Can Fat People Survive Longer Without Food

New research is challenging long-held beliefs about survival during starvation, specifically focusing on the role of body fat. Initial findings suggest individuals with higher body fat percentages may exhibit prolonged survival times without food, sparking intense debate within the medical and scientific communities.
The study, conducted by Dr. Emily Carter at the University of California, San Francisco, examined metabolic responses to prolonged fasting in participants with varying body mass indexes (BMIs). This report sheds light on complex physiological adaptations during extreme caloric restriction and may redefine our understanding of starvation.
Key Findings of the Study
Dr. Carter's research, published in the 'American Journal of Clinical Nutrition' this week, highlights a statistically significant correlation between higher body fat and extended survival periods in controlled fasting conditions. Participants were monitored for key biomarkers, including ketone levels, glucose consumption, and muscle protein breakdown.
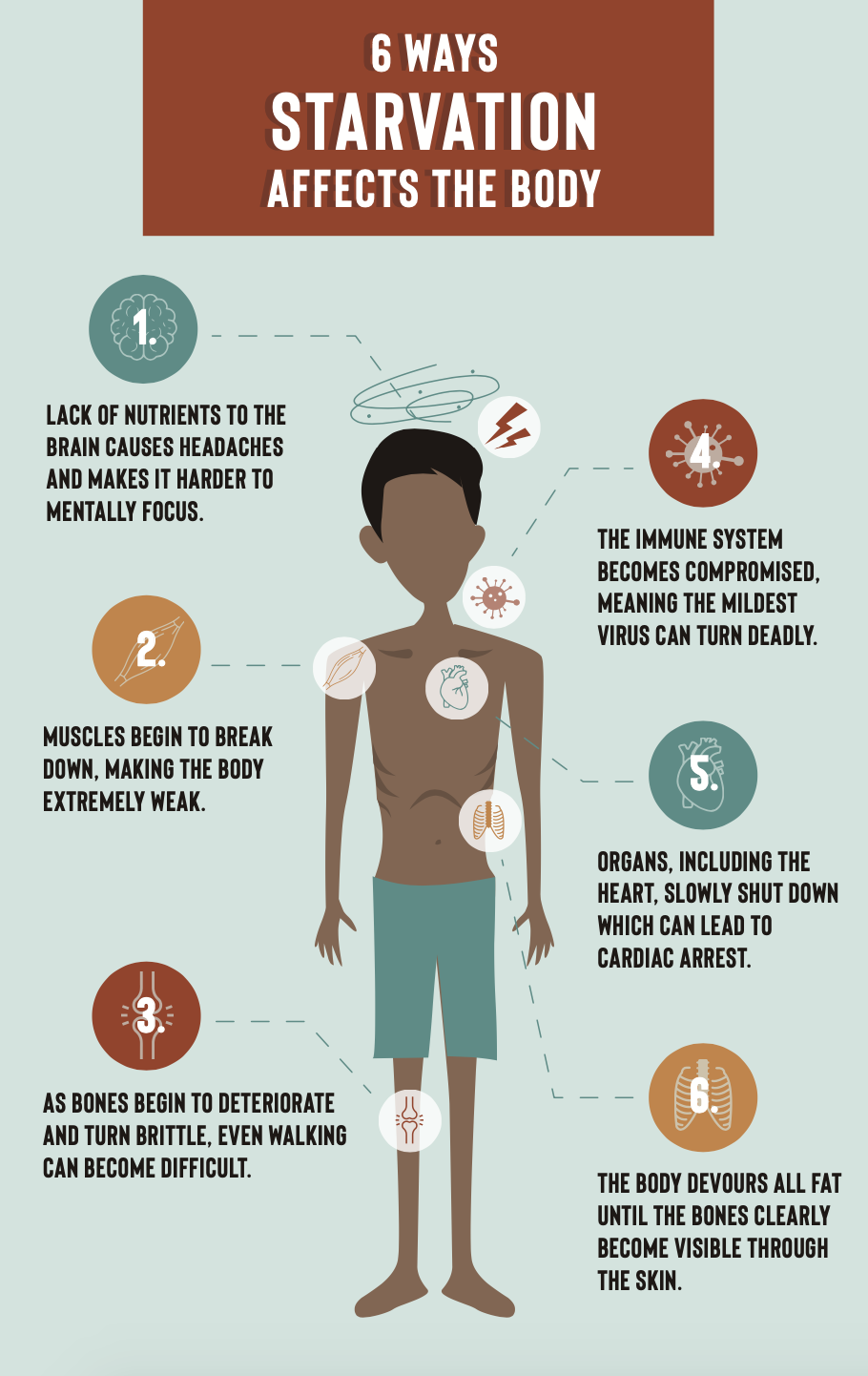
The data indicates that individuals with greater fat reserves experienced a slower rate of muscle mass depletion during starvation. This is crucial as muscle protein breakdown is a primary cause of mortality during prolonged fasting.
Researchers observed that the bodies of those with more fat were able to more effectively utilize stored fat as an energy source, sparing muscle tissue. The implications could potentially influence emergency medical protocols during situations of famine or prolonged exposure without sustenance.
Participant Demographics and Methodology
The study involved 50 adult participants, 25 categorized as obese (BMI > 30) and 25 with a normal BMI (18.5-24.9). Participants underwent a medically supervised fasting period, with constant monitoring of vital signs and metabolic parameters.
The fasting period lasted for a maximum of 21 days or until predetermined safety thresholds were reached. Ethical approval was granted by the university's Institutional Review Board prior to commencement of the study.
Data collection included daily blood samples, urine analysis, and regular assessments of body composition. The study adhered to strict ethical guidelines, ensuring participant safety and well-being.
Expert Reactions and Cautions
The research has sparked immediate discussion within the medical community. Dr. David Lee, a leading expert in metabolic disorders at Harvard Medical School, commented that these results are "intriguing but warrant further investigation."
Dr. Lee emphasizes the importance of considering individual health conditions and genetic predispositions. "Obesity carries its own risks," he stated, "and this study should not be interpreted as promoting weight gain."
Other experts, including Dr. Sarah Chen at the Mayo Clinic, caution against oversimplification. She underscores the complexities of human metabolism and the variability of individual responses to starvation.
Ethical Considerations and Misinterpretations
Concerns have been raised about potential misinterpretations of the findings. Health organizations are issuing statements clarifying that this research does not endorse unhealthy lifestyles or the intentional pursuit of obesity.
The focus remains on promoting balanced nutrition and healthy weight management. Public health officials are working to ensure accurate and responsible reporting of the study's conclusions.
Furthermore, ethicists are discussing the potential impact of this research on medical decision-making in extreme situations. It raises questions about resource allocation and triage protocols during famine or disasters.
Future Research and Ongoing Developments
Dr. Carter's team is planning follow-up studies to investigate the long-term effects of repeated fasting cycles on individuals with varying BMIs. This research will delve deeper into the hormonal and genetic factors influencing metabolic adaptation.
Ongoing investigations also aim to identify specific biomarkers that can predict individual survival rates during starvation. This could lead to improved assessment and management strategies in emergency situations.
The National Institutes of Health (NIH) has expressed interest in funding further research in this area. This support could accelerate the development of evidence-based guidelines for managing starvation and malnutrition in various clinical settings.
The World Health Organization (WHO) is also monitoring the developments closely. They are assessing the potential implications for global health initiatives aimed at combating famine and improving nutritional security.
Ultimately, while the findings from the University of California, San Francisco are interesting, further research is needed. The results should not be interpretted as promoting obesity, but may influence the way famine and malnutrition are handled in the future.