Blood Flow Is Blank According To Metabolic Needs
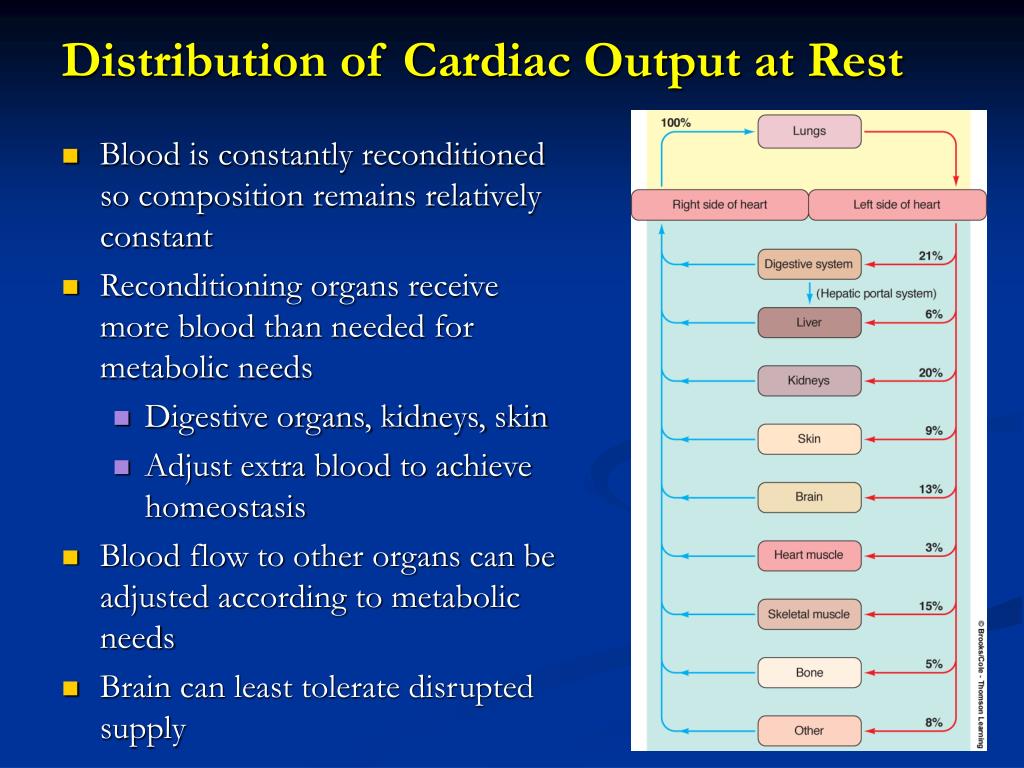
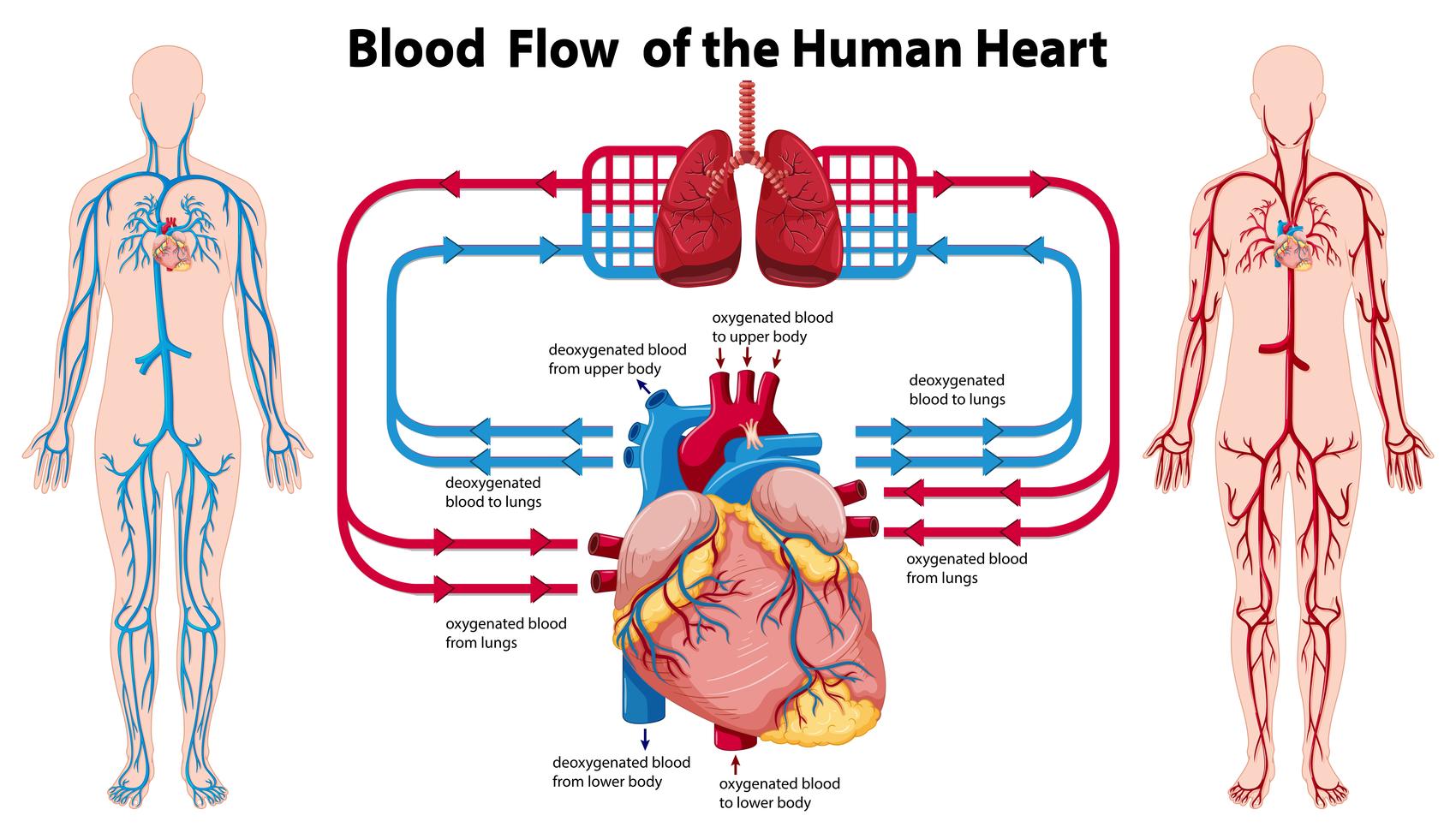
The human body, a marvel of biological engineering, orchestrates a complex symphony of processes every second. At the heart of this orchestra lies the circulatory system, constantly adjusting blood flow to meet the ever-changing metabolic demands of tissues and organs. New research is revealing the intricate mechanisms governing this dynamic regulation, challenging long-held assumptions and paving the way for innovative therapies.
This article delves into the emerging understanding of how blood flow is intrinsically linked to metabolic needs. We will explore the key players involved in this dynamic interplay, the latest scientific findings, and the potential implications for treating a range of diseases from cardiovascular disorders to cancer. Expert opinions and the latest data from reputable organizations will be presented to provide a comprehensive and balanced overview of this crucial area of biomedical research.
The Intricate Dance of Blood Flow and Metabolism
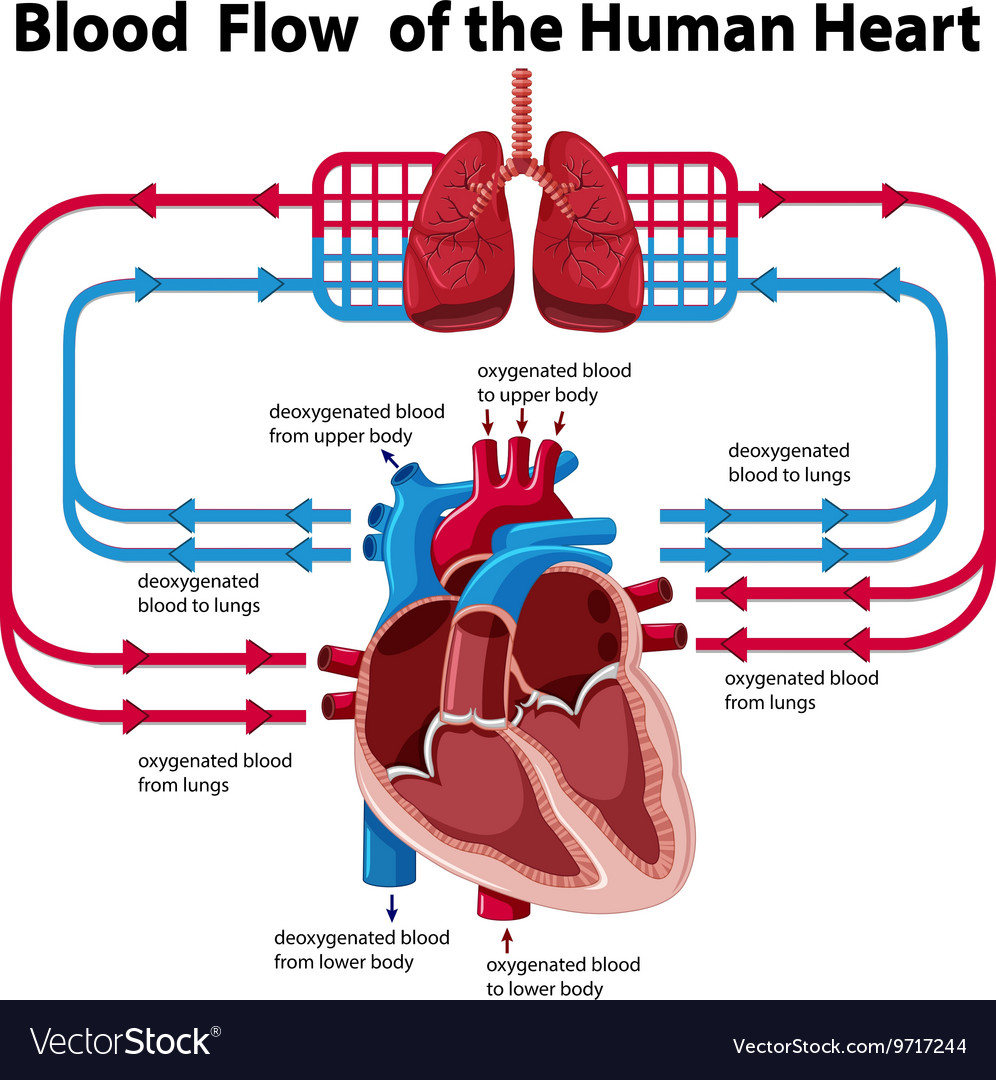
The body's metabolic rate, the rate at which it consumes energy, fluctuates dramatically based on activity levels, stress, and even the time of day. Blood flow, the delivery system for oxygen and nutrients, must precisely match these fluctuations to maintain cellular function. Failure to do so can lead to tissue damage, organ dysfunction, and ultimately, death.
The question is, how does the body achieve this remarkable feat of coordination?
Local Control Mechanisms
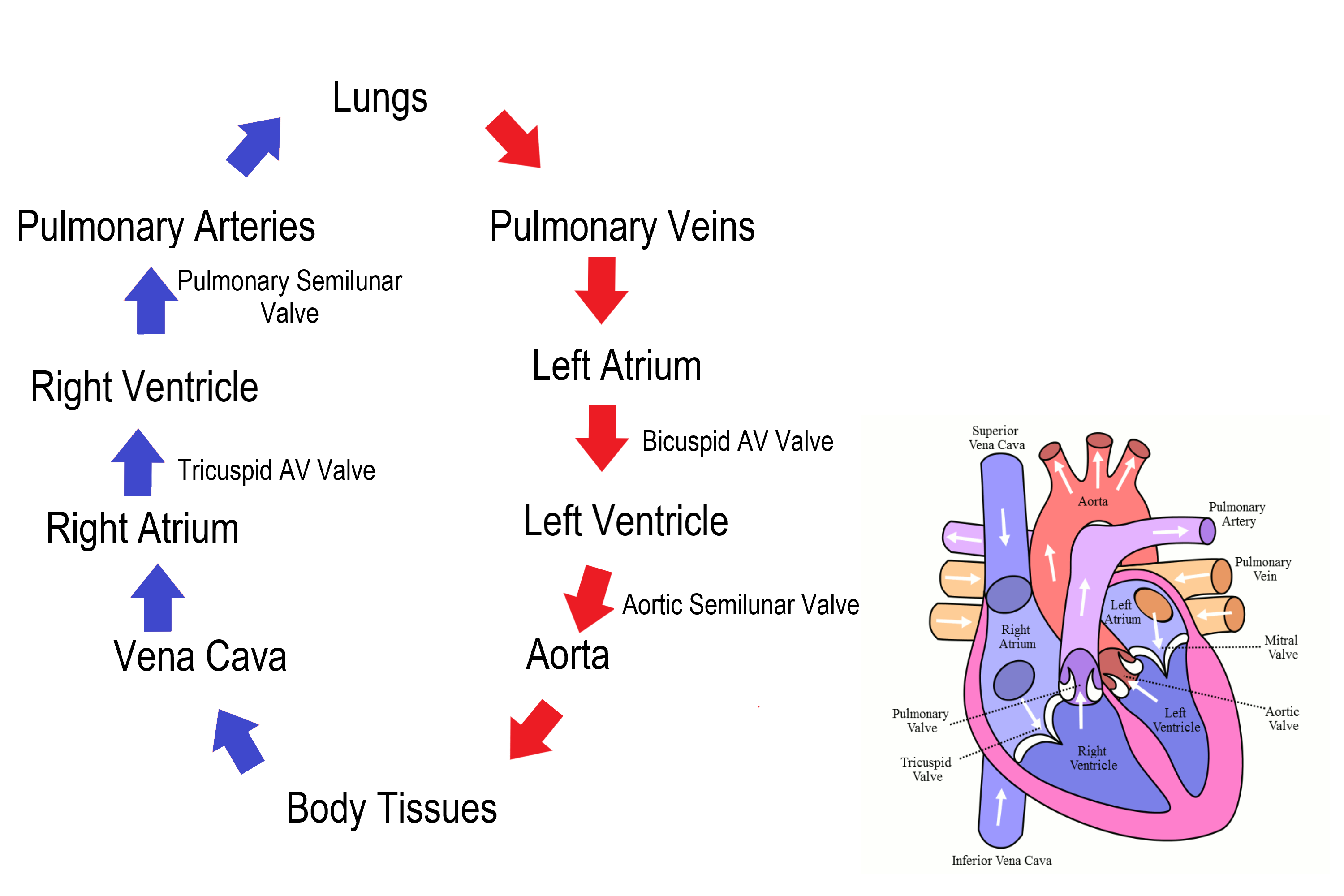
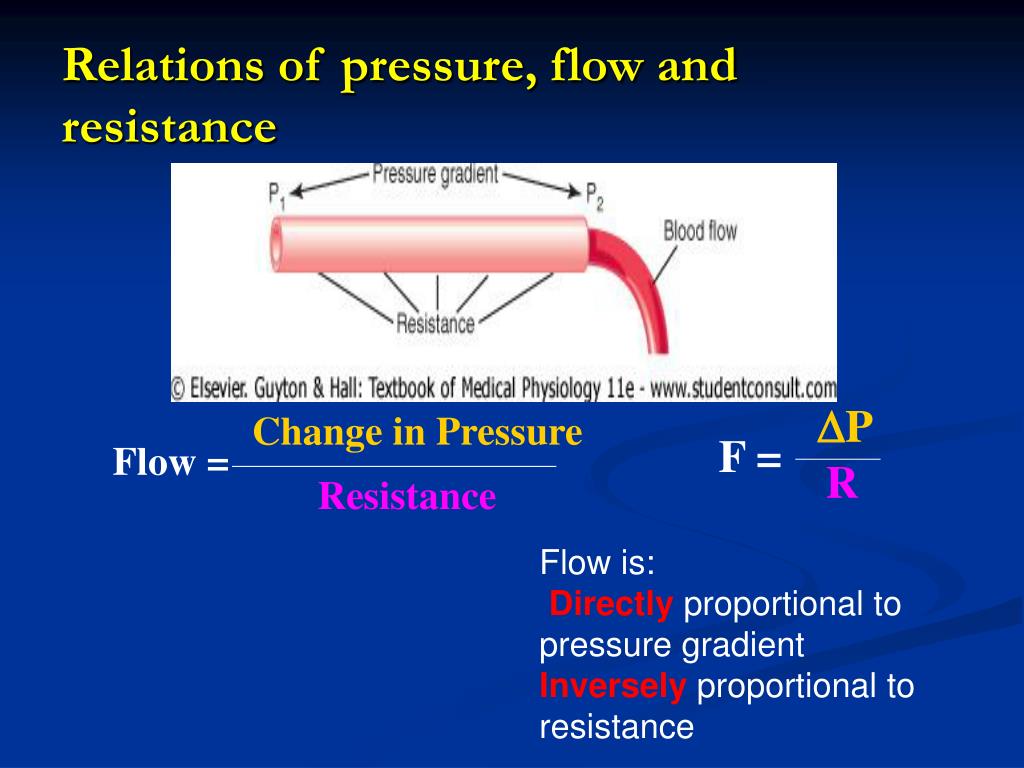
One of the primary mechanisms involves local control, where tissues themselves signal their needs directly to nearby blood vessels. This often involves the release of vasoactive substances, molecules that either constrict or dilate blood vessels.
For example, during exercise, muscle cells consume more oxygen and produce more carbon dioxide and adenosine. These byproducts trigger vasodilation, increasing blood flow to the active muscles.
According to a statement from the American Heart Association, “Understanding these local control mechanisms is vital for developing therapies that can improve blood flow to ischemic tissues."
The Role of the Endothelium
The endothelium, the inner lining of blood vessels, plays a critical role in regulating blood flow. It produces nitric oxide (NO), a potent vasodilator, in response to a variety of stimuli, including shear stress from blood flow itself.
Professor Emily Carter, a leading researcher in vascular biology at Stanford University, explains that, "The endothelium acts as a sensor, constantly monitoring the metabolic environment and adjusting blood vessel tone accordingly." This intricate feedback loop ensures that blood flow is finely tuned to meet the metabolic needs of surrounding tissues.
Endothelial dysfunction, characterized by impaired NO production, is a hallmark of many cardiovascular diseases, including hypertension and atherosclerosis.
Beyond Local Control: Systemic Regulation
While local control mechanisms are crucial, the body also employs systemic regulation to maintain blood pressure and blood flow throughout the entire circulatory system. This involves the autonomic nervous system and hormones.
The sympathetic nervous system, for instance, can constrict blood vessels in less active tissues to redirect blood flow to areas with higher metabolic demands. Hormones like epinephrine (adrenaline) can also have profound effects on blood flow, increasing heart rate and blood pressure during times of stress.
New Discoveries and Emerging Technologies
Recent advances in imaging technologies and molecular biology have shed new light on the complex interplay between blood flow and metabolism. Researchers are now able to visualize blood flow at the microvascular level and identify the specific molecules involved in regulating this process.
One promising area of research focuses on the role of metabolic sensors, proteins that directly detect changes in metabolic substrates like glucose and lactate. These sensors can then activate signaling pathways that modulate blood vessel tone and angiogenesis (the formation of new blood vessels).
Dr. David Miller at the National Institutes of Health stated, "Identifying these metabolic sensors and understanding how they function could lead to new therapies for diseases characterized by impaired blood flow, such as peripheral artery disease and diabetic ulcers."
Implications for Cancer Treatment
The link between blood flow and metabolism also has significant implications for cancer treatment. Cancer cells often have altered metabolic profiles, requiring more glucose and oxygen than normal cells.
Tumors also promote angiogenesis to ensure a constant supply of nutrients. Targeting tumor vasculature is a promising strategy for starving cancer cells and preventing their growth and spread.
Studies published in Nature Cancer have shown that drugs that disrupt tumor blood flow can significantly improve the efficacy of chemotherapy and radiation therapy.
Future Directions and Concluding Remarks
The field of blood flow regulation is rapidly evolving. Researchers are continuing to unravel the complex mechanisms that govern the dynamic interplay between blood flow and metabolism.
Future research will focus on identifying novel therapeutic targets for diseases characterized by impaired blood flow. This includes developing drugs that can enhance endothelial function, stimulate angiogenesis in ischemic tissues, and disrupt tumor vasculature.
Understanding how blood flow is intricately tailored to metabolic needs holds tremendous promise for improving human health. By continuing to explore this complex and fascinating area of biomedical research, scientists can pave the way for innovative therapies that will benefit millions of people worldwide.