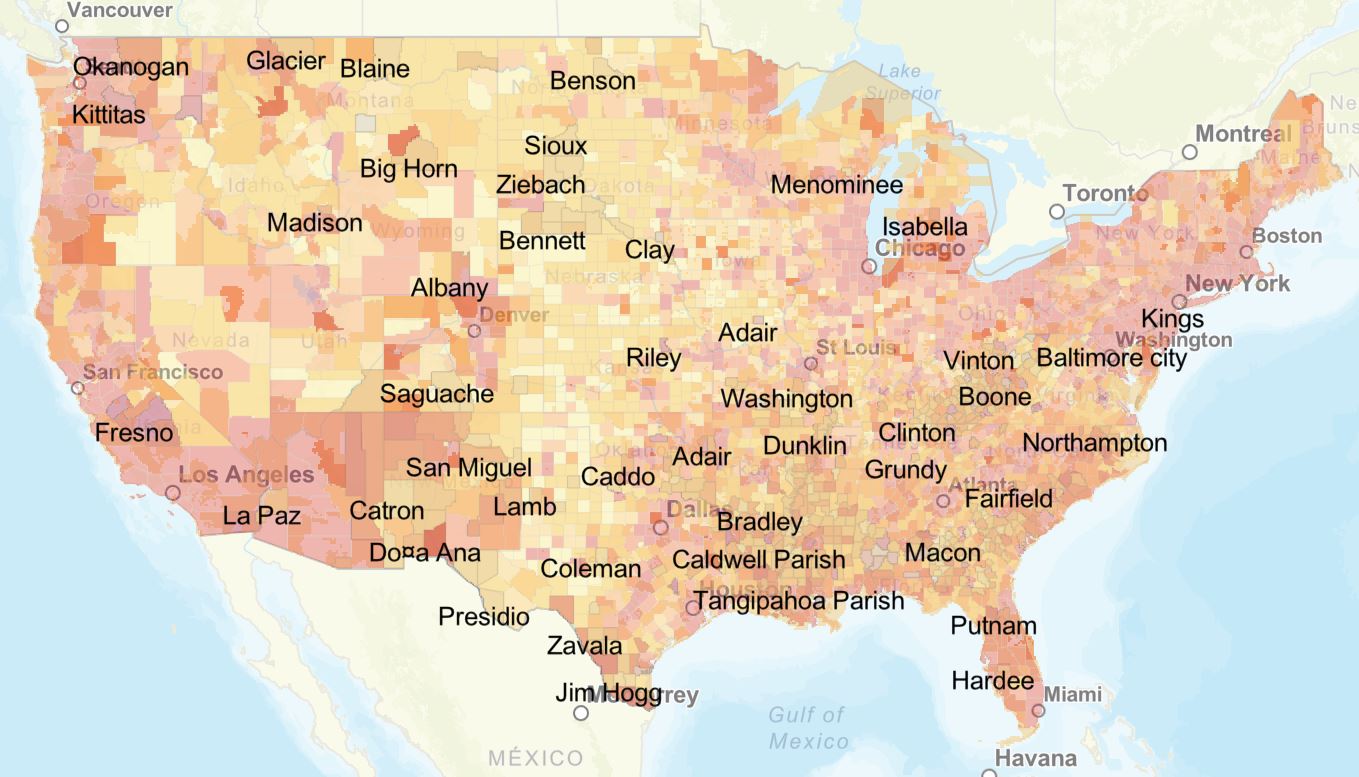
Transportation costs can also be prohibitive, especially for those living in areas with limited public transit or reliable vehicles, as highlighted in a 2023 report by the Centers for Disease Control and Prevention (CDC).
The lack of affordable housing and the stress associated with unstable living situations further complicate adherence.
Food Insecurity and Medication Adherence
Food insecurity creates a difficult choice: medication or nourishment. Some medications require taking with food, further straining resources.
Malnutrition can also affect the body's ability to absorb and utilize medications effectively, compounding the problem. According to the USDA, food deserts disproportionately affect low-income communities.
The Burden of Employment
Many underserved individuals work multiple jobs or hold positions with inflexible hours. This makes it difficult to attend medical appointments or take medication as prescribed.
The lack of paid sick leave can also force individuals to choose between their health and their livelihood. Lost wages associated with medical visits add to the financial burden.
Systemic Inequities: Navigating a Broken System
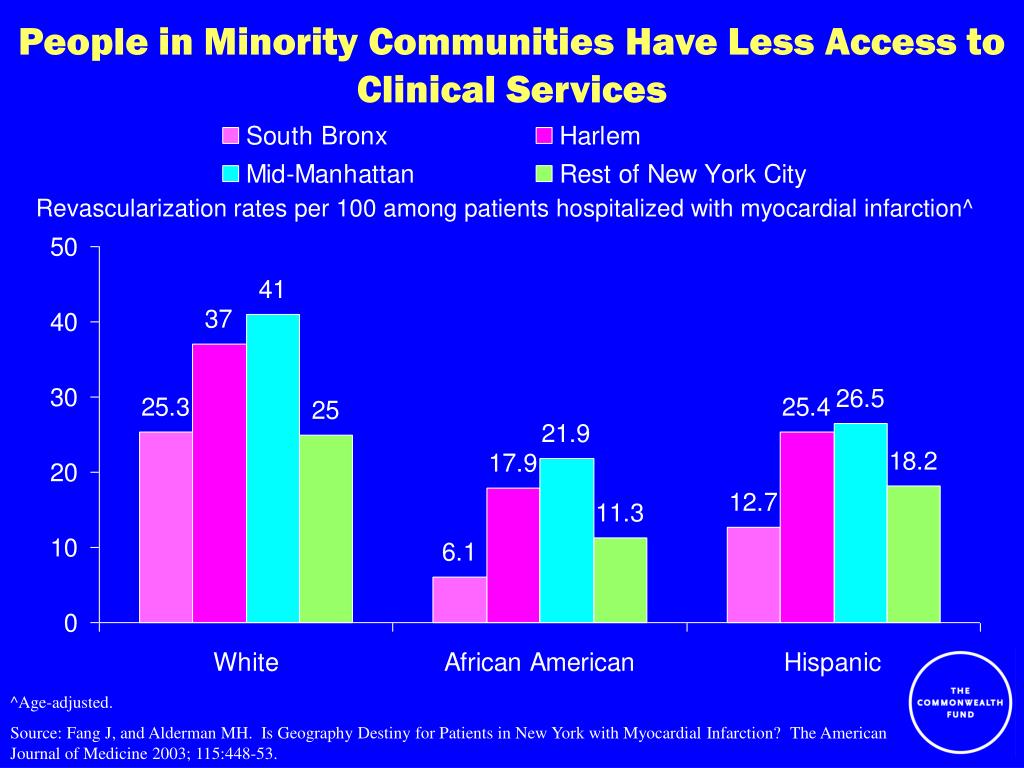
The healthcare system itself often presents barriers to adherence. Limited access to quality healthcare, long wait times, and understaffed clinics disproportionately impact underserved communities.
Furthermore, a lack of cultural competency among healthcare providers can create mistrust and communication barriers, making it difficult for patients to understand and follow treatment plans, says Dr. Maria Rodriguez, a public health expert at Johns Hopkins University.
Language barriers exacerbate these issues. A 2022 study published in the American Journal of Public Health found that patients with limited English proficiency were significantly less likely to adhere to medication regimens.
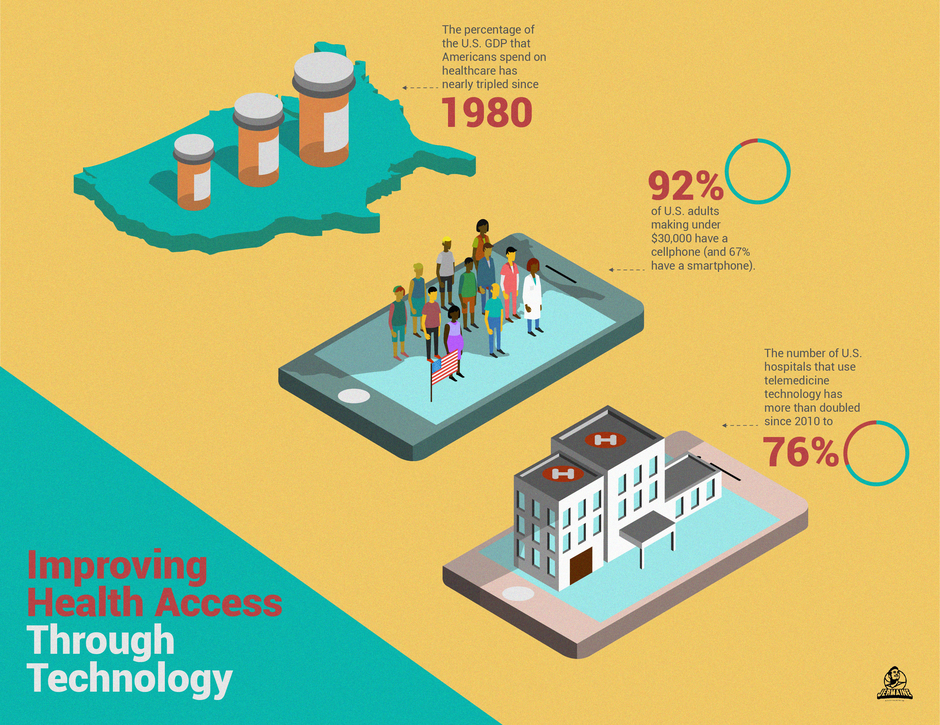
The Digital Divide
The increasing reliance on telehealth and online patient portals can exclude those without access to reliable internet or digital literacy skills. This creates a "digital divide" that further marginalizes underserved populations.
Many patients rely on paper instructions and in-person consultations, both of which can be less accessible. The shift towards digital health tools unintentionally widens existing health disparities.
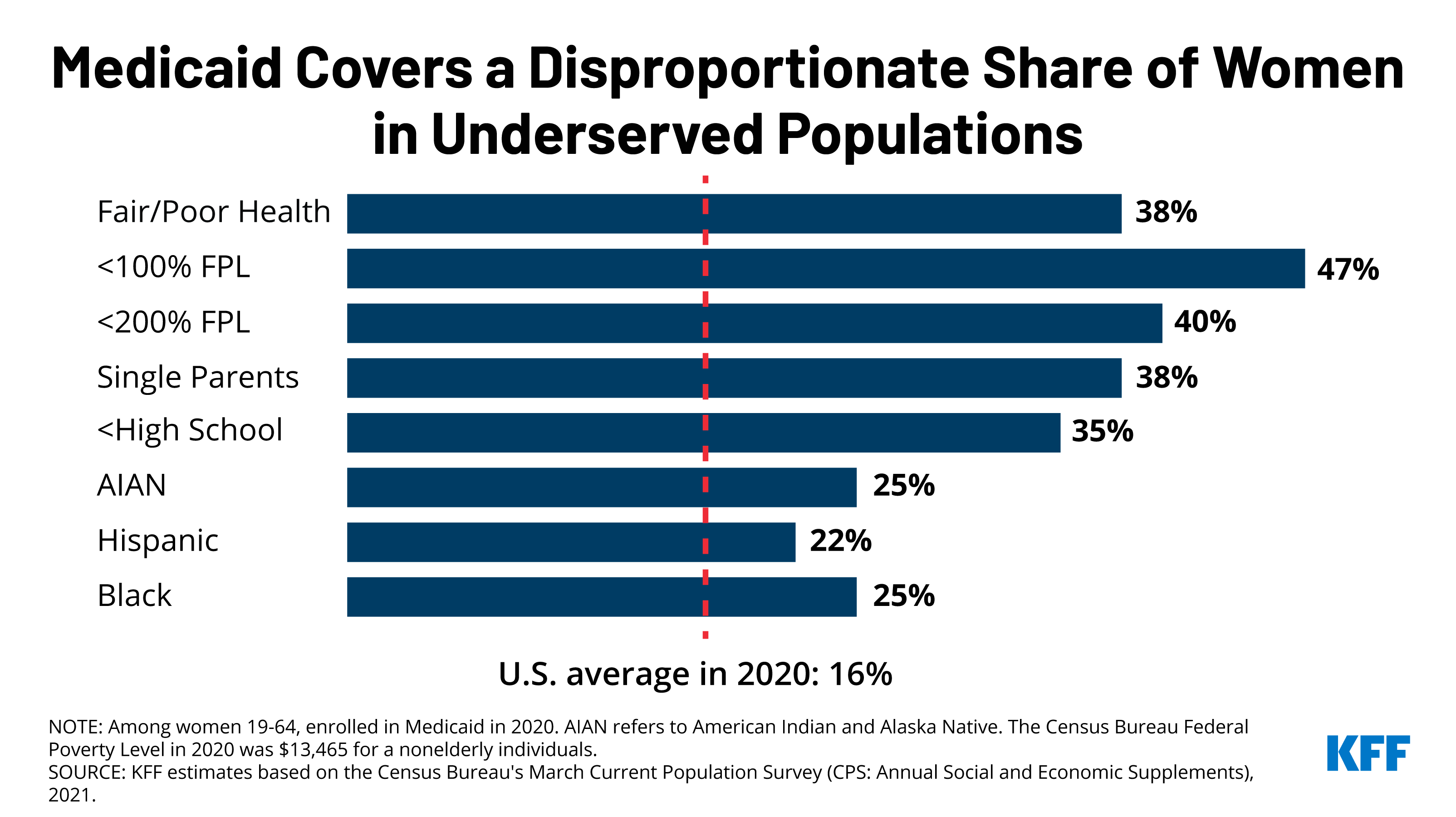
Insurance Coverage and Access
Gaps in insurance coverage, high deductibles, and co-pays can make healthcare unaffordable. Even with insurance, many medications are simply too expensive for low-income individuals.
"The complexities of navigating the insurance system can be overwhelming, especially for those with limited education or language proficiency," explains Dr. David Williams, a health policy analyst at the Kaiser Family Foundation.
Cultural and Psychological Factors: Beyond the Surface
Cultural beliefs and practices can also influence adherence. Some communities may have traditional healing practices that conflict with conventional medicine, leading to hesitancy in following prescribed treatments.
Mistrust of the medical establishment, rooted in historical injustices and experiences of discrimination, can create significant barriers. The Tuskegee Syphilis Study, for example, continues to cast a long shadow on trust within the African American community.
Mental health challenges, such as depression and anxiety, are often more prevalent in underserved populations and can significantly impact adherence. These conditions can impair a person's ability to remember appointments, manage medications, and engage in self-care.
Health Literacy and Communication
Low health literacy, the ability to understand and act on health information, is a major obstacle. Patients may struggle to comprehend complex medical instructions or ask clarifying questions.
Effective communication between healthcare providers and patients is crucial. This involves using plain language, tailoring information to individual needs, and actively listening to patient concerns.
Social Support and Community Resources
A lack of social support can make it difficult to adhere to treatment plans. Strong social networks provide encouragement, reminders, and practical assistance.
Community-based organizations and peer support groups can play a vital role in promoting adherence by providing education, resources, and a sense of belonging. The Robert Wood Johnson Foundation has funded numerous initiatives aimed at strengthening community health infrastructure.
Moving Forward: A Path Towards Equitable Adherence
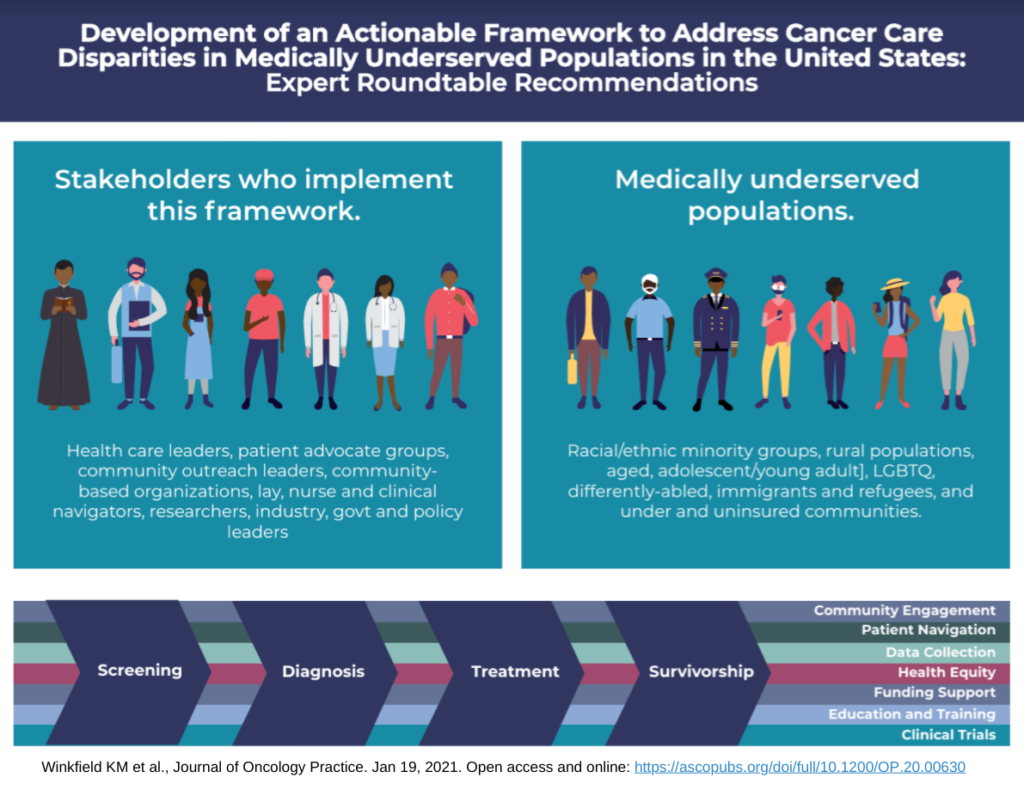
Addressing the challenges of treatment adherence in underserved populations requires a multi-pronged approach. This includes advocating for policies that expand access to affordable healthcare, addressing social determinants of health, and promoting culturally competent care.
Telehealth can offer solutions, but must be implemented thoughtfully to ensure equitable access. Increased funding for community-based health programs and culturally sensitive outreach initiatives are also essential.
By recognizing the complex interplay of socioeconomic, systemic, and cultural factors that influence adherence, we can create a more equitable and effective healthcare system for all. Only then can we truly bridge the gap in health outcomes and empower underserved communities to lead healthier lives.