Chart Audits Find The Following Practice Errors
The healthcare landscape is facing increased scrutiny as a growing number of chart audits reveal alarming patterns of practice errors across various medical facilities. These audits, designed to ensure compliance and improve patient safety, are uncovering a range of issues, from inadequate documentation to potential billing fraud. The implications for both patient well-being and the financial stability of healthcare organizations are significant.
The recent surge in chart audits highlights critical systemic failures within healthcare practices. A "nut graf" should address the scope and importance of the issue and this article aims to unpack the findings of these audits, explore the types of errors commonly identified, and discuss the potential consequences for patients and practitioners alike. It also will provide insight on solutions and how to prevent future mistakes from happening.
Scope and Methodology of Chart Audits
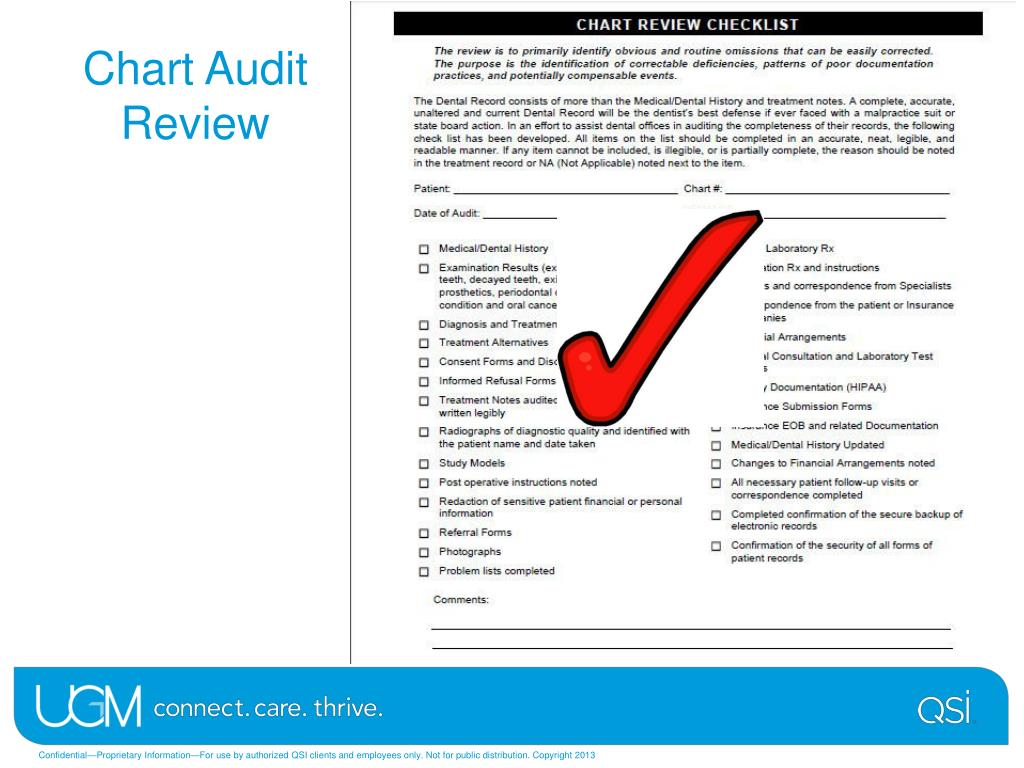
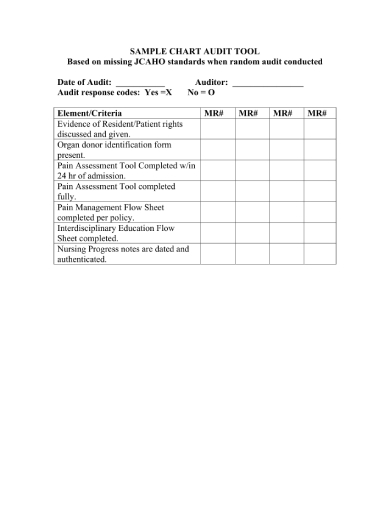
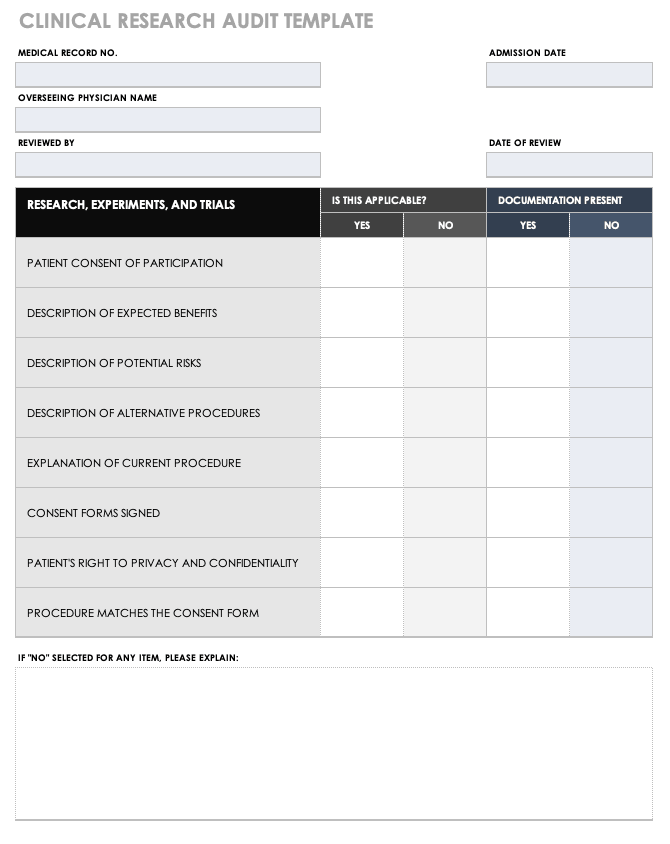
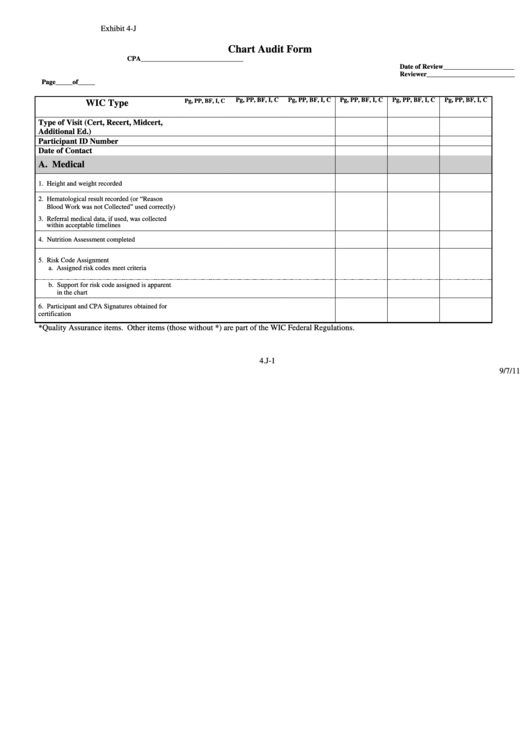
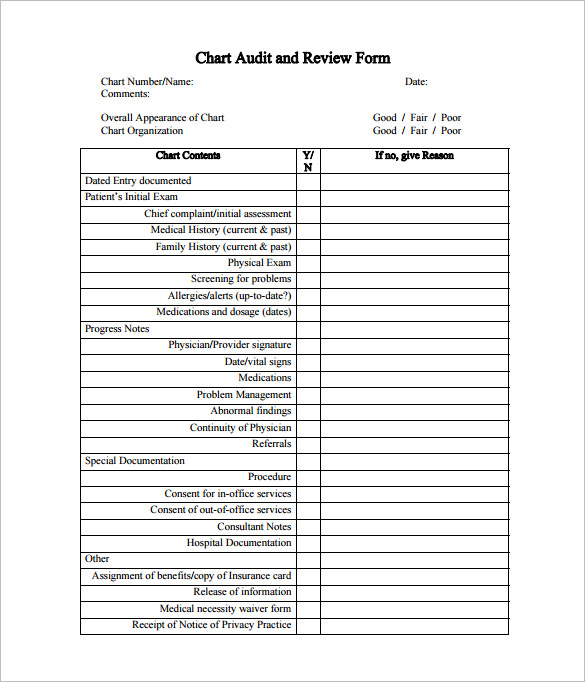
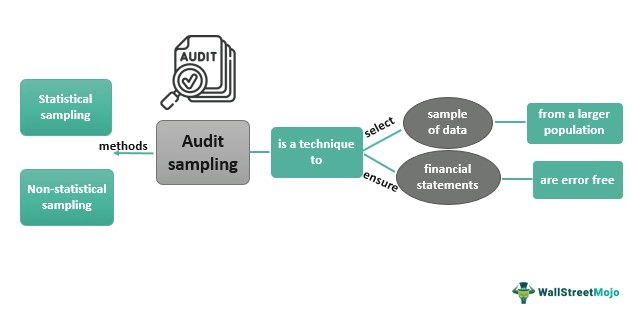
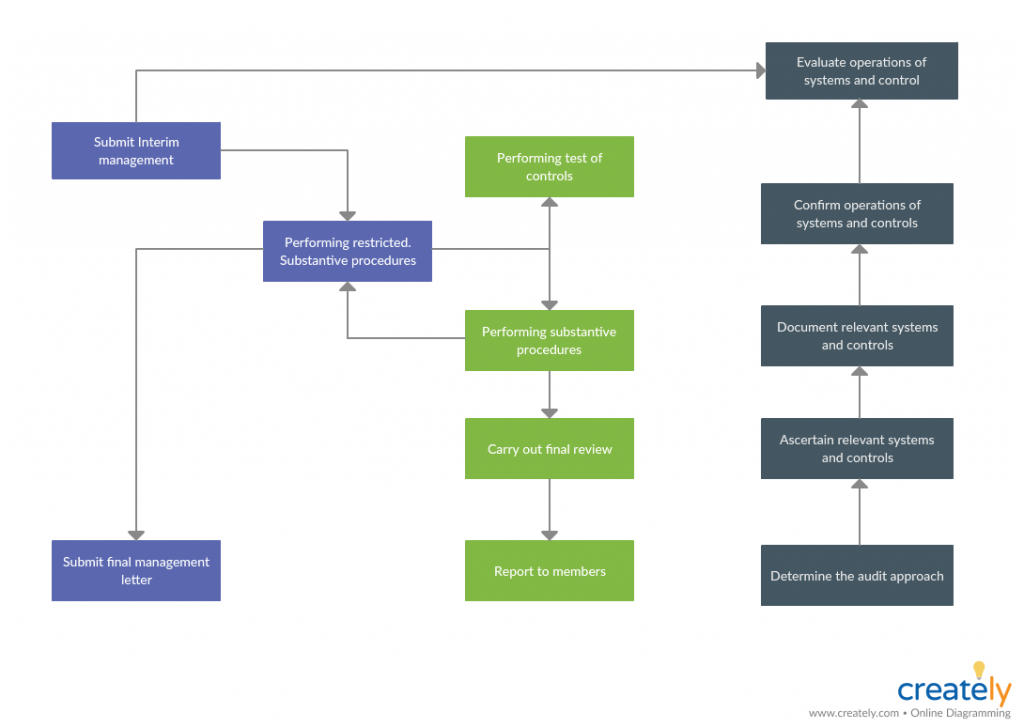
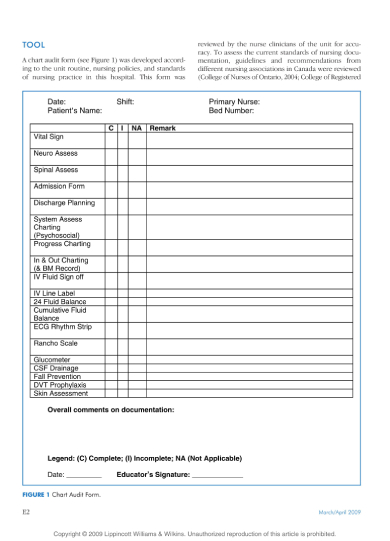
Chart audits are systematic reviews of patient medical records, conducted to assess the accuracy, completeness, and compliance of documentation. They are often initiated by regulatory bodies, insurance companies, or internal quality assurance teams.
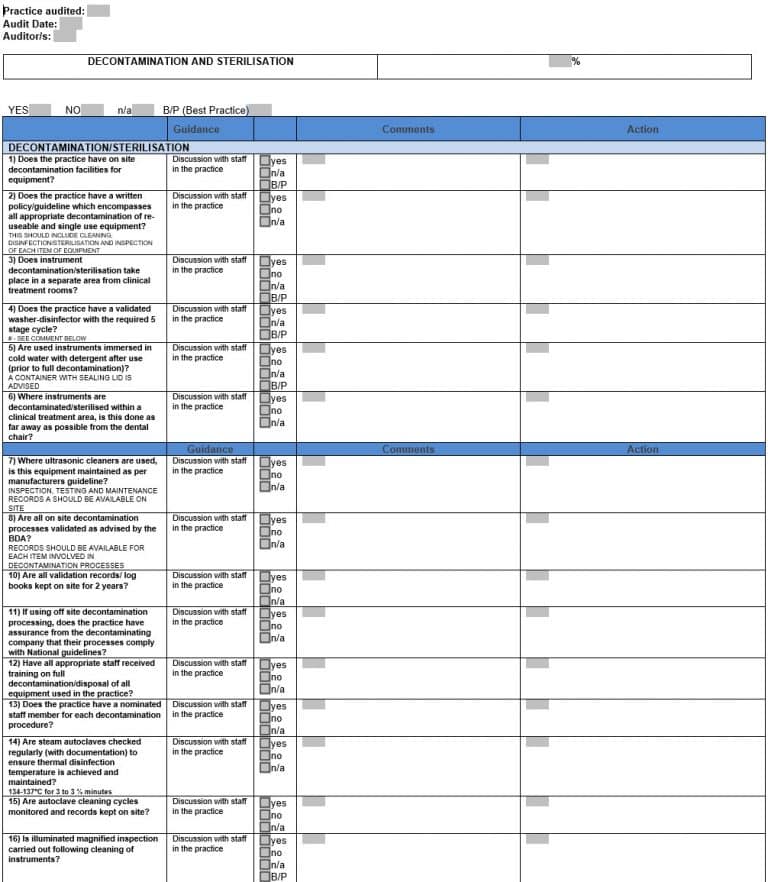
The auditing process involves examining various aspects of patient charts, including the accuracy of diagnoses, the appropriateness of treatment plans, and the adherence to established protocols. Auditors use established criteria and guidelines, often based on Centers for Medicare & Medicaid Services (CMS) regulations, to identify discrepancies and errors.
Common Errors Uncovered
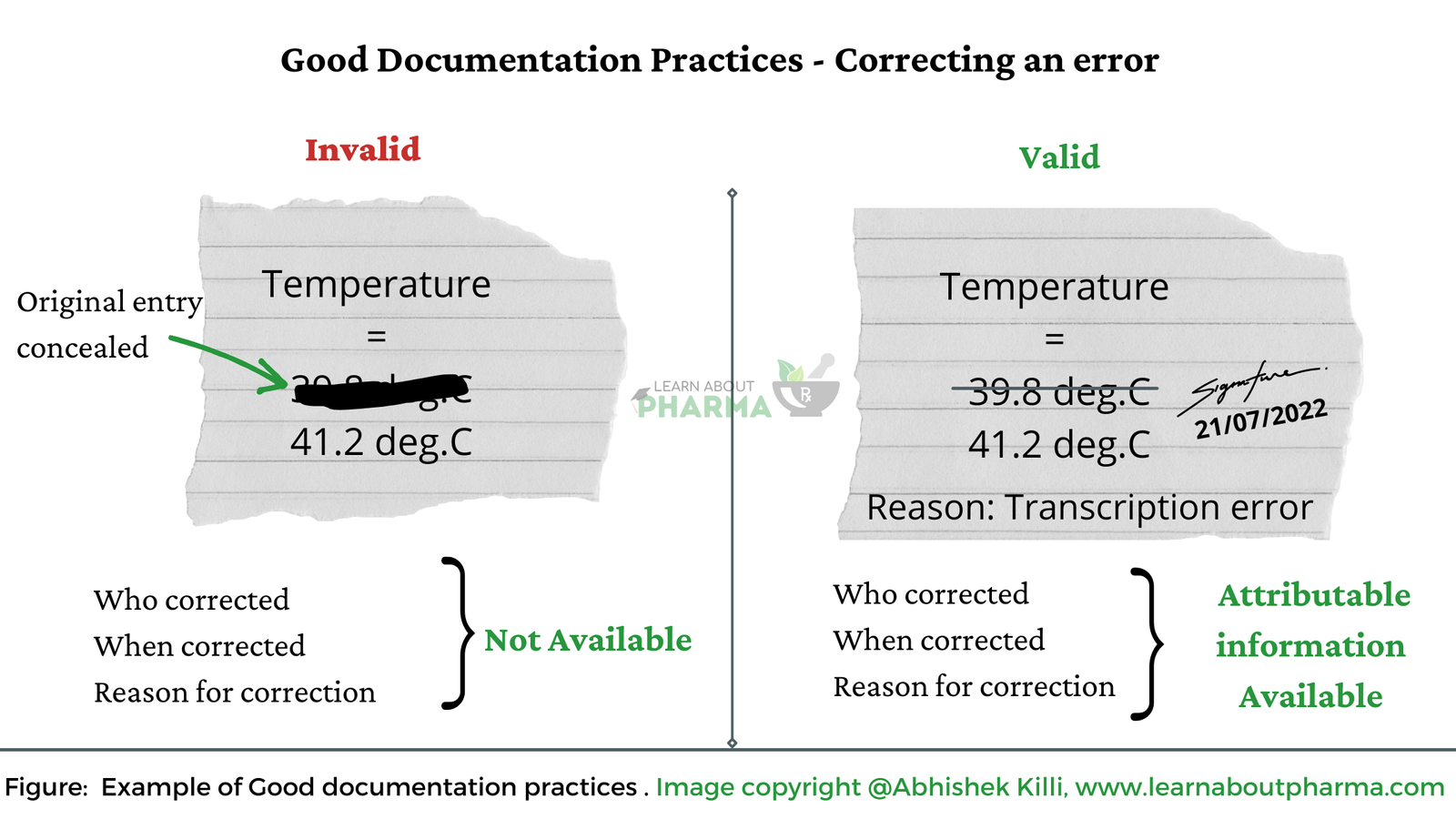
Chart audits are consistently revealing a number of recurring errors across different medical specialties. One of the most prevalent issues is inadequate documentation. This includes incomplete patient histories, missing or illegible notes, and a failure to document informed consent.
Another significant problem is coding and billing errors. Practices are sometimes incorrectly coding services or upcoding, which means billing for a more expensive service than was actually provided. This leads to overpayments from insurance companies or patients and can lead to legal penalties.
Audits also identify issues related to medication management. This encompasses failures to document medication allergies, drug interactions, and adverse reactions, as well as errors in prescribing and administering medications. Moreover, some practices failed to use tools that could support the medical decision when prescribing medicine.
Case Studies and Examples
In one instance, an audit of a large primary care practice revealed that 30% of patient charts lacked documentation of key vital signs. This omission could lead to missed diagnoses and inadequate patient monitoring.
Another audit of a surgical center found that a significant number of procedures were incorrectly coded. The center was billing for complex procedures when the simpler version of the procedures were performed, resulting in substantial overpayments from insurers and leading to legal ramifications.
Consequences for Patients and Practitioners
The errors identified in chart audits can have serious consequences for patient safety. Inaccurate or incomplete documentation can lead to misdiagnosis, delayed treatment, and adverse medical events.
Coding and billing errors can result in financial hardship for patients, as well as legal and financial penalties for practitioners and healthcare organizations. The reputation of medical facilities can also be tarnished, leading to a loss of patient trust.
Expert Perspectives
“Chart audits are an essential tool for identifying and correcting errors that can compromise patient safety and lead to financial penalties,” says Dr. Emily Carter, a healthcare compliance consultant. She argues that the audits are important to protect all parties.
John Davis, a healthcare attorney specializing in compliance, emphasizes the importance of proactive compliance measures. “Healthcare providers should implement regular internal audits and training programs to ensure that they are meeting all regulatory requirements,” he stated, noting the need for ongoing vigilance.
Preventive Measures and Solutions
To address the identified issues, healthcare organizations need to implement a comprehensive approach to error prevention. One key step is to improve documentation practices through standardized templates and training programs. These programs should focus on ensuring that all relevant information is accurately and completely recorded in patient charts.
Another crucial measure is to implement robust coding and billing compliance programs. These programs should include regular audits, coding updates, and staff training to minimize the risk of errors. Also, using new technologies and tools would support the medical team.
Technology can also play a significant role in reducing errors. Electronic health records (EHRs) with built-in decision support tools can help providers avoid medication errors and ensure adherence to clinical guidelines. EHRs help ensure patients receive the necessary treatment.
The Role of Technology
The adoption of advanced data analytics tools can also help identify patterns of errors and areas for improvement. These tools can analyze large volumes of data from patient charts to identify trends and anomalies that might otherwise go unnoticed.
Furthermore, telehealth and remote monitoring technologies offer opportunities to improve patient care and reduce the risk of errors. Telehealth appointments can increase access to care and allow for more frequent monitoring of patients, while remote monitoring devices can provide real-time data on patient health status.
Looking Ahead: The Future of Chart Audits
As healthcare becomes increasingly complex and regulated, chart audits will continue to play a vital role in ensuring patient safety and compliance. The focus is shifting towards more proactive and preventive approaches, with healthcare organizations implementing continuous monitoring systems and real-time feedback mechanisms.
By embracing technology, prioritizing training, and fostering a culture of compliance, healthcare providers can minimize the risk of errors and improve the quality of care they provide. The goal is to make healthcare as safe and secure as possible for all patients.