At What Flow Rate Should Supplemental Oxygen Be Delivered
Imagine a gentle breeze, barely perceptible, yet vital for the blossoming of a fragile flower. Similarly, in the realm of medicine, the correct flow rate of supplemental oxygen can be the subtle difference between a patient struggling for breath and breathing with ease, each breath a gentle reminder of life's inherent rhythm. It's a delicate balance, a carefully calibrated dance between need and delivery, where precision truly matters.
Determining the optimal flow rate for supplemental oxygen delivery is a critical aspect of respiratory care, influencing patient outcomes and comfort significantly. It requires a nuanced understanding of individual patient needs, underlying medical conditions, and available oxygen delivery devices. This article delves into the intricacies of this vital medical practice, exploring the factors that contribute to determining the appropriate oxygen flow rate and the importance of individualized treatment plans.
The Foundation: Why Oxygen Matters
Oxygen is the lifeblood of our cells, the essential ingredient for cellular respiration, the process that fuels our bodies. When illness or injury impairs the body's ability to absorb or transport oxygen efficiently, supplemental oxygen becomes a crucial intervention. This additional oxygen helps ensure tissues and organs receive the oxygen they need to function properly, preventing potentially life-threatening complications.
Conditions like pneumonia, chronic obstructive pulmonary disease (COPD), asthma exacerbations, and heart failure often necessitate supplemental oxygen. Understanding the specific pathology behind these conditions is key to tailoring oxygen therapy effectively.
Assessing the Need: Signs of Oxygen Deficiency
Recognizing the signs of hypoxia, or low blood oxygen levels, is the first step in initiating appropriate oxygen therapy. These signs can manifest in various ways, ranging from subtle to severe.
Common indicators include shortness of breath, rapid breathing, increased heart rate, confusion, and cyanosis (a bluish discoloration of the skin, particularly around the lips and fingertips). Using a pulse oximeter to measure oxygen saturation (SpO2) is a non-invasive way to assess oxygen levels in the blood, providing valuable data for clinical decision-making.
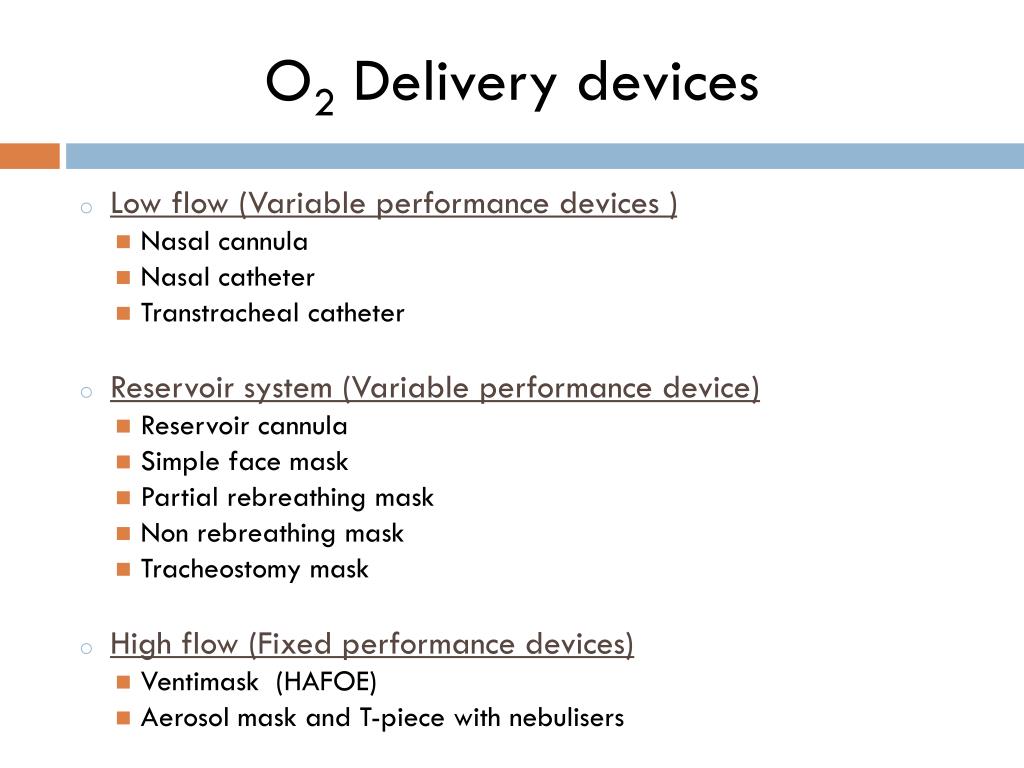
Delivery Methods: A Range of Options
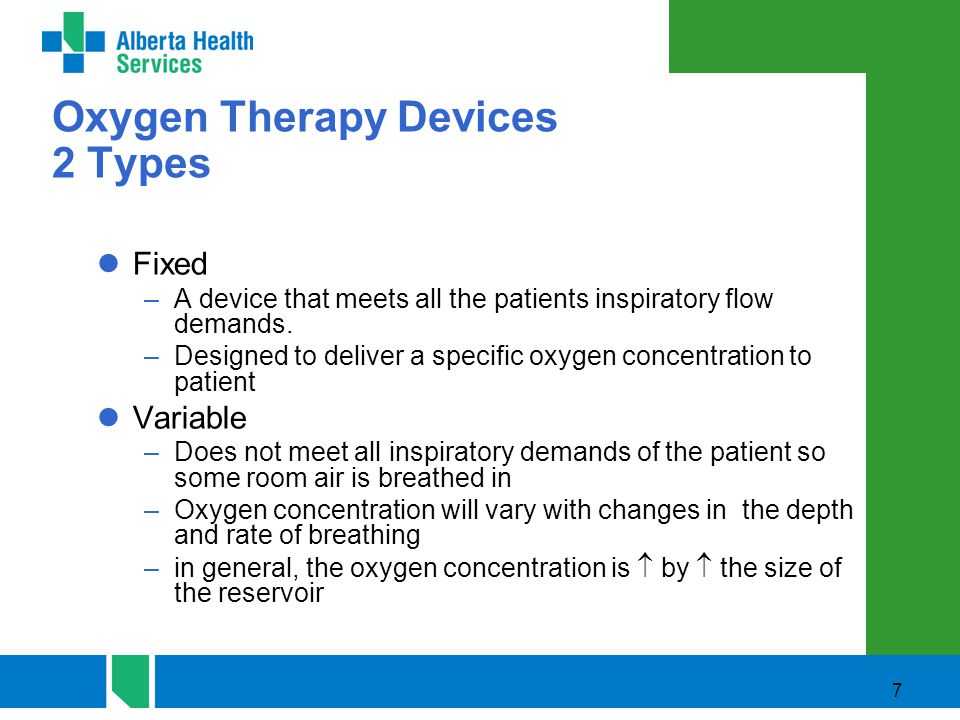
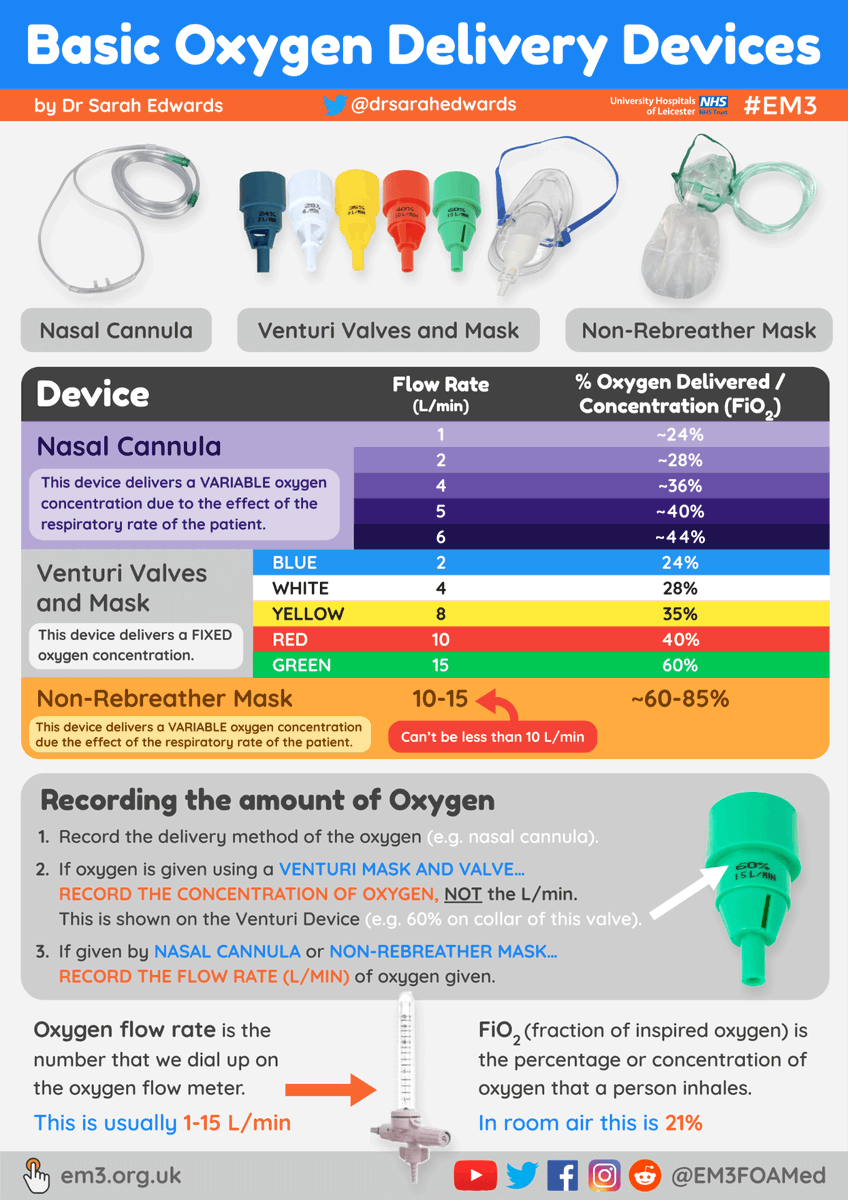
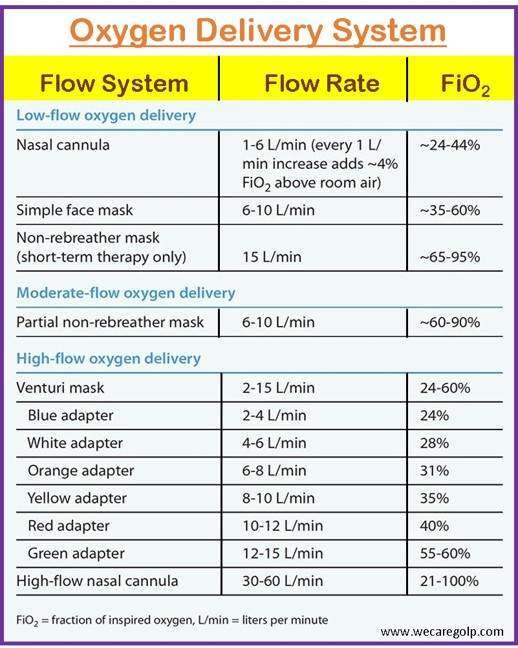
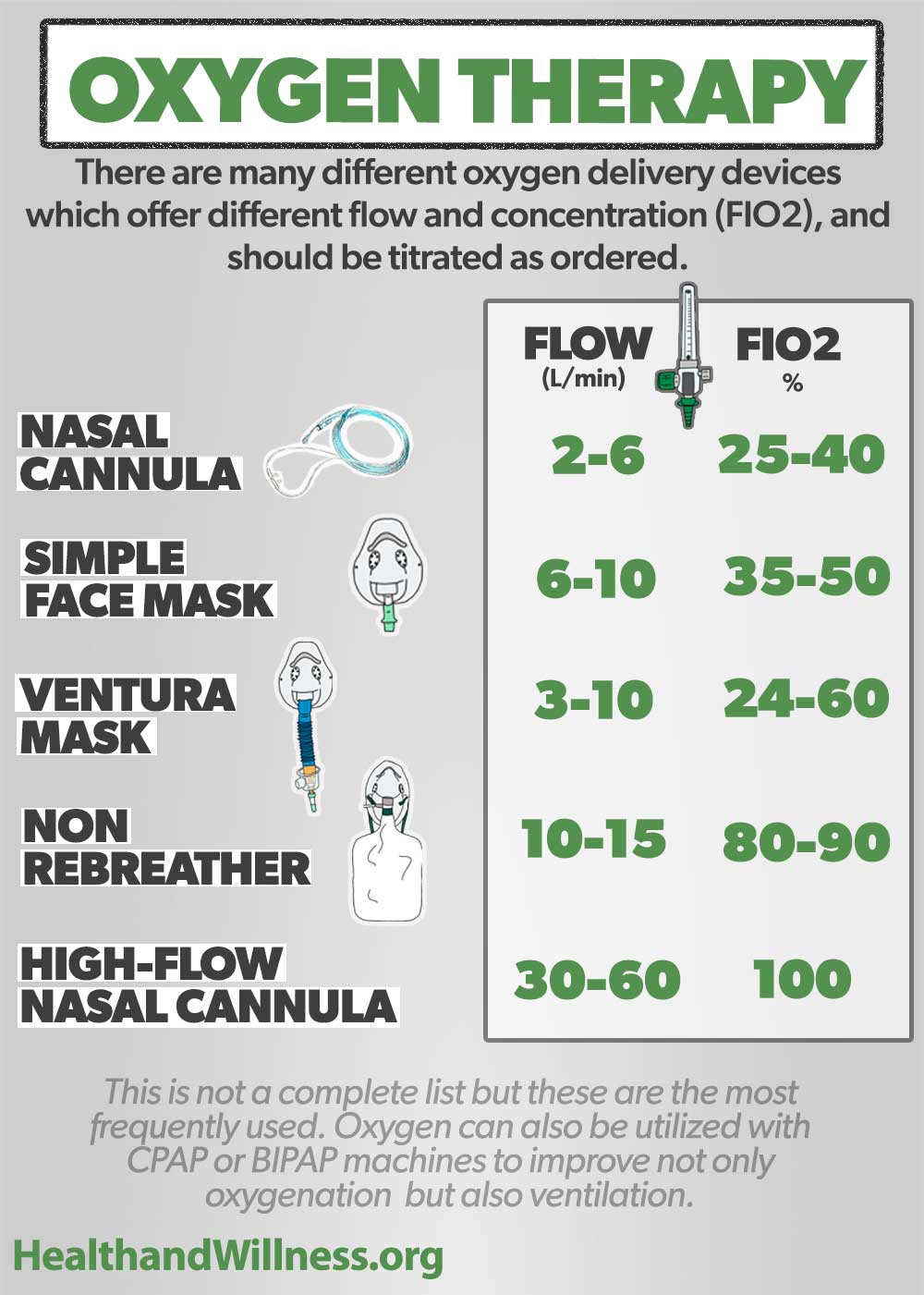
The method of oxygen delivery plays a significant role in determining the achievable flow rate and the concentration of oxygen delivered. Different devices are suited for various patient needs and clinical settings.
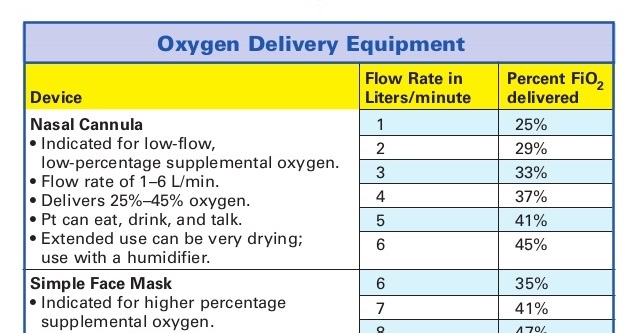
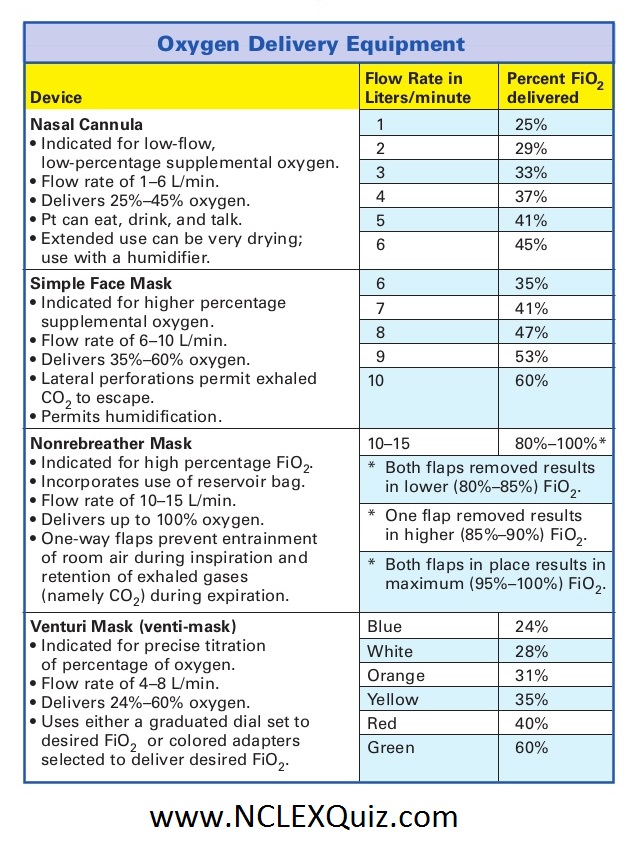
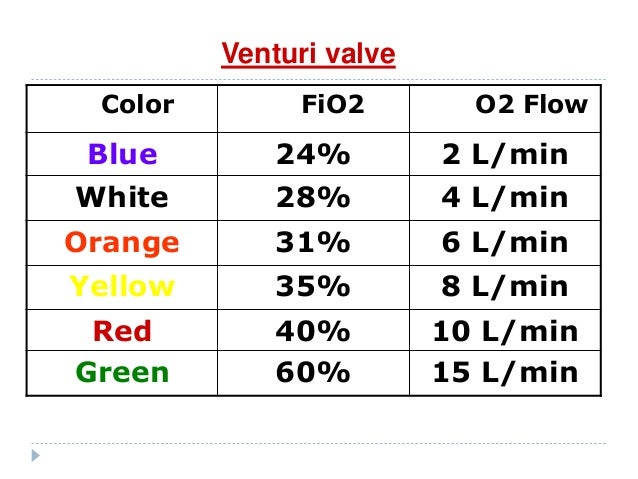
Nasal cannulas are a common and well-tolerated option for delivering low-flow oxygen, typically up to 6 liters per minute (LPM). Face masks, including simple masks and non-rebreather masks, can deliver higher concentrations of oxygen. Venturi masks offer a precise and controlled oxygen concentration, making them particularly useful for patients with COPD, where high oxygen levels can suppress the drive to breathe.
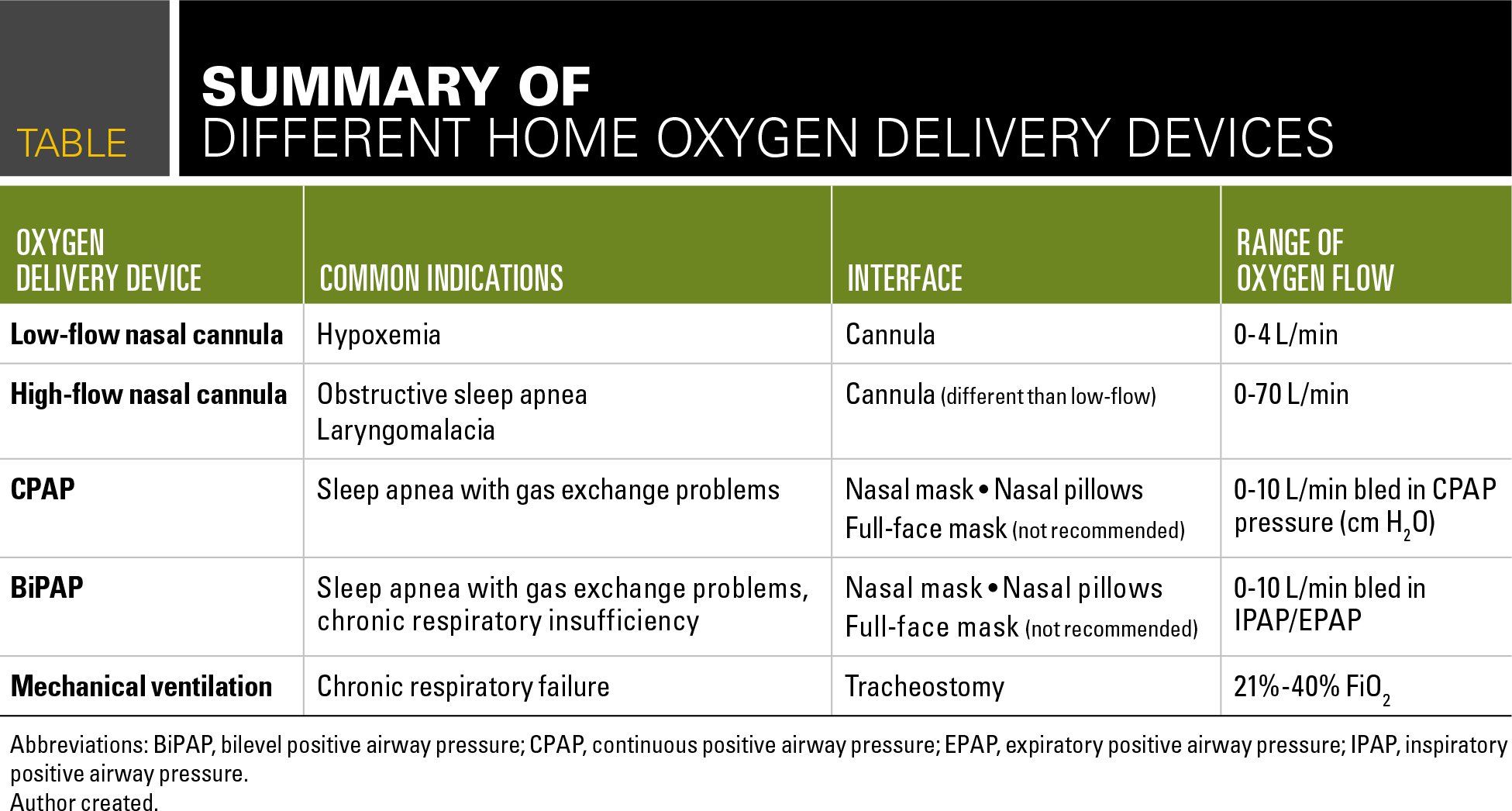
In critical situations, or when patients cannot breathe independently, more invasive methods like mechanical ventilation may be necessary. These methods require intubation and careful monitoring of respiratory parameters.
Flow Rate Guidelines: General Principles
While there is no one-size-fits-all answer to the optimal oxygen flow rate, some general guidelines provide a starting point. Most protocols aim to achieve an SpO2 between 94% and 98% in most patients.
However, this target range may differ for individuals with specific conditions, such as COPD, where a lower SpO2 target of 88% to 92% is often preferred to avoid suppressing the hypoxic drive. Starting with a low flow rate and gradually increasing it while monitoring the patient's response is generally recommended.
Regularly assessing the patient's oxygen saturation, respiratory rate, and work of breathing is crucial to adjust the flow rate as needed.
Individualized Care: Tailoring Oxygen Therapy
The most crucial aspect of determining the appropriate oxygen flow rate is individualizing the treatment plan. Factors like the patient's age, underlying medical conditions, severity of respiratory distress, and response to therapy must be considered.
For example, a young, healthy individual experiencing an asthma exacerbation might require a higher flow rate initially to quickly improve oxygenation, while an elderly patient with COPD may need a lower, more carefully titrated flow rate to avoid complications. Consulting with a respiratory therapist or physician is essential to develop and implement a personalized oxygen therapy plan.
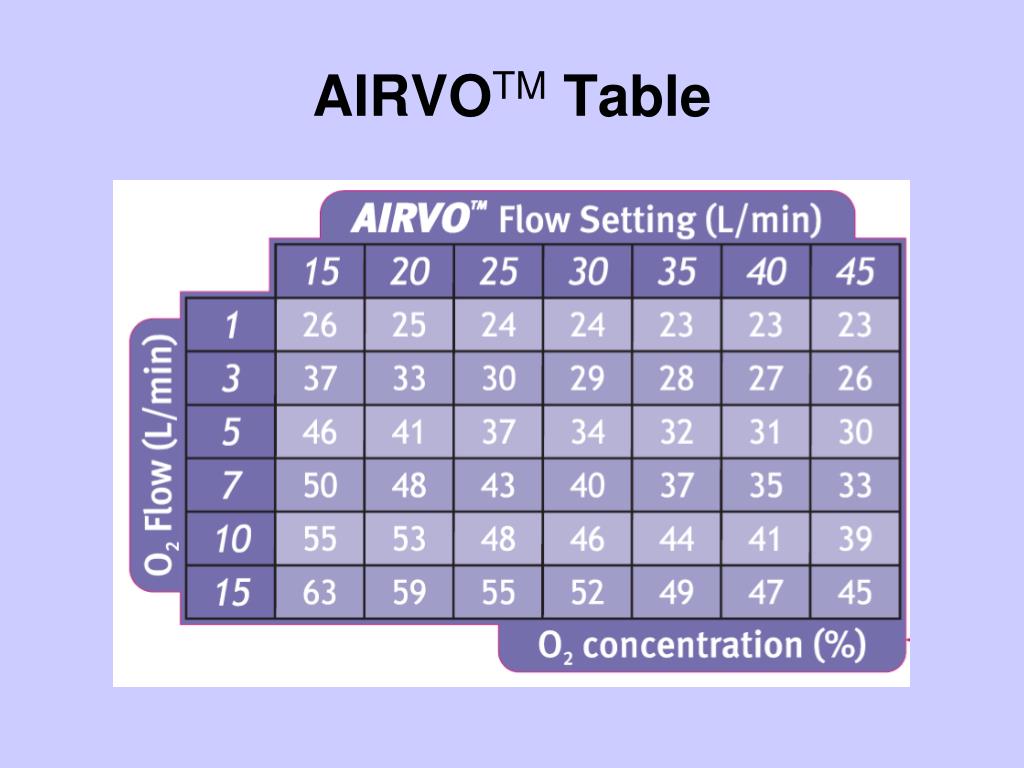
Furthermore, consider the role of humidity when administering oxygen. High flow rates of dry oxygen can dry out the nasal passages, leading to discomfort and potentially increasing the risk of nosebleeds. Adding humidification to the oxygen source can alleviate this issue and improve patient comfort.
COPD Considerations: A Delicate Balance
Patients with COPD often have chronically elevated carbon dioxide levels in their blood. Administering high concentrations of oxygen can suppress their hypoxic drive, the mechanism that stimulates them to breathe.
Therefore, healthcare providers must carefully titrate oxygen flow rates in COPD patients, aiming for a lower SpO2 target and closely monitoring their respiratory rate and level of consciousness. Using Venturi masks to deliver precise oxygen concentrations is particularly beneficial in these cases.
Close monitoring and frequent reassessment are vital to ensure the patient receives the appropriate amount of oxygen without compromising their respiratory drive.
The Role of Technology: Monitoring and Adjustment
Advancements in medical technology have significantly improved the precision and effectiveness of oxygen therapy. Pulse oximeters provide continuous, non-invasive monitoring of oxygen saturation, allowing healthcare providers to quickly detect changes in oxygenation and adjust the flow rate accordingly.
Some sophisticated oxygen delivery systems can automatically adjust the flow rate based on the patient's breathing pattern and oxygen saturation levels. These systems can help maintain optimal oxygenation while minimizing the risk of over- or under-oxygenation.
Blood gas analysis offers a more comprehensive assessment of oxygenation, carbon dioxide levels, and acid-base balance, providing valuable information for complex cases.
Educating Patients: Empowering Self-Management
Patient education is an integral part of successful oxygen therapy. Empowering patients and their caregivers with knowledge about their condition, oxygen delivery device, and potential complications can improve adherence to therapy and enhance their overall quality of life.
Patients should be instructed on how to properly use and maintain their oxygen equipment, recognize signs of hypoxia or hyperoxia (excessively high oxygen levels), and know when to seek medical attention. Providing clear and concise instructions, along with opportunities for questions and demonstrations, can significantly improve patient outcomes.
The ability to self-manage their oxygen therapy empowers patients to take an active role in their health and well-being.
Looking Ahead: Innovations in Oxygen Delivery
The field of oxygen therapy is continuously evolving, with ongoing research and development focused on improving delivery methods, monitoring technologies, and patient outcomes. Portable oxygen concentrators have revolutionized the lives of many patients requiring long-term oxygen therapy, providing greater freedom and mobility.
Researchers are also exploring novel oxygen delivery techniques, such as transcutaneous oxygen sensors and personalized oxygen titration algorithms, to further optimize oxygen therapy. Telemedicine and remote monitoring technologies are also playing an increasingly important role in managing patients on oxygen therapy at home.
These innovations promise to further enhance the effectiveness and convenience of oxygen therapy, improving the lives of countless individuals worldwide.
Determining the appropriate flow rate for supplemental oxygen is a dynamic process, requiring a blend of scientific knowledge, clinical judgment, and individualized patient assessment. It's about more than just numbers; it's about understanding the unique needs of each person and carefully calibrating the delivery to support their body's innate ability to heal and thrive. The gentle breeze of precisely delivered oxygen can indeed make all the difference, allowing individuals to breathe easier, live fuller lives, and find comfort in the rhythm of their own breath.