Can You Take Collagen With Blood Thinners

Urgent concerns are emerging about the safety of combining collagen supplements with blood thinners. New research is prompting experts to re-evaluate potential interactions that could impact patient health.
This article addresses the vital question: Can you safely take collagen with blood thinners? Understanding the potential risks is crucial for anyone considering or currently using both.
The Core Issue: Collagen and Blood Thinners - A Risky Mix?
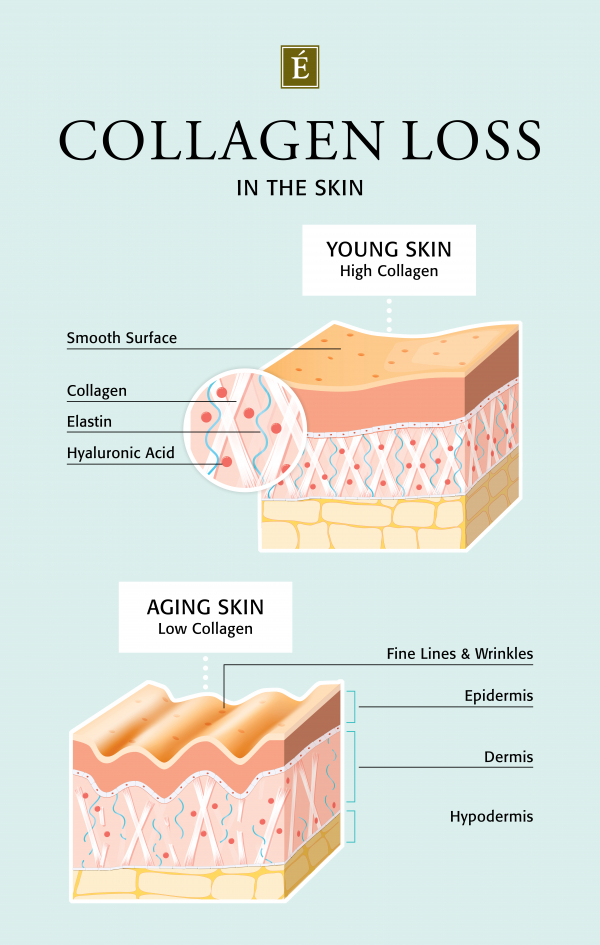
The primary concern revolves around collagen's potential antiplatelet effects. Platelets are vital for blood clotting. Blood thinners, also known as anticoagulants, work to reduce the risk of dangerous clots.
Collagen, particularly certain types, may interfere with platelet aggregation. This interference, combined with the effects of blood thinners, could increase the risk of bleeding.
What the Experts Say
Dr. Anya Sharma, a leading hematologist at the National Institute of Health, warns about a lack of definitive studies. "We don't have robust clinical trials specifically examining collagen and blood thinner interactions," she states. "This is a critical gap in our understanding."
Dr. Sharma emphasizes the need for caution. She highlights that anecdotal reports suggest increased bruising and prolonged bleeding times in some patients taking both collagen and anticoagulants.
However, some experts hold a different view, stating that collagen is safe and that no clinical trials demonstrated its harmful effect. They highlight the benefits of collagen for joint health and skin elasticity, and that this should not be overlooked.
Who is Most at Risk?
Individuals taking prescription blood thinners are most vulnerable. This includes patients on warfarin (Coumadin), heparin, enoxaparin (Lovenox), apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa).
Those with underlying bleeding disorders should also exercise extreme caution. Any potential interaction could exacerbate their condition.
Patients scheduled for surgery must inform their doctors about collagen supplement use. Surgeons require complete knowledge of all medications and supplements to manage bleeding risks during and after procedures.
What Type of Collagen Matters?
The type of collagen supplement might influence the risk. Some studies suggest that collagen derived from marine sources could have stronger antiplatelet effects than bovine collagen.
However, the scientific evidence is limited. More research is needed to definitively determine which collagen types pose the greatest threat when combined with blood thinners.
Regardless of the collagen source, it's vital to have an open discussion with your doctor.
Where is the Data Coming From?
Current concerns stem from case reports, preclinical studies, and expert opinions.
"We are primarily relying on extrapolated data and theoretical risks at this point,"explains Dr. Ben Carter, a cardiologist at Mayo Clinic.
The information is derived from observed effects of collagen on platelets in lab settings. These effects have not been consistently replicated in large-scale human trials.
Ongoing research aims to address this gap. Researchers are designing studies to evaluate the actual risk in patients taking both collagen and blood thinners.
How Can You Minimize Risk?
Always consult your doctor before starting any new supplement, especially if you are on blood thinners. This is the most important step you can take.
Disclose all medications and supplements you are currently taking. Your doctor can assess potential interactions and provide personalized recommendations.
If you choose to take collagen despite the risks, monitor yourself for signs of excessive bleeding. These signs may include nosebleeds, easy bruising, blood in your urine or stool, and prolonged bleeding from cuts.
When Should You Stop Taking Collagen?
Immediately stop taking collagen and contact your doctor if you experience any signs of increased bleeding. Do not delay seeking medical advice.
Prior to any surgical procedure, discontinue collagen use as instructed by your surgeon. This precaution minimizes the risk of bleeding complications during and after the operation.
Ultimately, the decision to take collagen while on blood thinners is a personal one, but must be made in consultation with a healthcare professional.
Next Steps and Ongoing Developments
Further research is underway to quantify the risks associated with collagen and blood thinners. These studies will provide more definitive guidance for patients and healthcare providers.
In the meantime, caution and open communication with your doctor are paramount. Until more conclusive data emerges, the potential for increased bleeding risk remains a serious concern.
Stay informed about the latest research and recommendations from reputable medical organizations. Your health and safety depend on making informed decisions based on the best available evidence.