Can An Ekg Detect Drug Use

In emergency rooms and clinical settings, the quest to swiftly and accurately diagnose a patient's condition is paramount. Amidst a growing opioid crisis and the prevalence of various substance abuse issues, the question arises: Can a seemingly routine electrocardiogram (EKG or ECG), primarily designed to assess heart function, also reveal evidence of drug use? The answer is complex and nuanced, sparking debate within the medical community and raising important considerations about diagnostic accuracy and patient privacy.
While an EKG is not a primary drug screening tool like a urine or blood test, it can detect abnormalities in heart rhythm and function that may be indicative of certain drug use. This article explores the extent to which an EKG can be used to identify drug-related effects, the limitations of this method, and the implications for both medical professionals and individuals seeking care. We will examine research findings, expert opinions, and potential ethical considerations surrounding the use of EKGs in detecting drug use.
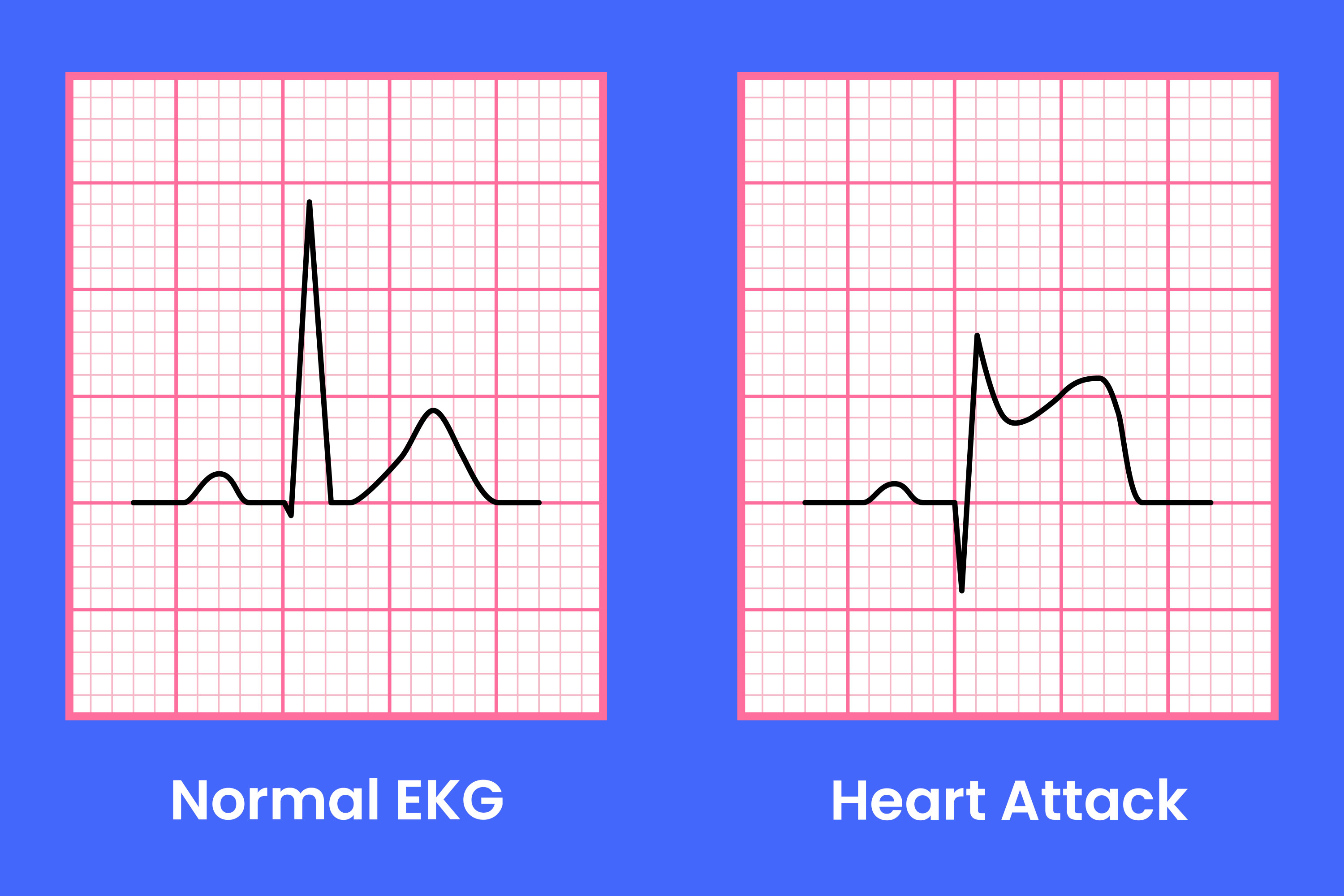
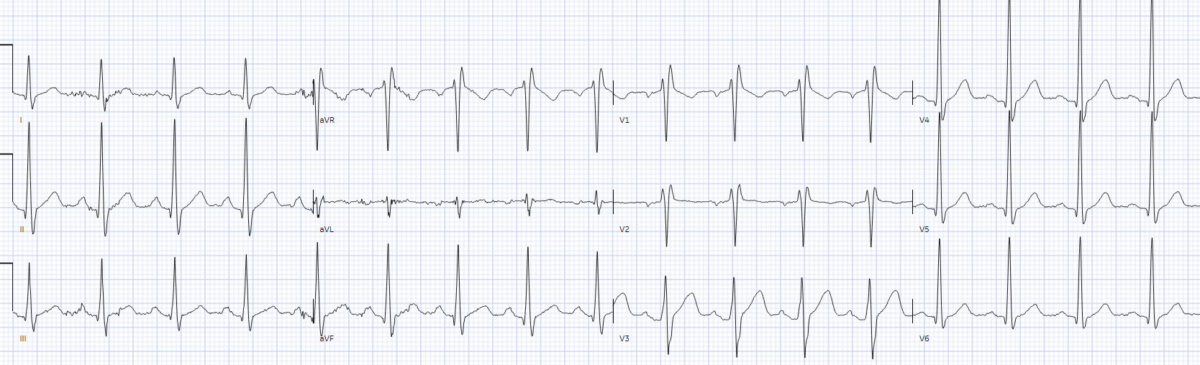
The Heart's Response: What an EKG Reveals
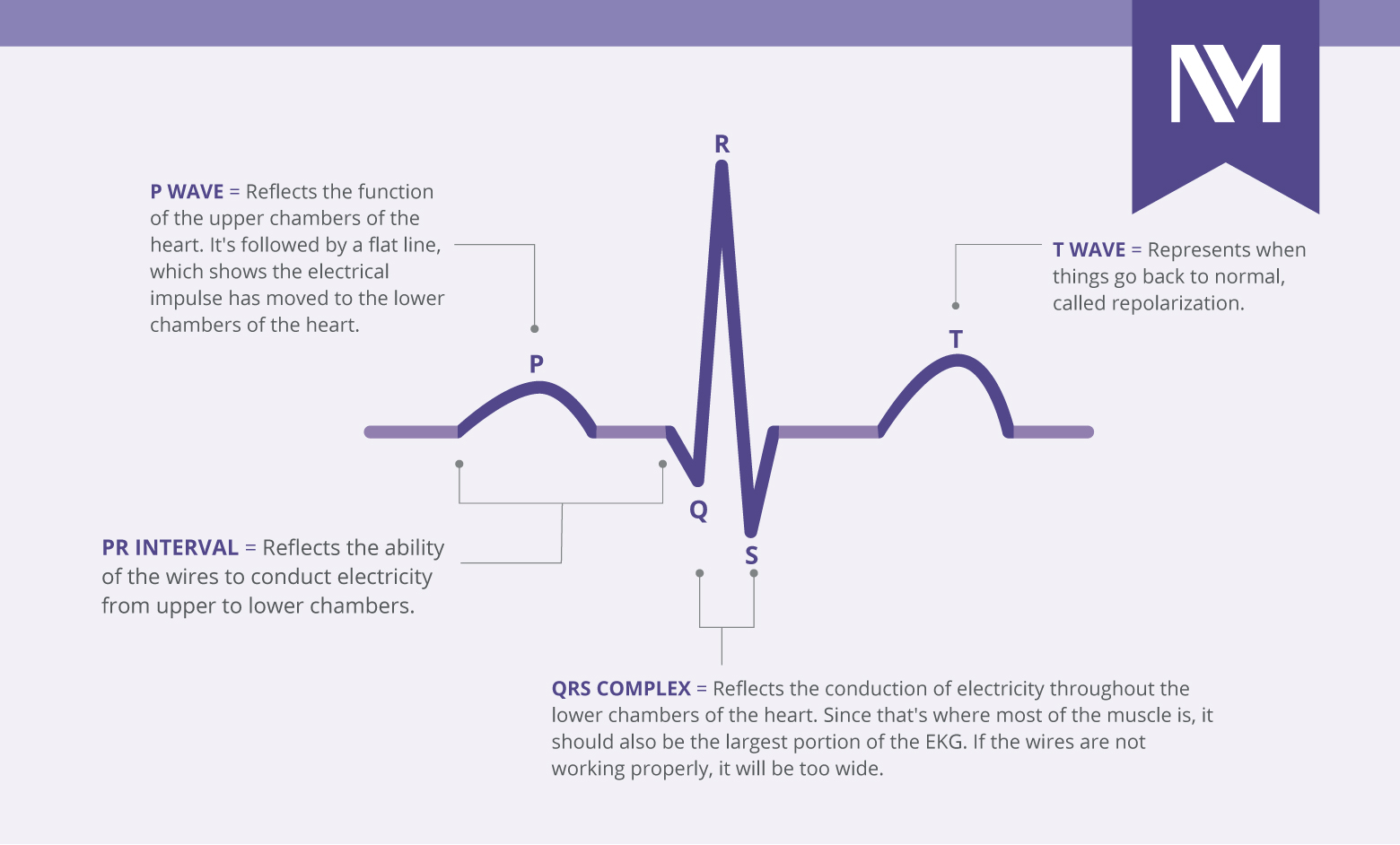
An EKG measures the electrical activity of the heart. This provides a visual representation of the heart's rhythm, rate, and any structural or functional abnormalities.
Certain drugs can significantly impact these electrical signals, leading to identifiable changes on an EKG.
These changes, however, are not always specific to drug use and can be caused by other medical conditions.
Specific Drugs and EKG Changes
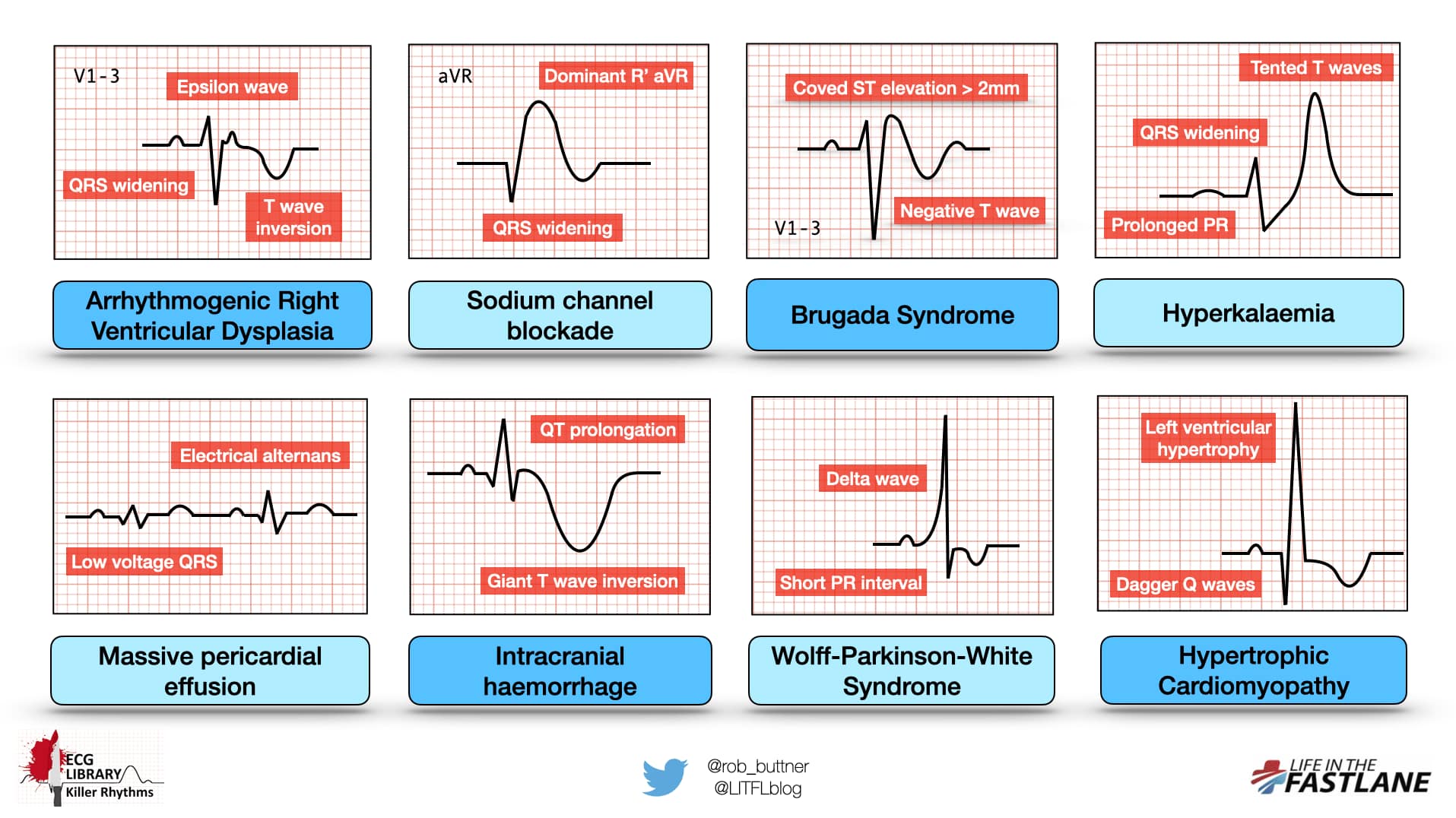
Several classes of drugs have been linked to characteristic EKG changes. Stimulants like cocaine and amphetamines can increase heart rate and blood pressure, potentially leading to arrhythmias, such as tachycardia (rapid heart rate) or atrial fibrillation.
Opioids, while generally slowing heart rate, can, in overdose situations, cause bradycardia (slow heart rate) and QT prolongation, a condition that increases the risk of life-threatening ventricular arrhythmias.
Tricyclic antidepressants, another class of drugs, are also known for causing QT prolongation and other conduction abnormalities that can be detected on an EKG.
QT Prolongation: A Key Indicator
QT prolongation is a particularly important EKG finding in the context of drug use. The QT interval represents the time it takes for the ventricles of the heart to depolarize and repolarize.
Certain drugs can lengthen this interval, increasing the risk of a potentially fatal arrhythmia called Torsades de Pointes.
While QT prolongation can be drug-induced, it can also be caused by congenital conditions, electrolyte imbalances, or other medications, making interpretation challenging.
Limitations and Challenges
Despite its potential, using an EKG to detect drug use has significant limitations. The changes observed on an EKG are rarely specific to a single substance.
Many factors can influence EKG readings, including age, sex, underlying medical conditions, and other medications a patient is taking.
This lack of specificity means that an abnormal EKG should never be used as the sole basis for diagnosing drug use; it requires further investigation.
The Importance of Clinical Context
Interpreting an EKG in the context of suspected drug use requires a thorough assessment of the patient's clinical presentation. This includes gathering a detailed medical history, inquiring about current medications and any known substance use, and performing a physical examination.
Symptoms such as chest pain, palpitations, shortness of breath, or altered mental status, coupled with suggestive EKG findings, can raise suspicion of drug-related cardiac effects.
In such cases, further diagnostic testing, such as blood or urine drug screens, is necessary to confirm the diagnosis.
Ethical and Legal Considerations
The potential use of EKGs to detect drug use raises ethical and legal concerns. Patient privacy and confidentiality are paramount.
Using medical information obtained from an EKG for purposes other than the patient's direct medical care, without their consent, could be a violation of privacy laws.
Furthermore, there is a risk of misinterpretation or overreliance on EKG findings, leading to false accusations of drug use and potential discrimination.
Informed Consent and Transparency
To mitigate these risks, it is crucial that patients are fully informed about the purpose of an EKG and how the results will be used. Obtaining informed consent before performing an EKG is essential.
Healthcare providers should be transparent about the limitations of EKGs in detecting drug use and avoid making assumptions or judgments based solely on EKG findings.
Policies and procedures should be in place to protect patient privacy and prevent the misuse of EKG data.
The Future of Drug Detection and Cardiac Monitoring
While EKGs are not a substitute for traditional drug screening methods, ongoing research may lead to more sophisticated algorithms and technologies that can improve the accuracy of drug detection using cardiac monitoring. For example, AI-powered tools are being developed to analyze EKG patterns and identify subtle changes that may be indicative of drug use, even in the absence of overt clinical symptoms.
Future research should focus on developing more specific and sensitive biomarkers that can distinguish between drug-induced cardiac effects and other causes of EKG abnormalities. This would help to reduce the risk of false positives and improve the clinical utility of EKGs in the context of drug use.
Ultimately, the responsible and ethical use of EKGs in detecting drug use requires a multidisciplinary approach, involving healthcare providers, policymakers, and patients, to ensure that the benefits of this technology are realized while safeguarding individual rights and promoting public health.





/assets/images/provider/photos/2655460.jpg)