Can You Have Yeast And Bv At The Same Time

Imagine that familiar, unsettling itch. The discomfort that whispers, "Something's not right down there." You reach for the over-the-counter yeast infection treatment, hoping for quick relief. But this time, something feels different. It's not just the itch; there's an unusual odor, maybe a different kind of discharge. You're left wondering, could it be something else entirely, or even… both?
The question of whether you can experience a yeast infection and bacterial vaginosis (BV) simultaneously is more common than you might think. While they are distinct conditions with different causes, their symptoms can overlap, leading to confusion and sometimes, co-occurrence. Understanding the nuances of each condition is crucial for accurate diagnosis and effective treatment, allowing you to reclaim your comfort and confidence.
Understanding the Vaginal Ecosystem
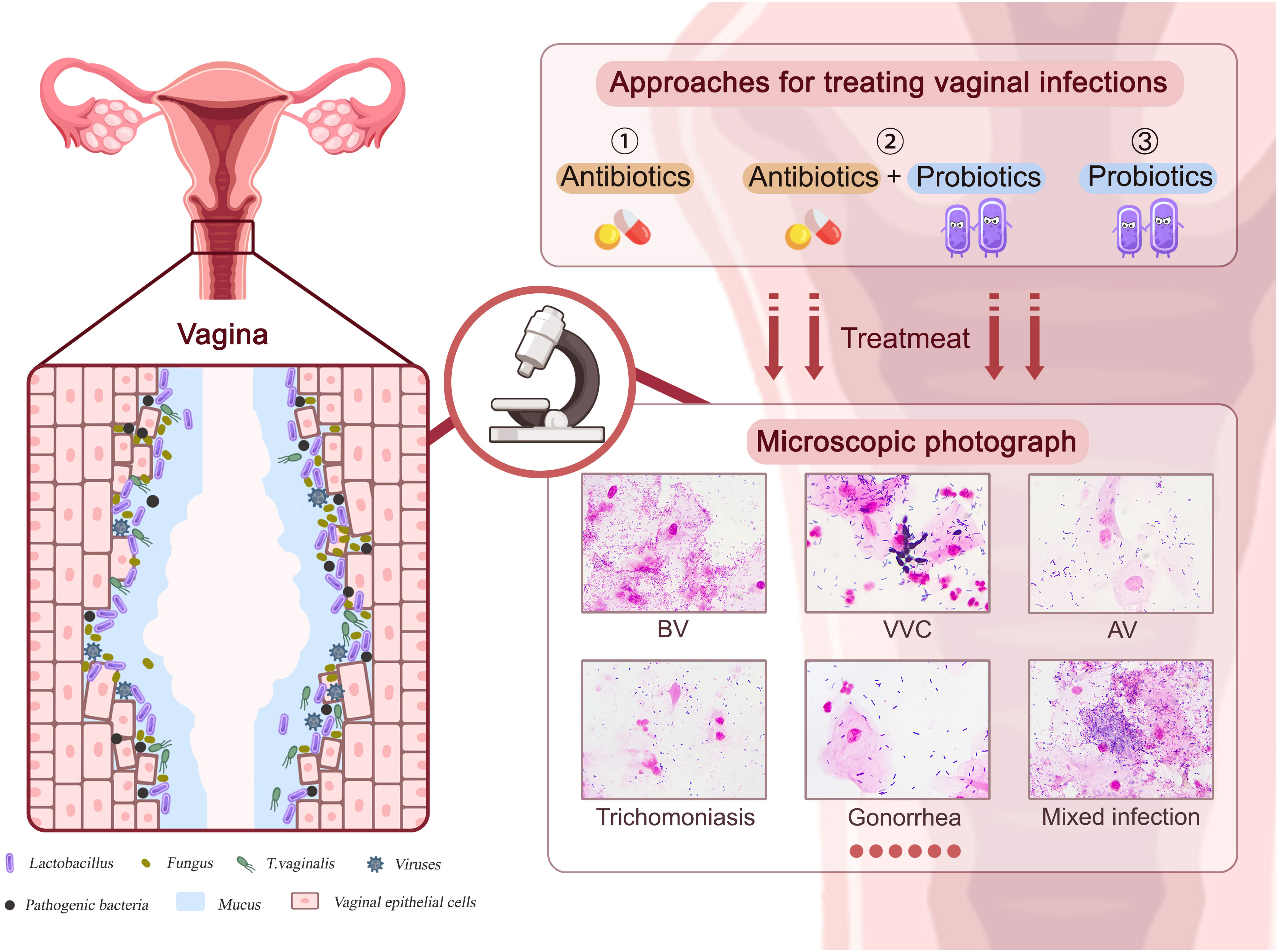
The vagina is a complex ecosystem, a delicate balance of bacteria, yeast, and other microorganisms. This ecosystem, also known as the vaginal microbiome, plays a vital role in maintaining vaginal health. Lactobacilli are the dominant bacteria, producing lactic acid that keeps the vaginal pH at a healthy level, typically between 3.8 and 4.5. This acidic environment discourages the overgrowth of harmful organisms.
When this delicate balance is disrupted, problems can arise. Factors such as antibiotics, douching, hormonal changes (like those during menstruation, pregnancy, or menopause), and even certain soaps or detergents can throw the vaginal microbiome out of whack. This imbalance can create an opportunity for opportunistic infections like yeast infections or BV to take hold.
Yeast Infections: An Overgrowth of Fungus
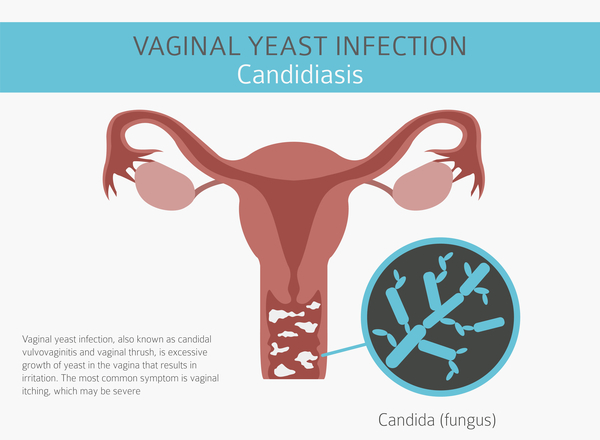
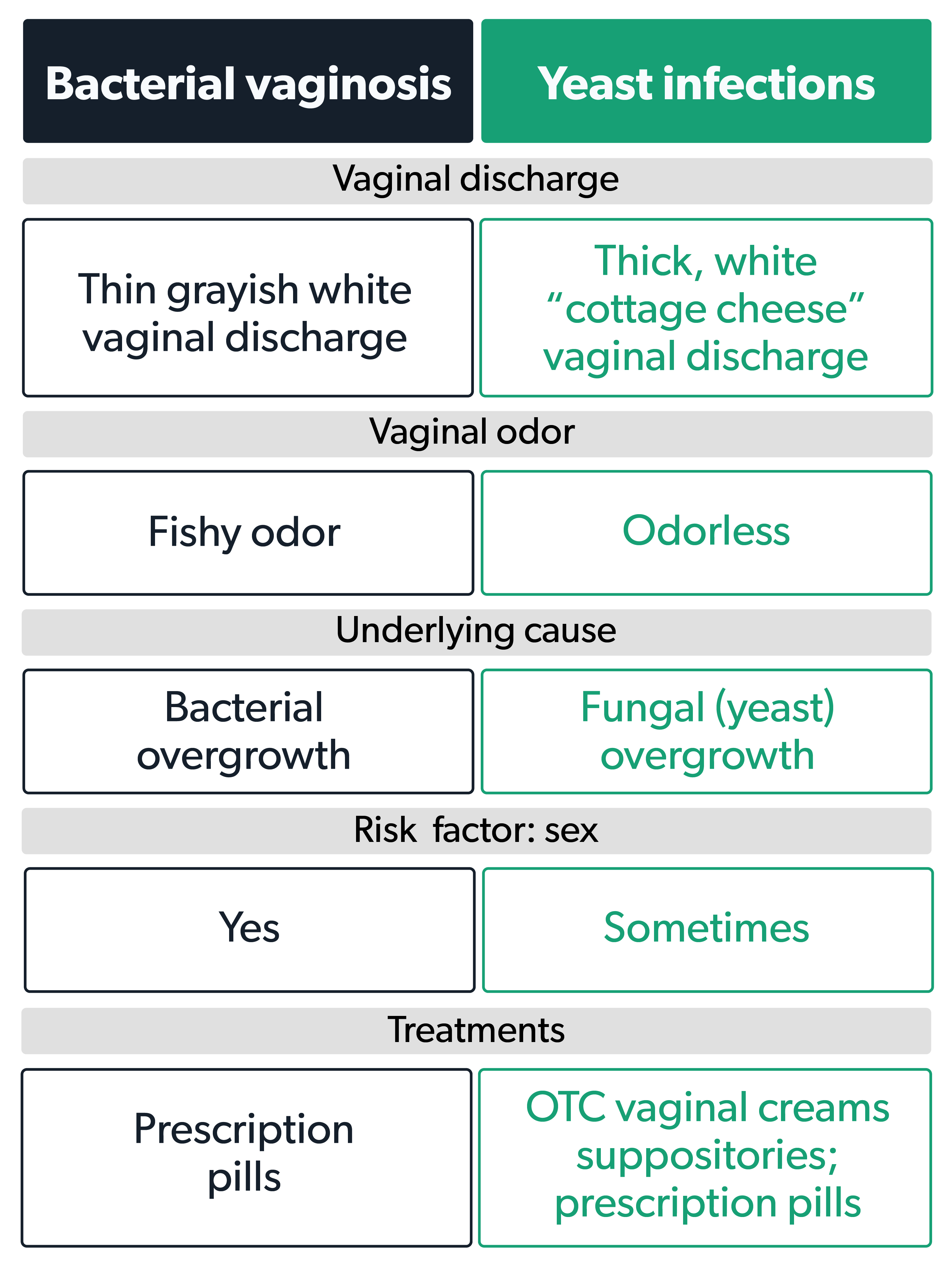
A yeast infection, also known as vulvovaginal candidiasis, is caused by an overgrowth of Candida, a type of fungus that naturally lives in the vagina. While several Candida species can cause infections, Candida albicans is the most common culprit. Symptoms typically include intense itching, burning, redness, and a thick, white, cottage cheese-like discharge.
Yeast infections are often triggered by factors that disrupt the vaginal pH, such as antibiotic use (which kills beneficial bacteria), hormonal changes (like increased estrogen levels during pregnancy), or a weakened immune system. Diabetes, if poorly controlled, can also increase the risk of yeast infections due to higher sugar levels in vaginal secretions, providing fuel for Candida.
Treatment for yeast infections usually involves antifungal medications, available as creams, suppositories, or oral tablets. Over-the-counter options are often effective for uncomplicated yeast infections. However, recurrent or severe infections may require prescription-strength medication or a longer course of treatment. It's always a good idea to consult with a healthcare professional to confirm the diagnosis and rule out other potential causes of your symptoms.
Bacterial Vaginosis: A Bacterial Imbalance
Bacterial vaginosis (BV), on the other hand, is a result of an imbalance in the vaginal bacteria. Specifically, it occurs when the normally dominant lactobacilli are replaced by an overgrowth of other bacteria, such as Gardnerella vaginalis. Unlike yeast infections, BV is not considered a sexually transmitted infection (STI), although it is more common in sexually active women.
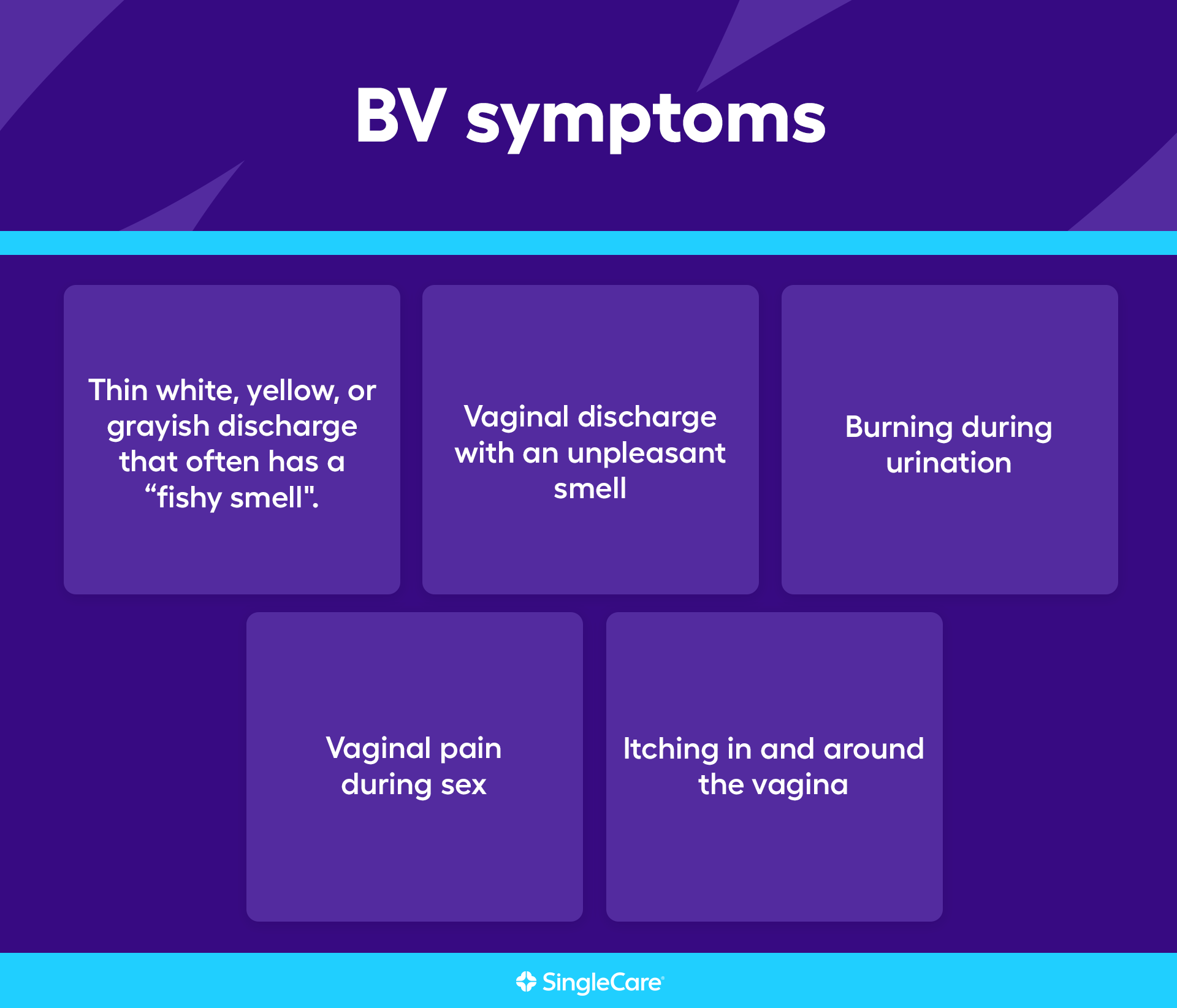
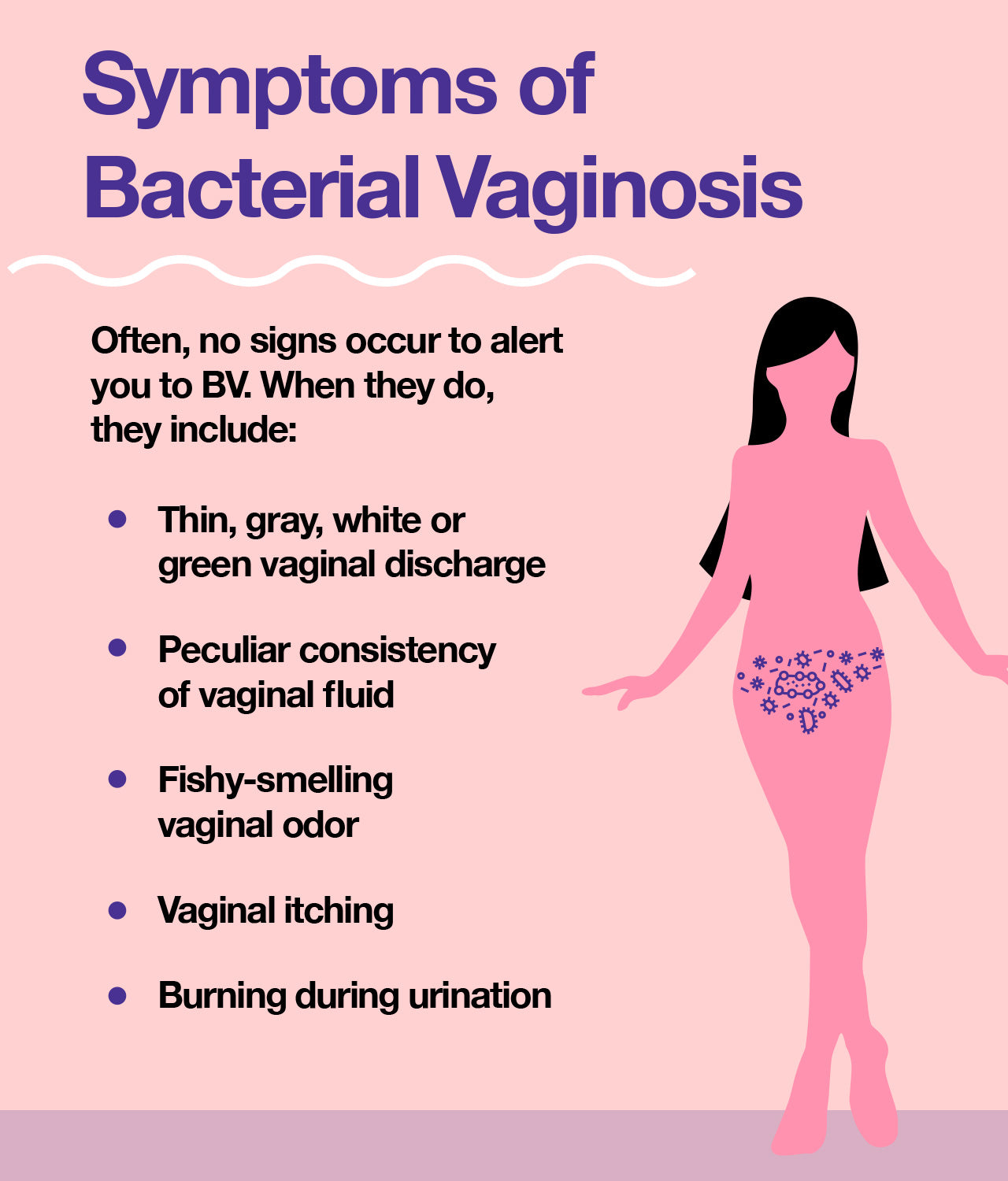
The hallmark symptom of BV is a thin, grayish-white discharge with a distinct fishy odor. Some women may also experience itching or burning, although many women with BV have no symptoms at all. Douching, using scented feminine hygiene products, and having multiple sexual partners can increase the risk of BV by disrupting the vaginal flora.
BV is typically treated with antibiotics, either oral or vaginal. It's important to complete the entire course of antibiotics, even if your symptoms improve, to ensure the infection is completely eradicated. Unlike yeast infections, over-the-counter treatments are not effective for BV, and it's crucial to seek medical attention for diagnosis and treatment.
Can You Have Both? The Possibility of Co-occurrence
Yes, it is entirely possible to have both a yeast infection and bacterial vaginosis at the same time. While they are separate conditions, the factors that disrupt the vaginal ecosystem can sometimes create an environment conducive to both infections. For instance, antibiotic use can wipe out beneficial bacteria, making you susceptible to both a yeast overgrowth and BV.
Furthermore, some women may misdiagnose themselves, thinking they have a yeast infection when they actually have BV, or vice versa. The overlapping symptoms of itching, burning, and discharge can make it difficult to distinguish between the two without a proper examination and testing by a healthcare professional.
According to the Centers for Disease Control and Prevention (CDC), the only way to know for sure if you have a yeast infection, BV, or both is to get tested by a doctor or other healthcare provider. A simple swab of the vaginal discharge can be examined under a microscope or sent to a lab for further analysis to identify the specific organisms present.
Diagnosis and Treatment: Seeking Expert Advice
If you suspect you have either a yeast infection, BV, or both, it's essential to seek medical advice. A healthcare provider can perform a pelvic exam and collect a sample of vaginal discharge for testing. This will help determine the exact cause of your symptoms and ensure you receive the appropriate treatment.
Treating both conditions simultaneously usually involves addressing each infection separately. For example, you may be prescribed an antifungal medication for the yeast infection and antibiotics for the BV. It's crucial to follow your healthcare provider's instructions carefully and complete the entire course of treatment for both infections to prevent recurrence and complications.
Ignoring symptoms or attempting to self-treat without a proper diagnosis can lead to prolonged discomfort, recurrent infections, and potentially more serious complications, such as pelvic inflammatory disease (PID) in the case of untreated BV. Furthermore, some symptoms that resemble yeast infections or BV could be indicative of other underlying conditions, such as STIs, which require different treatment approaches.
Prevention and Maintenance: Promoting Vaginal Health
Maintaining a healthy vaginal ecosystem is key to preventing both yeast infections and BV. Some simple lifestyle modifications can help promote a healthy balance of bacteria and yeast. Avoid douching, as it disrupts the natural vaginal flora. Use unscented soaps and detergents, and avoid using scented feminine hygiene products.
Wear breathable cotton underwear to allow for better air circulation and reduce moisture. After swimming or exercising, change out of wet clothes promptly. Practice safe sex by using condoms to reduce the risk of STIs, which can sometimes disrupt the vaginal microbiome. Consider incorporating probiotics into your diet or taking a probiotic supplement, as some strains of lactobacilli have been shown to help maintain a healthy vaginal flora.
Finally, be mindful of your overall health. Managing underlying conditions like diabetes and maintaining a healthy immune system can help reduce your susceptibility to vaginal infections. Open communication with your healthcare provider about any concerns or changes in your vaginal health is also crucial for early detection and prompt treatment.
Reclaiming Your Comfort and Confidence
Experiencing vaginal discomfort can be frustrating and even embarrassing, but remember that you're not alone. Understanding the differences between yeast infections and BV, recognizing the possibility of co-occurrence, and seeking professional medical advice are crucial steps in reclaiming your comfort and confidence.
By prioritizing your vaginal health, adopting preventive measures, and working closely with your healthcare provider, you can effectively manage these conditions and maintain a healthy and balanced vaginal ecosystem. Don't hesitate to speak up and seek the care you need. Your health and well-being are worth it.
Ultimately, listening to your body and seeking guidance from healthcare professionals empowers you to navigate the complexities of vaginal health with knowledge and confidence. Remember, taking proactive steps to understand and address these common concerns can lead to lasting comfort and peace of mind.







:max_bytes(150000):strip_icc()/VWH_Illustration_Tips-to-Prevent-a-Yeast-Infection_Illustrator_Laura-Porter_Final-2b3b48db3f86497e9094532164a6086d.jpg)