Choose All Of The Following That Affect Peripheral Resistance.

Immediate action is crucial as understanding the dynamics of peripheral resistance impacts treatment strategies for hypertension and related cardiovascular diseases. Factors influencing this key physiological parameter are now under intense scrutiny.
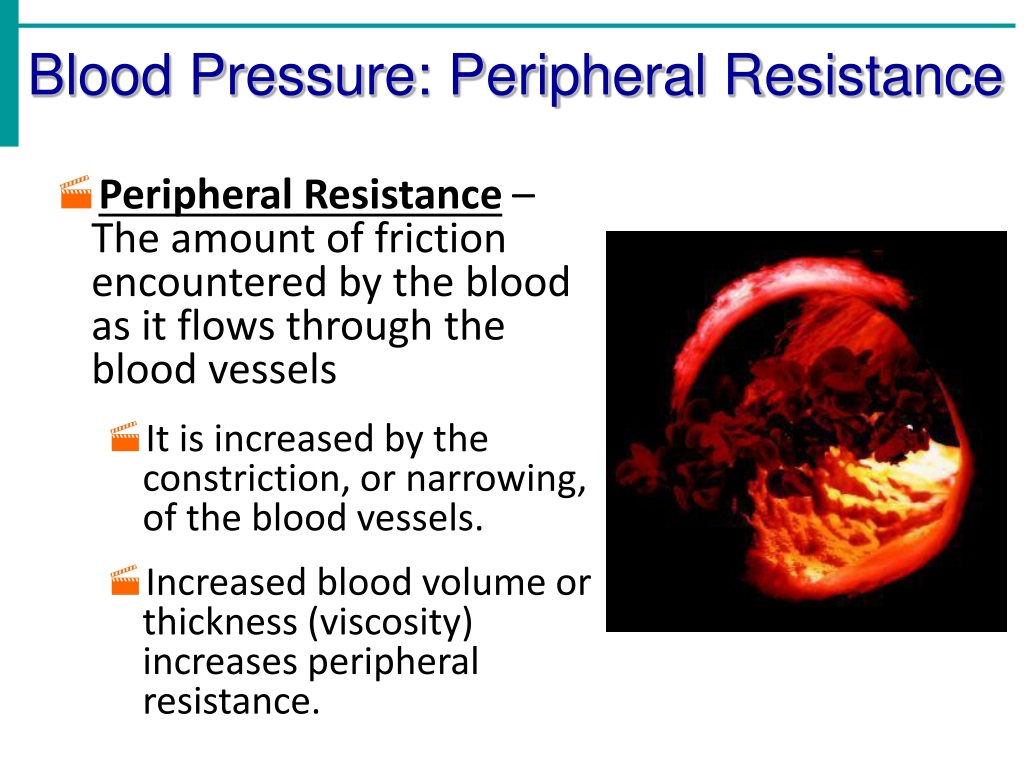
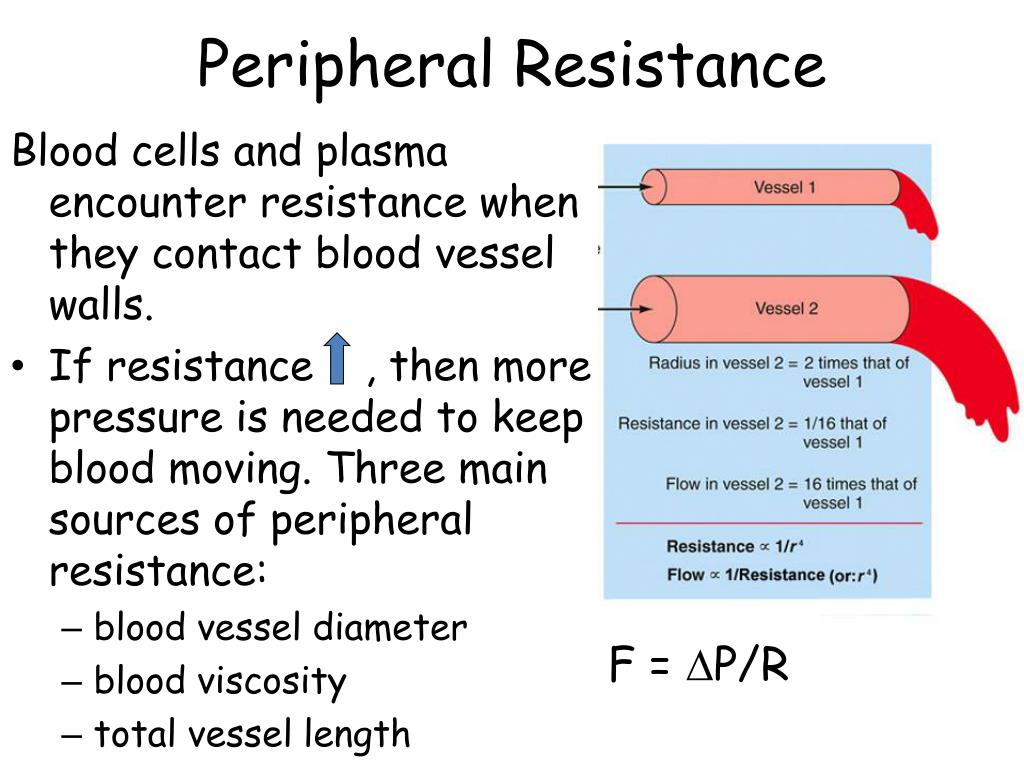
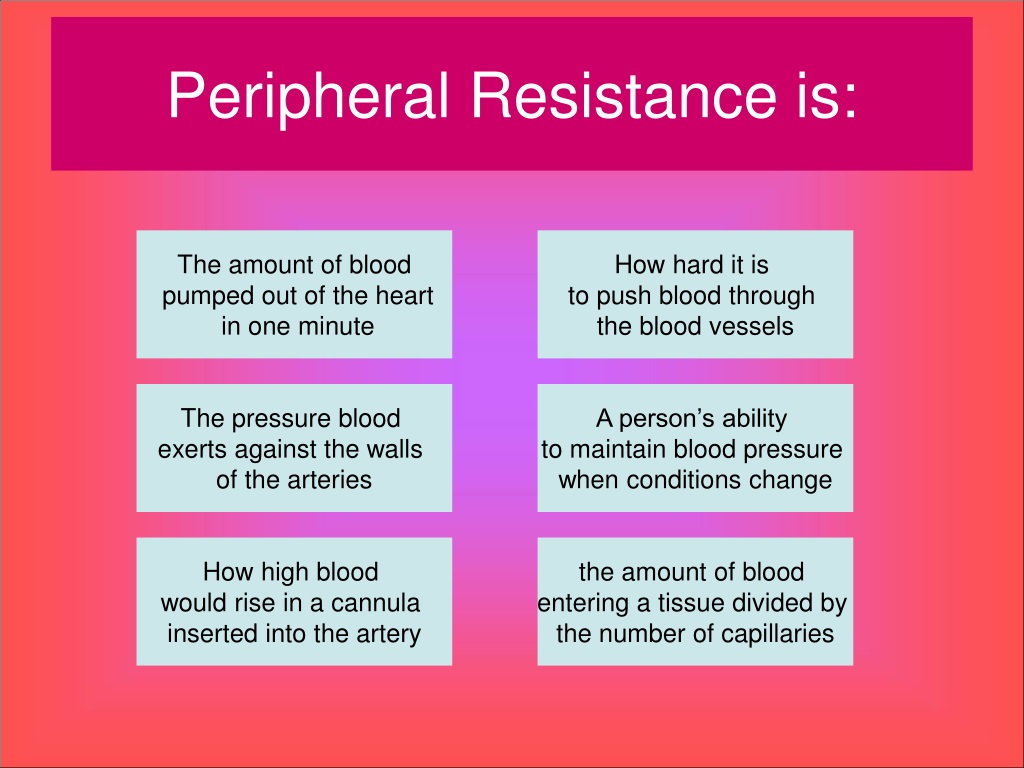
Peripheral resistance, the opposition to blood flow in the arteries, dictates how hard the heart must work to circulate blood. Identifying and managing the factors that modulate it is vital in preventing and treating cardiovascular diseases.
Key Factors Influencing Peripheral Resistance
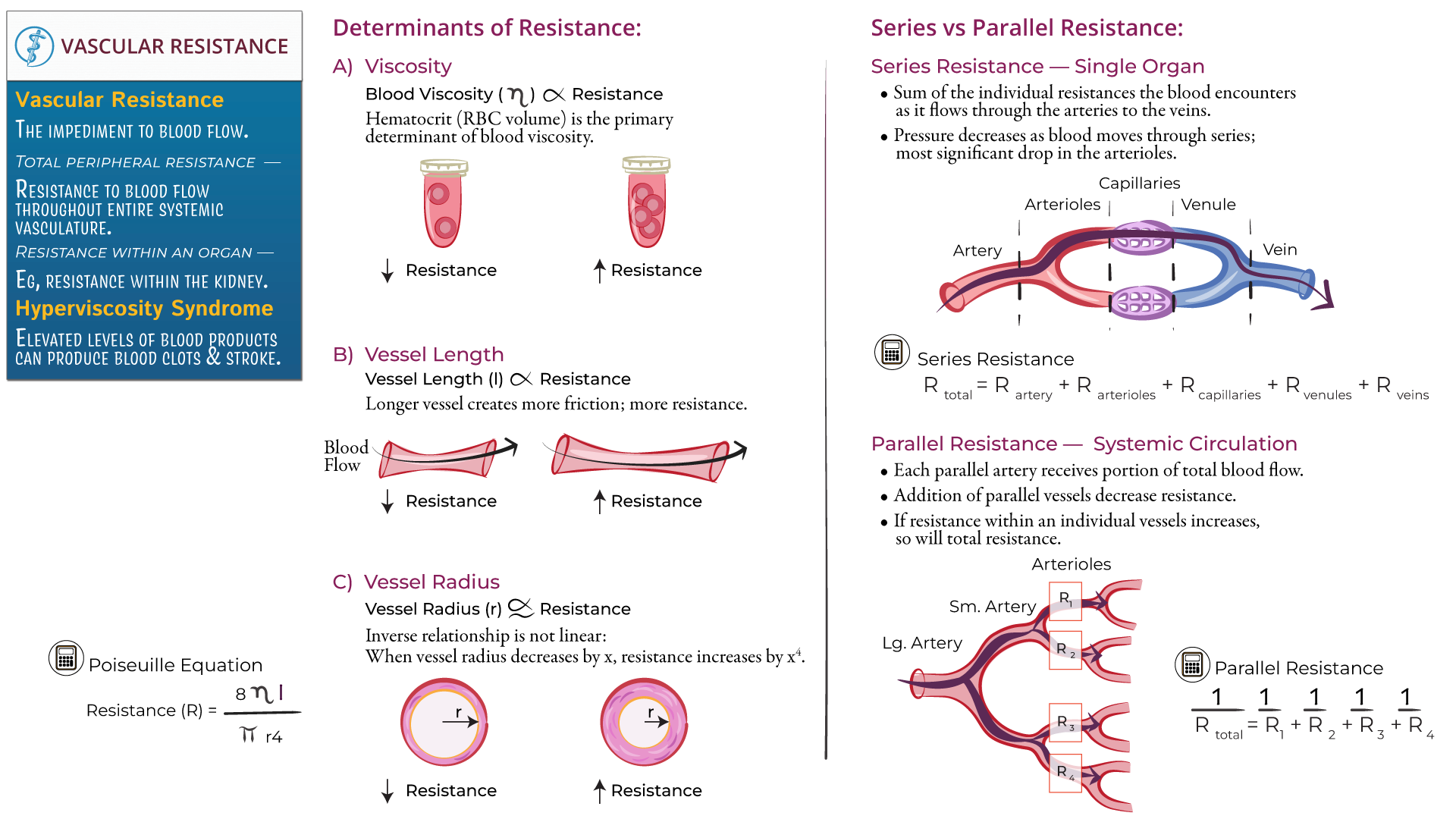
Blood Viscosity: A Thickening Threat
Blood viscosity, or the thickness of the blood, directly impacts peripheral resistance. Higher viscosity, often due to increased red blood cell count or elevated plasma proteins, translates to greater resistance.
Conditions like polycythemia vera, a disorder causing excessive red blood cell production, increase blood viscosity and subsequently elevate peripheral resistance. Dehydration can also contribute to increased viscosity.
Therapeutic interventions may include phlebotomy to reduce red blood cell mass in cases of polycythemia or intravenous fluids to combat dehydration and lower viscosity.
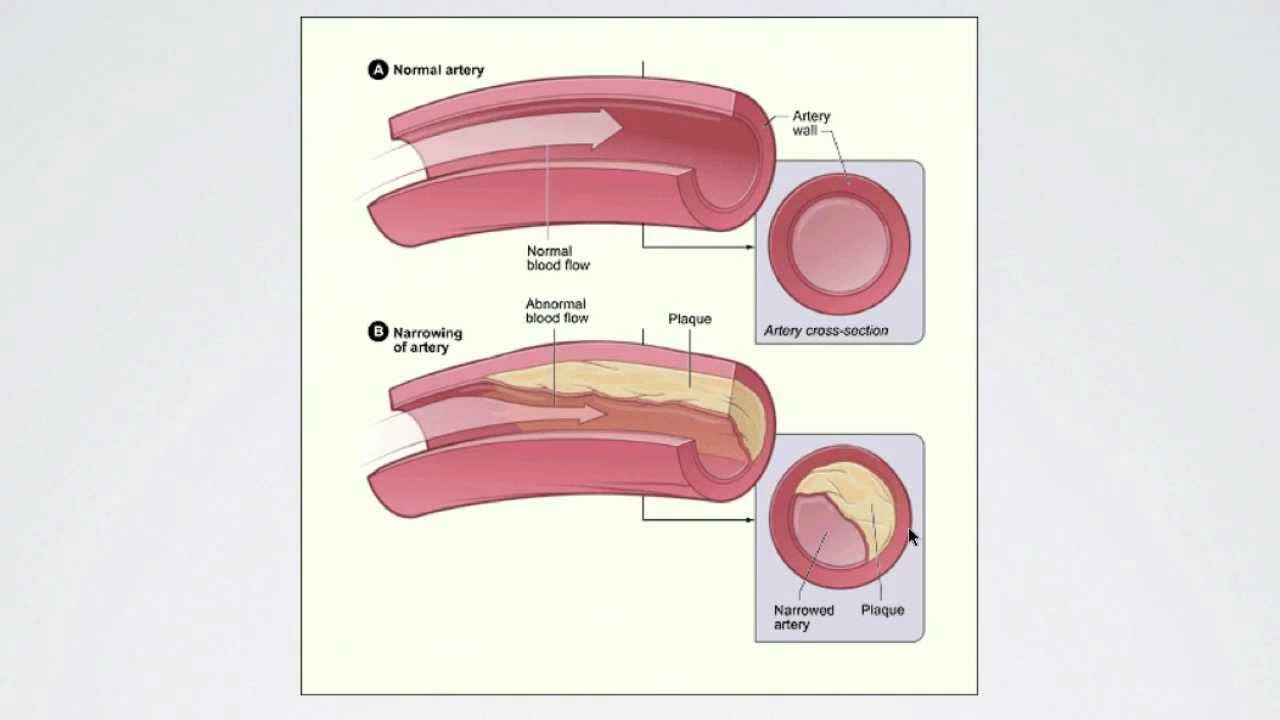
Blood Vessel Diameter: Constriction vs. Dilation
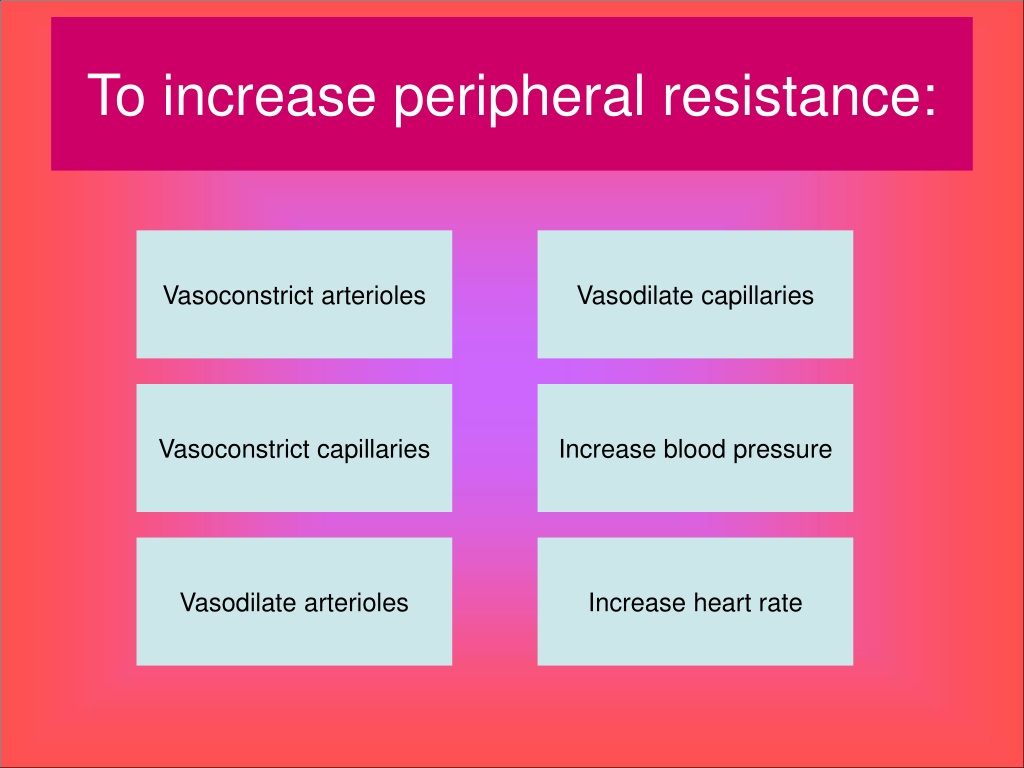
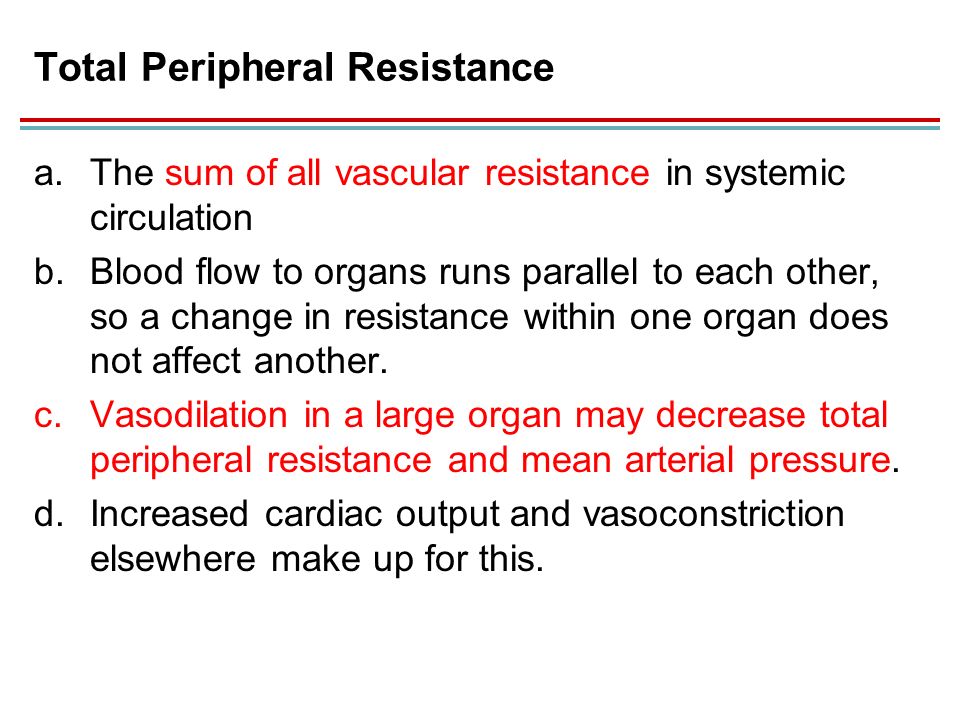
The diameter of blood vessels, primarily arterioles, is a critical determinant of peripheral resistance. Vasoconstriction, the narrowing of blood vessels, increases resistance, while vasodilation decreases it.
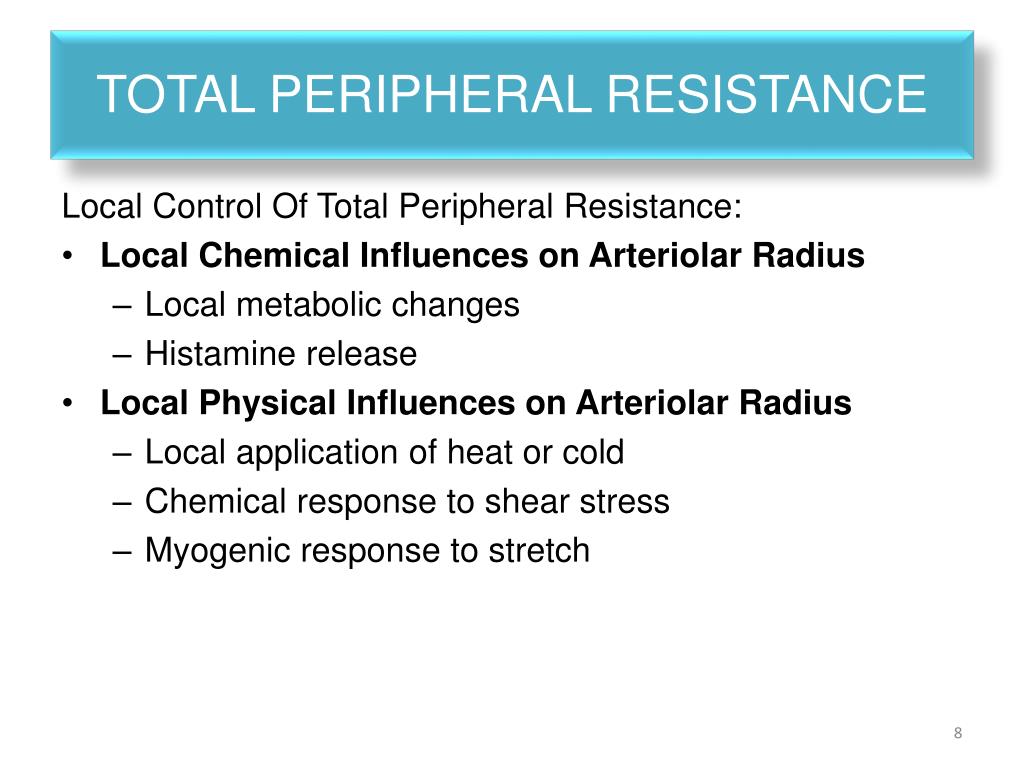
The autonomic nervous system plays a key role, with sympathetic nerve stimulation generally leading to vasoconstriction. Conversely, parasympathetic stimulation often promotes vasodilation.
Angiotensin II, a potent vasoconstrictor, acts on blood vessel smooth muscle to narrow the vessel lumen. Medications like ACE inhibitors and ARBs target this system to reduce vasoconstriction and lower blood pressure.
Autonomic Nervous System Activity: The Body's Control Center
The autonomic nervous system (ANS) exerts significant influence over peripheral resistance. Its sympathetic and parasympathetic branches have opposing effects on blood vessel tone.
Increased sympathetic activity, often triggered by stress or the "fight or flight" response, leads to vasoconstriction and increased peripheral resistance. This response is mediated by norepinephrine acting on alpha-adrenergic receptors in blood vessels.
Conversely, increased parasympathetic activity promotes vasodilation and decreased peripheral resistance. Beta-blockers are medications that can block sympathetic stimulation and lower peripheral resistance.
Hormonal Influences: Chemical Messengers at Work
Various hormones significantly impact peripheral resistance. Besides Angiotensin II, other hormones like epinephrine and vasopressin also play vital roles.
Epinephrine, released during stress, can cause vasoconstriction in some vascular beds and vasodilation in others, depending on the receptor type present. Vasopressin, also known as antidiuretic hormone (ADH), is a powerful vasoconstrictor that increases peripheral resistance.
Hormonal imbalances, such as those seen in conditions like hyperthyroidism, can disrupt normal vascular function and alter peripheral resistance.
Blood Volume: The Circulating Load
Blood volume indirectly affects peripheral resistance. While not a direct determinant, significant changes in blood volume can influence blood pressure and, consequently, vascular tone.
Hypovolemia, or low blood volume, can trigger compensatory mechanisms that increase peripheral resistance to maintain blood pressure. Hypervolemia, or high blood volume, may lead to increased blood pressure and eventually impact vascular tone.
Conditions like heart failure or kidney disease can lead to fluid retention and hypervolemia, potentially contributing to increased peripheral resistance in the long term.
The Role of Nitric Oxide: A Key Vasodilator
Nitric oxide (NO) is a powerful vasodilator produced by endothelial cells lining blood vessels. It plays a crucial role in regulating vascular tone and maintaining low peripheral resistance.
NO promotes smooth muscle relaxation, leading to vasodilation and improved blood flow. Endothelial dysfunction, often associated with conditions like hypertension and diabetes, can impair NO production and increase peripheral resistance.
Therapies aimed at improving endothelial function and increasing NO bioavailability are crucial in managing cardiovascular risk.
Age and Genetics: Unavoidable Factors
Age and genetics can predispose individuals to higher peripheral resistance. Vascular stiffness tends to increase with age, leading to higher resistance.
Genetic factors can influence vascular function and susceptibility to conditions that increase peripheral resistance. Family history of hypertension or cardiovascular disease is a significant risk factor.
While these factors are largely unavoidable, lifestyle modifications and targeted therapies can mitigate their impact.
Moving Forward: Research and Clinical Implications
Ongoing research continues to shed light on the complex interplay of factors influencing peripheral resistance. Clinical trials are exploring novel therapies that target specific pathways involved in vascular regulation.
Effective management of peripheral resistance requires a holistic approach, including lifestyle modifications, pharmacological interventions, and addressing underlying medical conditions.
Continued monitoring and personalized treatment strategies are essential to optimize cardiovascular health and reduce the burden of hypertension and related diseases.





.jpg)
+resistance.jpg)


