Can You Develop Gluten Sensitivity Later In Life
:max_bytes(150000):strip_icc()/surprising-signs-you-may-have-a-gluten-allergy-4147574_final-a5ba89e52afc4be98dcb6320d35a13fa.jpg)
New research indicates that gluten sensitivity can emerge at any age, challenging previous assumptions. This unexpected development is prompting revised diagnostic approaches and dietary considerations for adults experiencing gastrointestinal distress.
For years, gluten sensitivity, often referred to as non-celiac gluten sensitivity (NCGS), was primarily associated with childhood or early adulthood. The emerging evidence suggests a need for heightened awareness and adaptable testing strategies to accommodate late-onset cases.
Rising Cases of Late-Onset Gluten Sensitivity
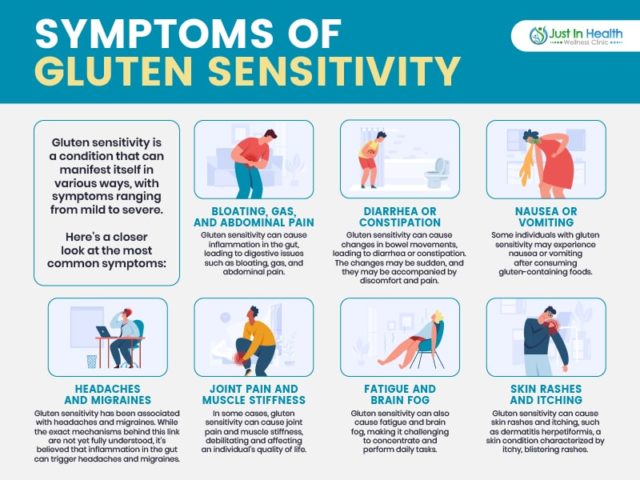
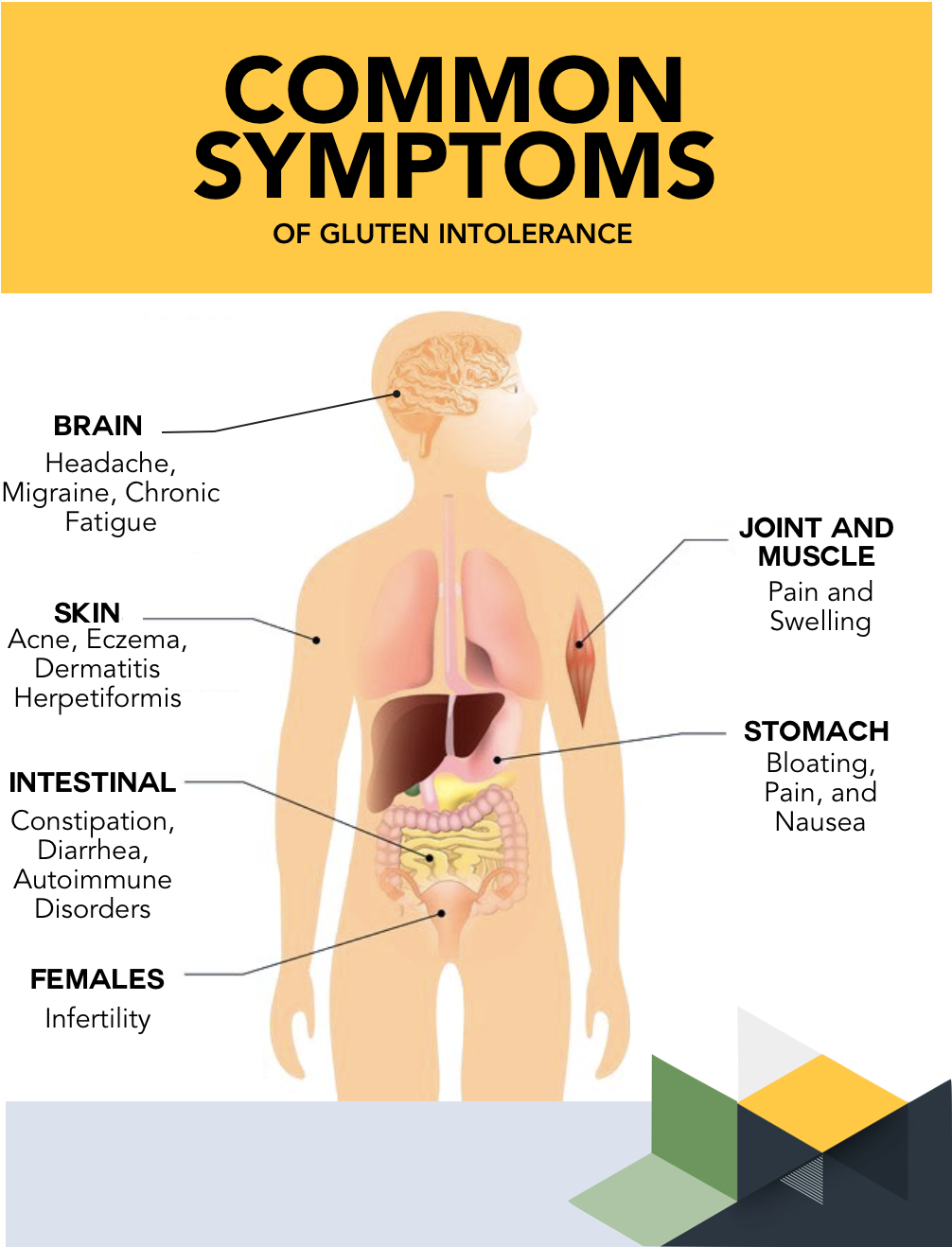
Gastroenterologists are reporting an increase in adult patients presenting with symptoms mirroring gluten sensitivity despite previously tolerating gluten without issue. These symptoms include bloating, abdominal pain, fatigue, and brain fog.
Dr. Emily Carter, a leading gastroenterologist at the University of California, San Francisco, notes a significant shift. "We're seeing a rise in patients over 40, even 50, who are suddenly experiencing gluten-related discomfort," she states.
A recent study published in the American Journal of Gastroenterology highlighted that nearly 15% of newly diagnosed NCGS cases were in individuals over 50.
What Triggers Late-Onset Gluten Sensitivity?
The exact causes remain under investigation, but several factors are suspected to play a role. These include changes in gut microbiota, increased intestinal permeability (leaky gut), and alterations in the immune system.
Gut microbiota, the complex community of microorganisms residing in the digestive tract, can be influenced by diet, medication, and stress. These changes can potentially trigger an adverse reaction to gluten.
Intestinal permeability, the ease with which substances can pass through the intestinal lining, can also be affected by various factors. Increased permeability may allow gluten proteins to trigger an immune response.
Stress, both physical and psychological, can also alter gut function and potentially contribute to the development of gluten sensitivity later in life.
Diagnostic Challenges
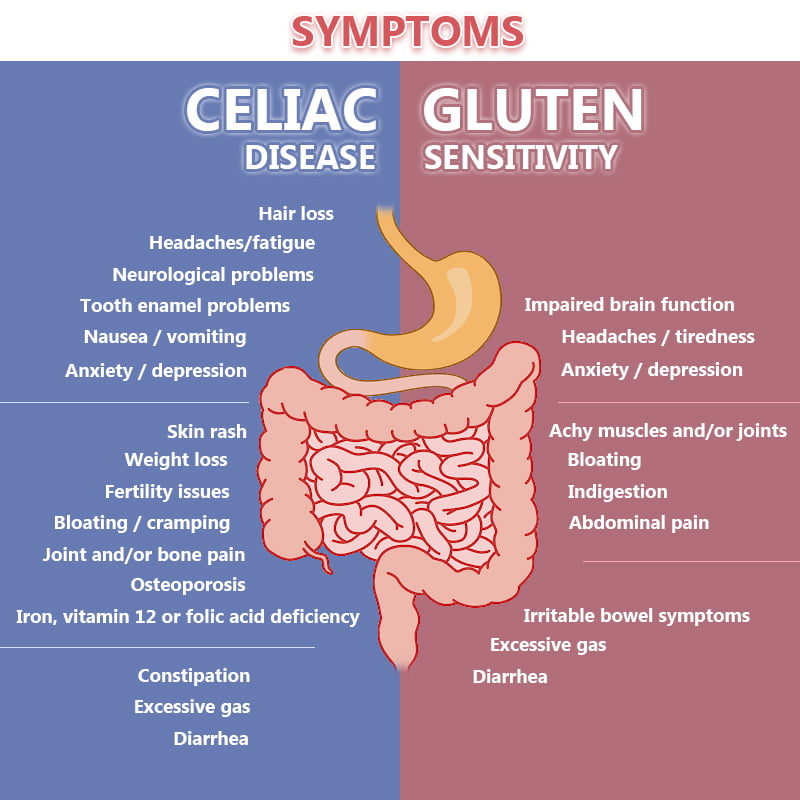
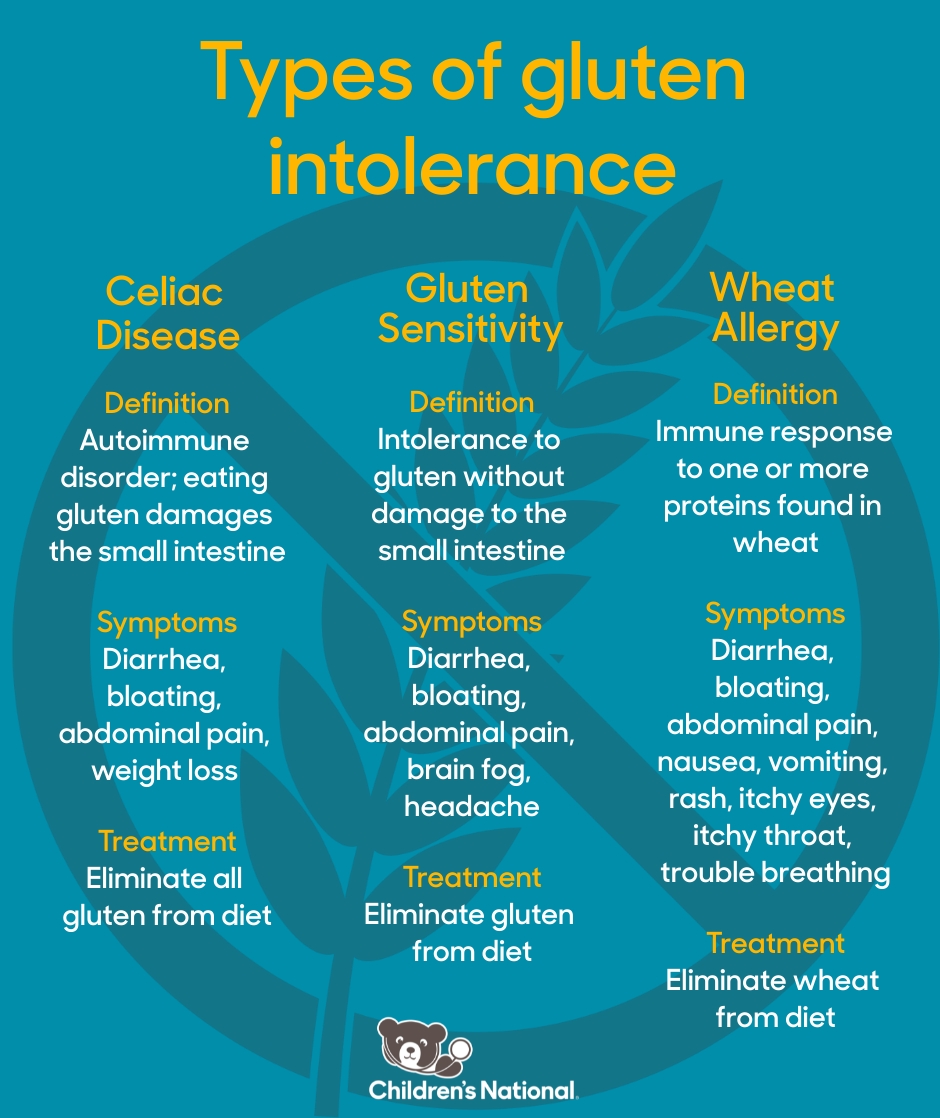
Diagnosing late-onset gluten sensitivity presents unique challenges. Traditional diagnostic methods primarily focus on ruling out celiac disease and wheat allergy.
Celiac disease is an autoimmune disorder triggered by gluten, characterized by damage to the small intestine. Wheat allergy involves an allergic reaction to proteins found in wheat.
NCGS is diagnosed after excluding these conditions and observing symptom improvement on a gluten-free diet. This process can be lengthy and subjective.
Dr. David Miller, a researcher at the Mayo Clinic, emphasizes the need for more precise diagnostic markers. "We desperately need biomarkers to objectively identify NCGS and differentiate it from other gastrointestinal disorders," he explains.
Dietary Management and Lifestyle Adjustments
The primary treatment for gluten sensitivity involves adhering to a gluten-free diet. This means eliminating wheat, barley, and rye from the diet.
Many individuals also find relief by addressing underlying gut health issues. This may involve taking probiotics, managing stress, and adopting an anti-inflammatory diet.
Consulting with a registered dietitian or nutritionist is crucial for developing a personalized dietary plan and ensuring adequate nutrient intake.
Important Considerations
Individuals suspecting they have developed gluten sensitivity should consult with a healthcare professional. Self-diagnosing and initiating a gluten-free diet without proper medical evaluation can mask other underlying conditions.
Accurate diagnosis is crucial to ensure appropriate management and prevent unnecessary dietary restrictions.
Ongoing research is exploring potential therapies and preventative measures for gluten sensitivity. Stay informed about the latest developments from reputable sources.
Next Steps
Researchers are actively investigating potential biomarkers and diagnostic tools for NCGS. Clinical trials are underway to evaluate the effectiveness of various treatments, including specific enzyme supplements and gut-healing protocols.
Continued research is crucial to improve our understanding of the underlying mechanisms of gluten sensitivity and develop targeted interventions.
Healthcare professionals are urged to remain vigilant and consider NCGS in adult patients presenting with unexplained gastrointestinal symptoms, even in the absence of a prior history.

:max_bytes(150000):strip_icc()/Health-Gluten-Intolerance-GettyImages-1489991903-horizontal-v3-4d28cc83e392437297545787fdab040a.jpg)







:max_bytes(150000):strip_icc()/VWH-MichelaButtignol-CeliacGlutenSensitivity-txt-4000x2700-cee0537425b04c1485793fb1ec8aab4f.png)




