Best Probiotic To Prevent C Diff
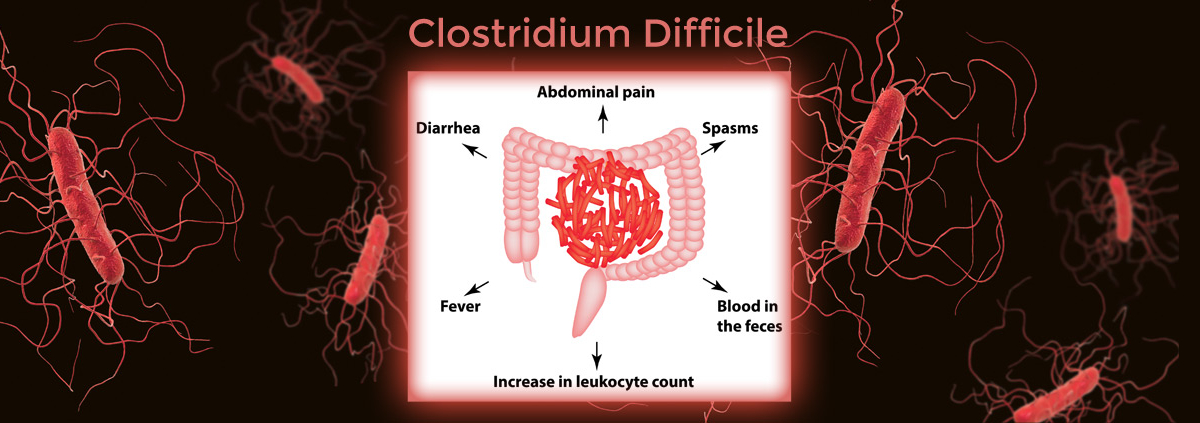
The specter of Clostridioides difficile (C. diff) infection looms large in healthcare settings, a formidable foe that can transform routine antibiotic treatment into a debilitating and potentially deadly ordeal. This bacterium, notorious for its antibiotic resistance, exploits weakened gut microbiomes to unleash a cascade of symptoms, from relentless diarrhea to life-threatening colitis. The quest for effective preventative measures has become increasingly urgent, with researchers focusing intensely on the potential of probiotics to fortify the gut and ward off C. diff's insidious advance.
This article delves into the burgeoning field of probiotic research concerning C. diff prevention. It examines the scientific evidence surrounding various probiotic strains and their efficacy in mitigating the risk of infection. By analyzing clinical trials and expert opinions, we aim to provide a balanced perspective on the current state of knowledge, highlighting both the promise and the limitations of using probiotics as a preventative strategy against this persistent healthcare challenge.
The C. diff Threat: A Primer
C. diff infection (CDI) primarily affects individuals who have recently taken antibiotics. Antibiotics, while crucial for fighting bacterial infections, can disrupt the delicate balance of the gut microbiome. This disruption creates an opportunity for C. diff to flourish, releasing toxins that damage the colon lining.
Symptoms of CDI can range from mild diarrhea to severe abdominal pain, fever, and toxic megacolon. In severe cases, CDI can lead to sepsis, organ failure, and even death. Hospitalized patients, the elderly, and those with weakened immune systems are particularly vulnerable.
Probiotics: A Potential Shield Against C. diff
Probiotics, often referred to as "good bacteria," are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. They are believed to work by restoring balance to the gut microbiome, competing with harmful bacteria like C. diff for resources, and producing substances that inhibit their growth. The allure of probiotics lies in their potential to bolster the gut's natural defenses, preventing C. diff from gaining a foothold.
The mechanism behind probiotic action against C. diff is complex. It involves competition for nutrients, production of antimicrobial substances, and modulation of the immune response. Some probiotic strains can even neutralize C. diff toxins directly.
Key Probiotic Strains Under Investigation
Several probiotic strains have emerged as promising candidates for C. diff prevention. Among them, Saccharomyces boulardii and certain strains of Lactobacillus stand out due to the strength of evidence supporting their use.
Saccharomyces boulardii: A Fungal Ally
S. boulardii is a non-pathogenic yeast that has shown efficacy in preventing antibiotic-associated diarrhea, including CDI. Clinical trials have demonstrated that S. boulardii can significantly reduce the risk of CDI in patients taking antibiotics. Its mechanism of action is thought to involve neutralizing C. diff toxins and modulating the host's immune response.
A 2023 meta-analysis published in The Lancet Infectious Diseases, reviewed multiple clinical trials and found that S. boulardii was associated with a statistically significant reduction in the incidence of CDI. The study emphasized the need for further research to determine optimal dosages and duration of treatment.
Lactobacillus: A Diverse Group of Bacteria
The Lactobacillus genus encompasses a wide range of bacterial species, each with its unique properties. Some Lactobacillus strains, such as Lactobacillus rhamnosus GG and Lactobacillus casei, have shown promise in preventing CDI. Research suggests that these strains can help restore balance to the gut microbiome and inhibit the growth of C. diff.
A systematic review in the Journal of Clinical Gastroenterology highlighted that multi-strain probiotics containing Lactobacillus species may be more effective than single-strain probiotics. The synergy between different strains could enhance their ability to compete with C. diff and restore gut health.
Challenges and Considerations
While the evidence supporting the use of certain probiotics for C. diff prevention is encouraging, several challenges and considerations remain. The efficacy of probiotics can vary depending on the strain, dosage, and individual characteristics of the patient.
Not all probiotics are created equal. It is crucial to select products that have been rigorously tested and shown to be effective in clinical trials. Furthermore, the optimal timing of probiotic administration relative to antibiotic use is still under investigation.
Concerns about potential adverse effects of probiotics, although rare, also need to be addressed. In immunocompromised individuals, there is a theoretical risk of probiotic-associated infections.
Expert Perspectives and Guidelines
Medical organizations like the Centers for Disease Control and Prevention (CDC) acknowledge the potential role of probiotics in preventing antibiotic-associated diarrhea. However, they emphasize the need for more high-quality research to guide clinical practice.
The American Gastroenterological Association (AGA) provides guidelines on the management of CDI. Although they do not explicitly recommend the routine use of probiotics for prevention, they acknowledge that certain probiotics may be beneficial in select patient populations. These guidelines are frequently updated as new research emerges.
Dr. Emily Carter, a leading expert in infectious diseases at Mayo Clinic, emphasizes the importance of individualized approaches to CDI prevention. "Probiotics can be a valuable tool, but they are not a one-size-fits-all solution," she says. "Factors such as the patient's age, underlying health conditions, and the specific antibiotics they are taking need to be considered."
The Future of Probiotic Research for C. diff Prevention
Ongoing research is focused on identifying novel probiotic strains and optimizing their use for C. diff prevention. Studies are exploring the use of fecal microbiota transplantation (FMT) as a more aggressive approach to restoring gut health in patients at high risk of recurrent CDI.
Advances in microbiome sequencing technologies are providing a deeper understanding of the complex interactions within the gut. This knowledge is paving the way for personalized probiotic therapies tailored to an individual's unique microbiome profile.
Ultimately, a comprehensive approach to C. diff prevention is needed. This includes judicious use of antibiotics, meticulous hygiene practices, and, potentially, targeted use of probiotics. Continued research is essential to refine our understanding of the microbiome and harness its power to combat this persistent threat.














/medriva/media/post_banners/content/uploads/2024/01/c-diff-prevention-after-antibiotics-20240120011247.jpg)

