Celiac Disease Can Cause Unstable Blood Sugar Control.
Urgent health alert: New research reveals a significant link between Celiac disease and unstable blood sugar levels, potentially impacting millions. Individuals with Celiac disease face an elevated risk of developing hypoglycemia and hyperglycemia, demanding immediate attention to dietary management and blood sugar monitoring.
This connection underscores the critical need for healthcare providers to screen Celiac patients for blood sugar irregularities. Proactive management can help prevent severe complications associated with both conditions.
The Connection: Celiac Disease and Blood Sugar
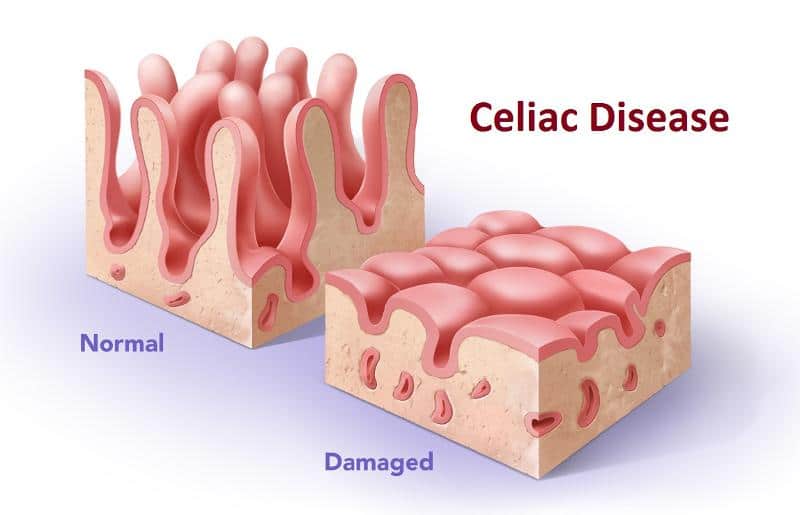
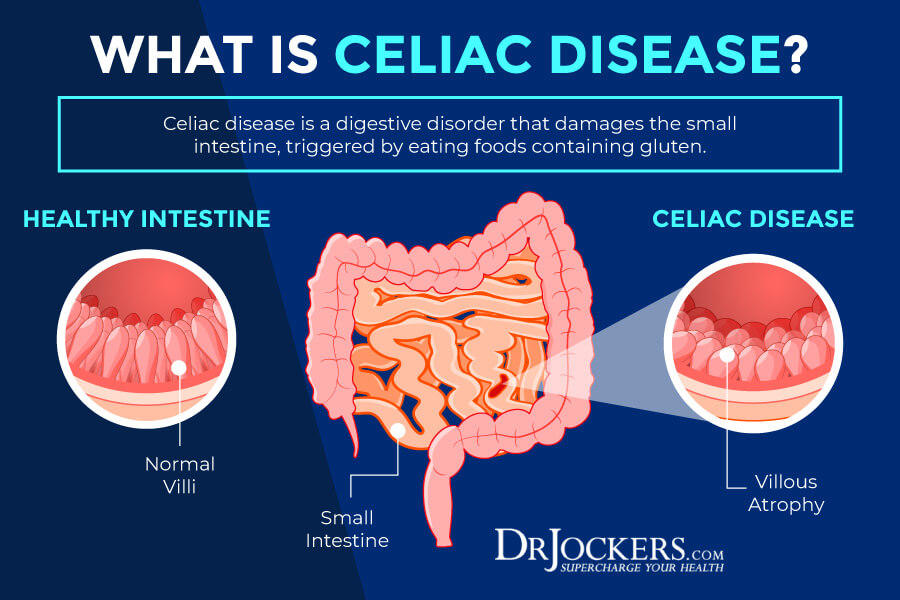
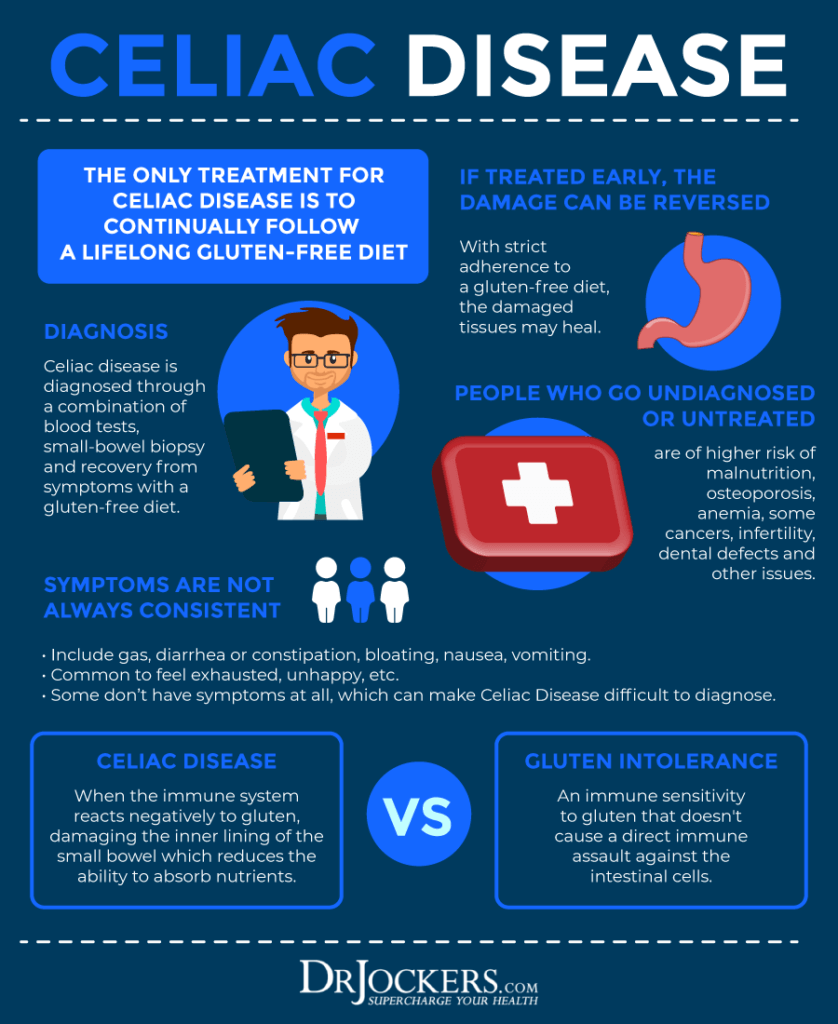
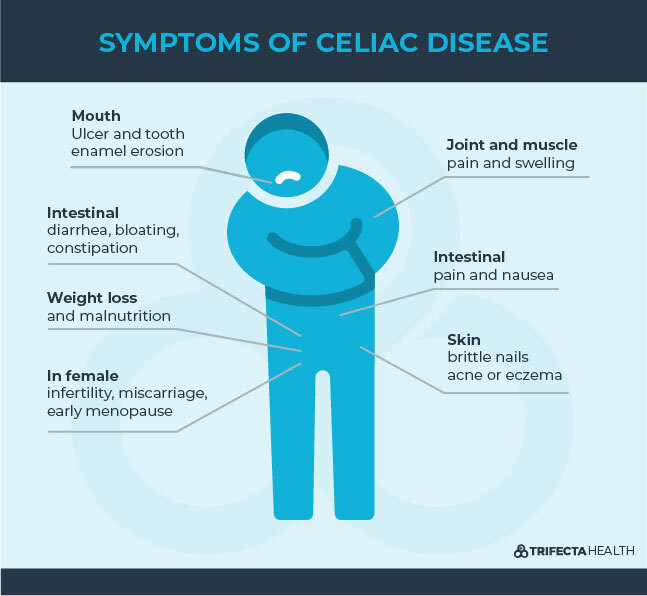
Celiac disease, an autoimmune disorder triggered by gluten consumption, damages the small intestine. This damage hinders nutrient absorption, including carbohydrates, which are crucial for maintaining stable blood sugar.
A study published in the American Journal of Gastroenterology found that individuals with Celiac disease were significantly more likely to experience fluctuations in blood glucose levels compared to those without the condition. The research indicates that malabsorption, a hallmark of Celiac disease, disrupts the body's ability to regulate blood sugar effectively.
Specifically, the damaged intestinal lining compromises the absorption of glucose, leading to both hypoglycemia (low blood sugar) when glucose isn't absorbed properly and hyperglycemia (high blood sugar) when the body struggles to process carbohydrates effectively.
Who is at Risk?
Anyone with a confirmed diagnosis of Celiac disease is potentially at risk for blood sugar instability. However, the risk is heightened for individuals with severe intestinal damage or those who are newly diagnosed and not yet adhering to a strict gluten-free diet.
Children with Celiac disease are also particularly vulnerable due to their growing bodies and developing metabolic systems.
Early diagnosis and adherence to a gluten-free diet are paramount in mitigating this risk.
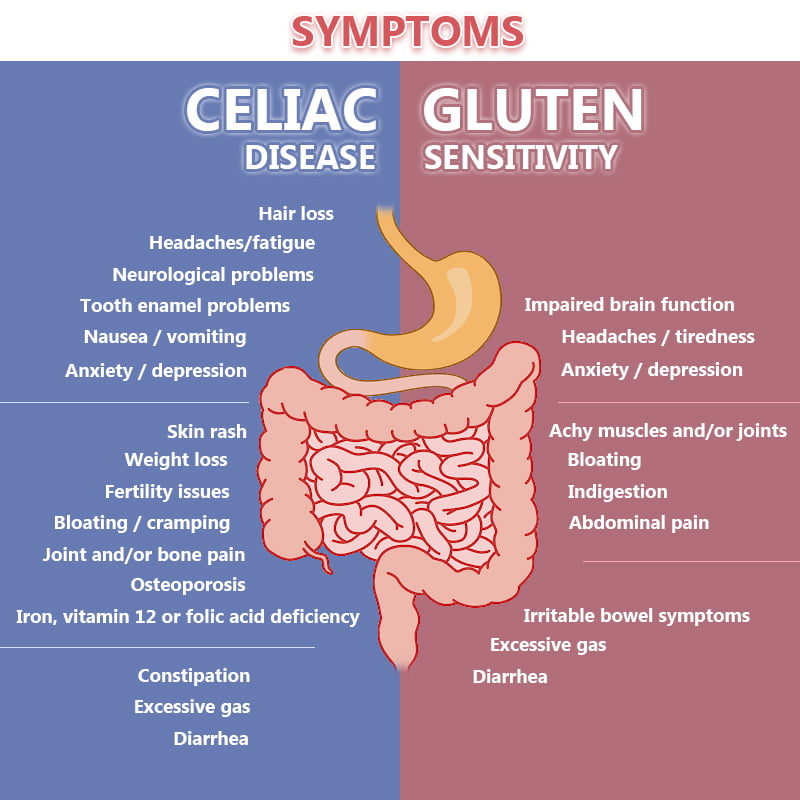
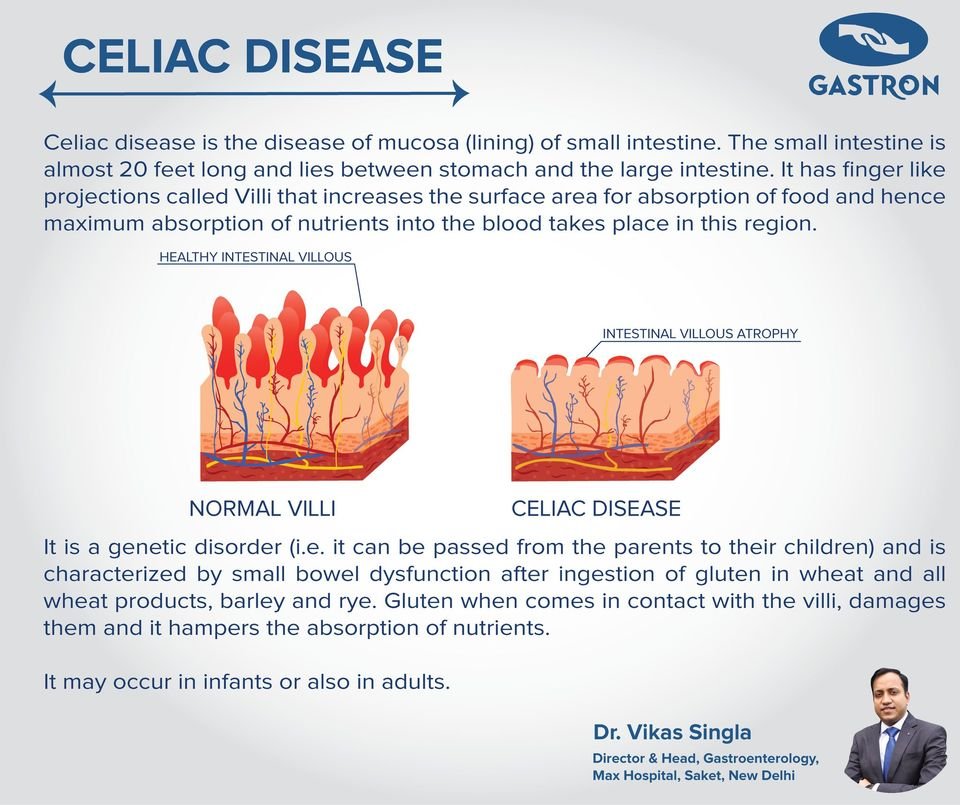
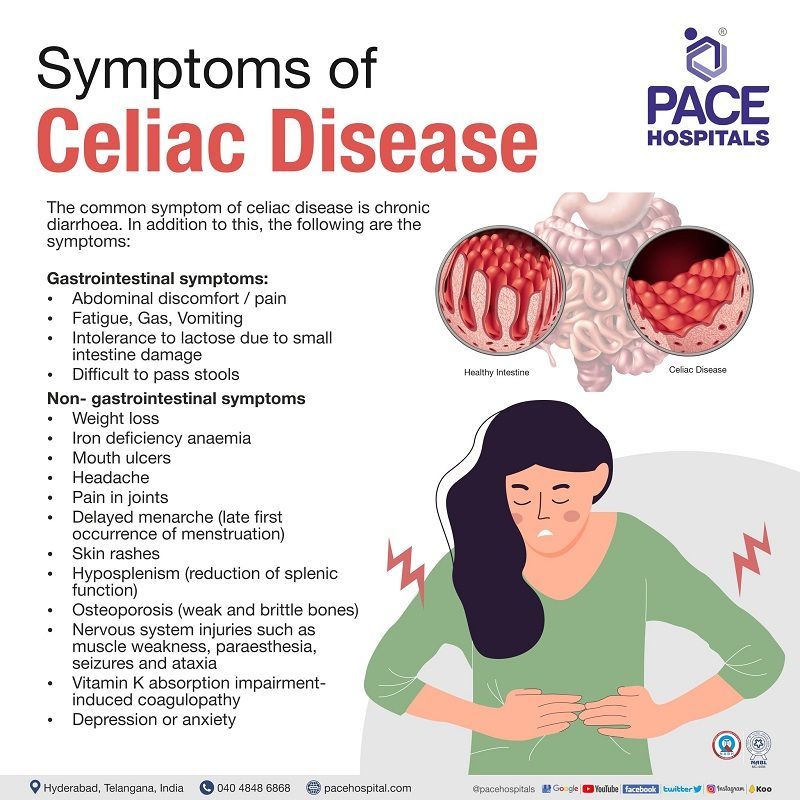
Symptoms to Watch For
Individuals with Celiac disease should be vigilant for symptoms of both hypoglycemia and hyperglycemia. Symptoms of hypoglycemia include shakiness, sweating, dizziness, confusion, and rapid heartbeat.
Conversely, symptoms of hyperglycemia may include increased thirst, frequent urination, blurred vision, and fatigue.
Any of these symptoms warrant immediate medical evaluation, especially if accompanied by a Celiac disease diagnosis.
The Role of a Gluten-Free Diet
The cornerstone of managing Celiac disease and mitigating blood sugar fluctuations is a strict, lifelong gluten-free diet. Avoiding all sources of gluten allows the small intestine to heal, improving nutrient absorption and potentially stabilizing blood sugar levels.
Consultation with a registered dietitian specializing in Celiac disease is crucial for developing a personalized dietary plan. This plan should ensure adequate carbohydrate intake and address any nutritional deficiencies.
Regular monitoring of blood glucose levels, as advised by a healthcare provider, is also essential for identifying and managing blood sugar irregularities.
Diagnosis and Management
Diagnosis of Celiac disease typically involves blood tests to detect specific antibodies and a biopsy of the small intestine. If Celiac disease is confirmed, further evaluation may be necessary to assess blood sugar control.
This could include fasting blood glucose tests, A1C testing (to measure average blood sugar levels over time), and continuous glucose monitoring (CGM) in some cases.
Management strategies often involve a combination of dietary modifications, regular blood sugar monitoring, and, in some cases, medication to manage blood sugar levels.
Expert Commentary
"This connection between Celiac disease and blood sugar instability highlights the importance of a holistic approach to patient care," says Dr. Emily Carter, a gastroenterologist specializing in Celiac disease. "We must screen Celiac patients for blood sugar irregularities and educate them about the potential risks and management strategies."
Dr. Carter emphasizes the need for collaboration between gastroenterologists, endocrinologists, and registered dietitians to provide comprehensive care for individuals with Celiac disease and unstable blood sugar.
The Impact on Public Health
The prevalence of Celiac disease is estimated to be around 1% of the population, meaning millions could be affected by this link to unstable blood sugar. Early detection and intervention are critical to prevent long-term complications, such as nerve damage, kidney disease, and cardiovascular problems.
Healthcare providers are urged to incorporate blood sugar screening into routine check-ups for Celiac patients and to educate them about the importance of dietary adherence and symptom awareness.
Public health campaigns are needed to raise awareness about this connection and to encourage individuals with Celiac disease to seek appropriate medical care.
Next Steps and Ongoing Research
Researchers are continuing to investigate the precise mechanisms by which Celiac disease affects blood sugar control. Future studies may explore the role of gut microbiota and inflammation in this complex interaction.
Further research is also needed to determine the most effective strategies for managing blood sugar instability in individuals with Celiac disease. This includes evaluating different dietary approaches and the potential benefits of various medications.
Individuals with Celiac disease experiencing symptoms of blood sugar irregularities should consult their healthcare provider immediately. Ongoing research and increased awareness will pave the way for improved diagnosis and management of this critical health issue.





![Celiac Disease Can Cause Unstable Blood Sugar Control. [DIAGRAM] Diagram Of Celiac Disease FULL Version HD Quality Celiac](https://www.gicare.com/wp-content/uploads/2014/12/Fig13.jpg)



:max_bytes(150000):strip_icc()/VWH-MichelaButtignol-SomePotentialSymptomsofCeliacDisease-Standard-d5e2c29ef0d04dbbbe14c9369fbcab5f.jpg)

:max_bytes(150000):strip_icc()/celiac-disease-overview-4014748_FINAL-1699755e0f7f46b4b70965dd0b5a6da6.png)
