Choose All That May Cause Hemolytic Anemia.

A surge in hemolytic anemia cases is triggering widespread concern among hematologists. Authorities are scrambling to identify the root causes behind the alarming spike in diagnoses.
This article aims to provide a succinct overview of potential triggers for hemolytic anemia, highlighting key factors that healthcare professionals and the public should be aware of, based on current medical understanding and recent case analyses.
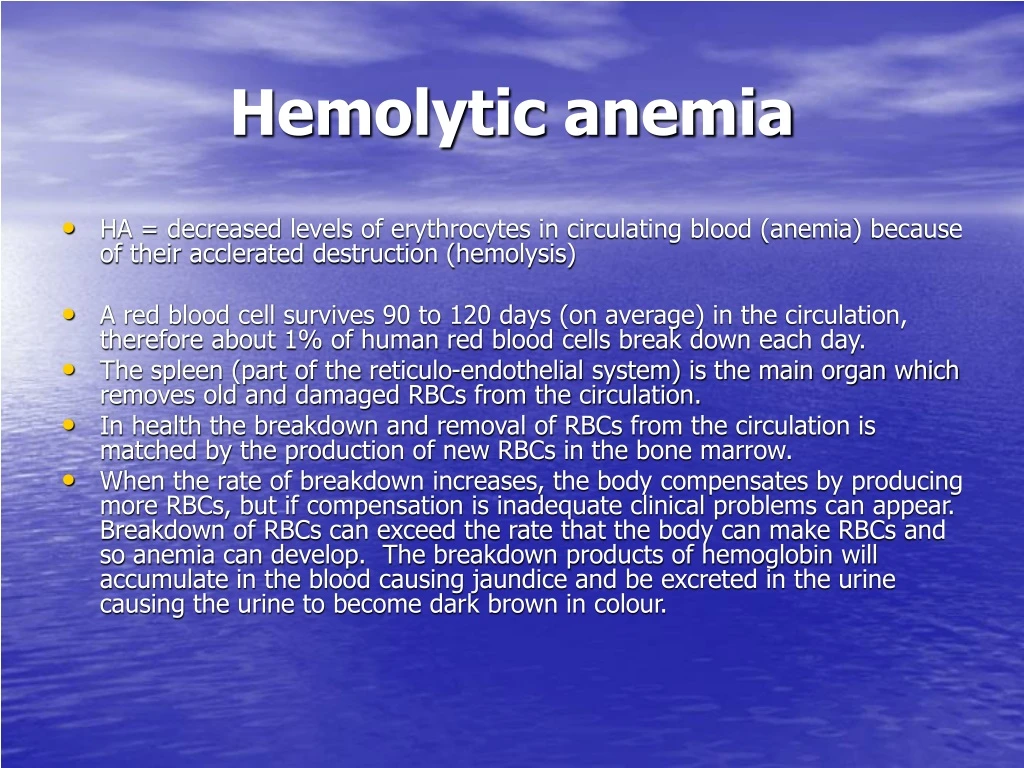
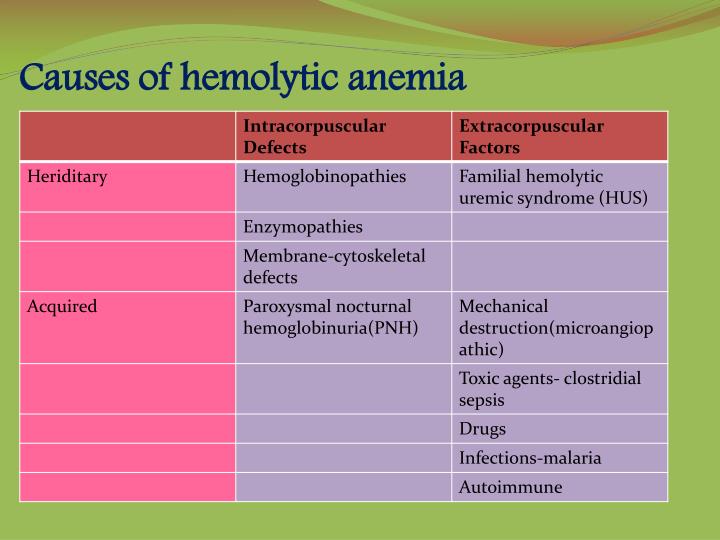
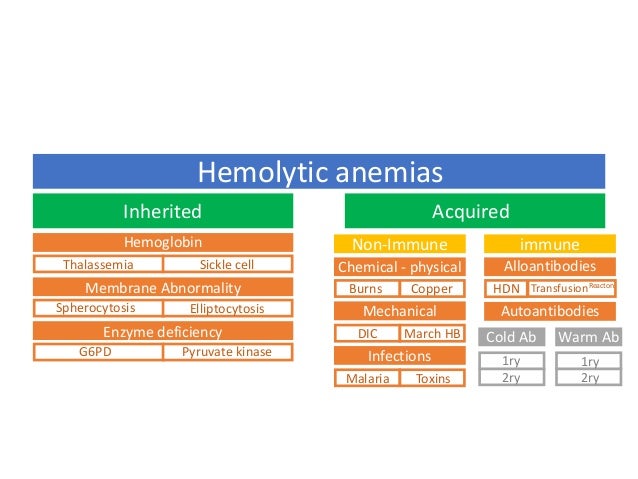
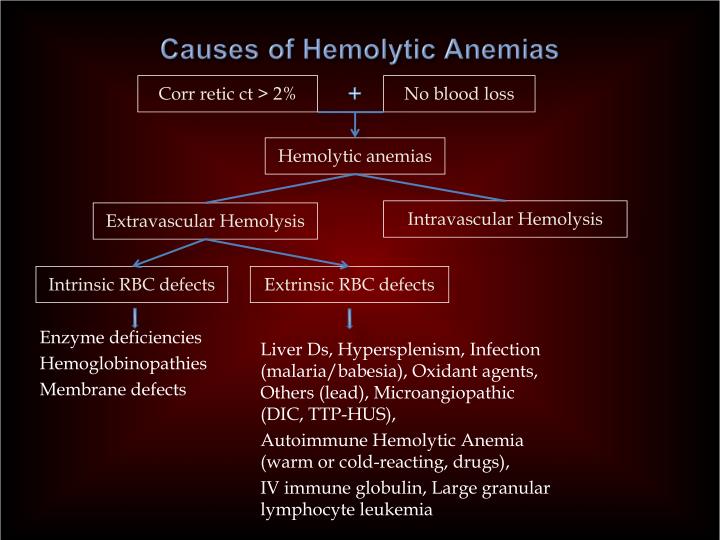
Genetic Predisposition
Hereditary conditions play a significant role in predisposing individuals to hemolytic anemia. Sickle cell anemia, a well-known genetic disorder, causes red blood cells to become rigid and sickle-shaped, leading to premature destruction.
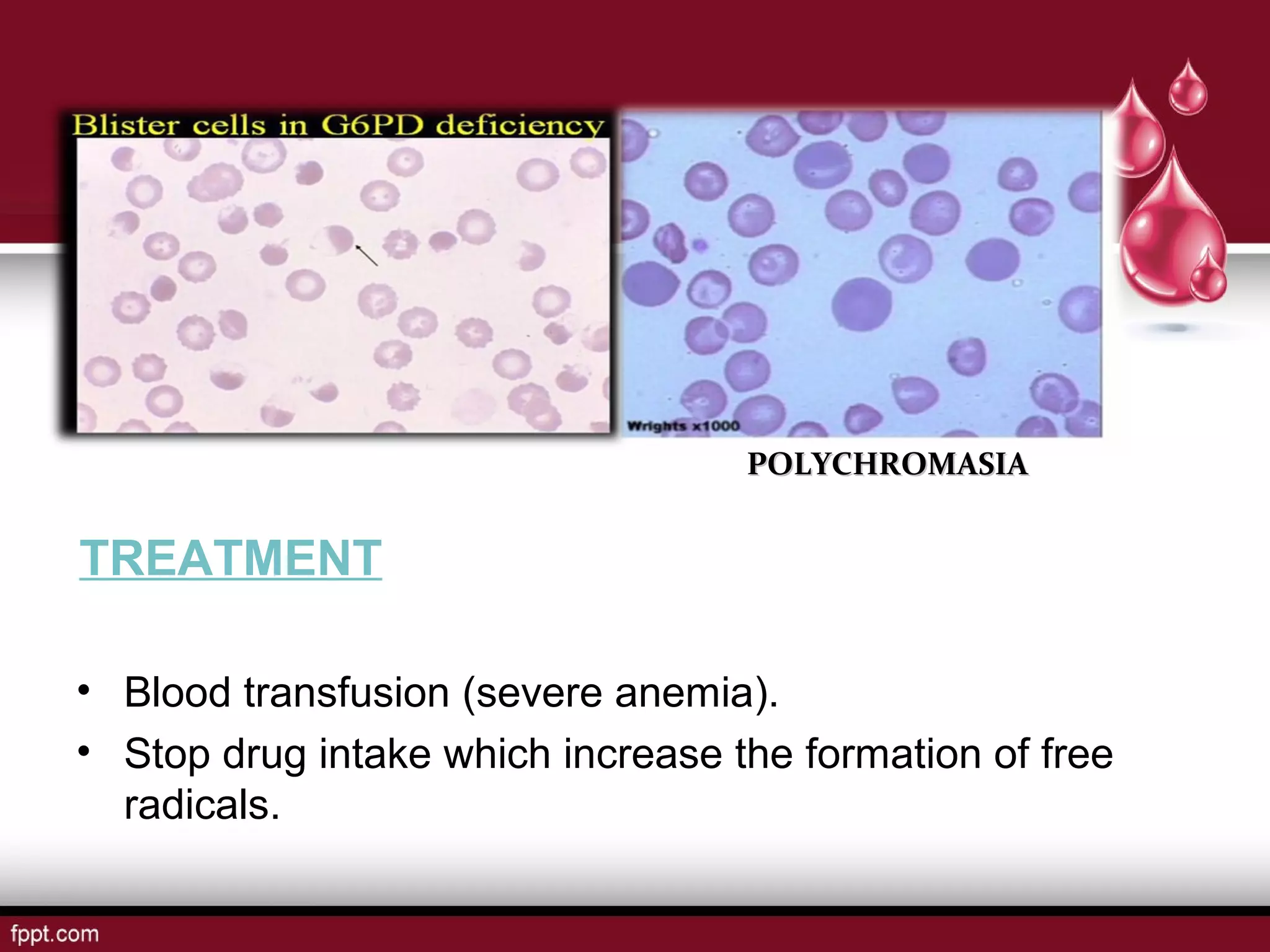
Thalassemia, another inherited blood disorder, affects the production of hemoglobin, resulting in fragile red blood cells susceptible to hemolysis. Certain enzyme deficiencies, such as G6PD deficiency, render red blood cells vulnerable to oxidative stress and subsequent breakdown.
These genetic factors often manifest early in life, requiring careful monitoring and management.
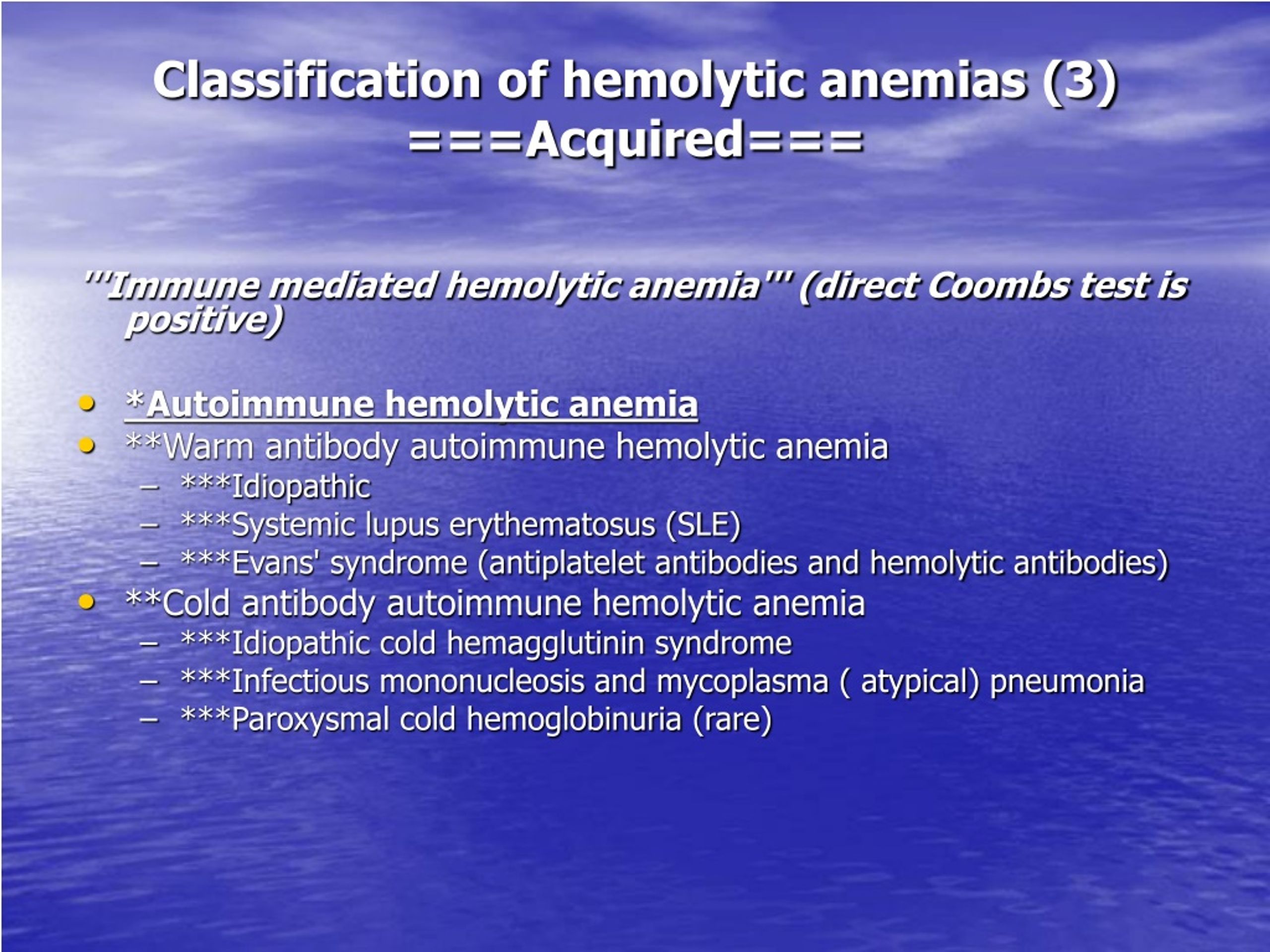
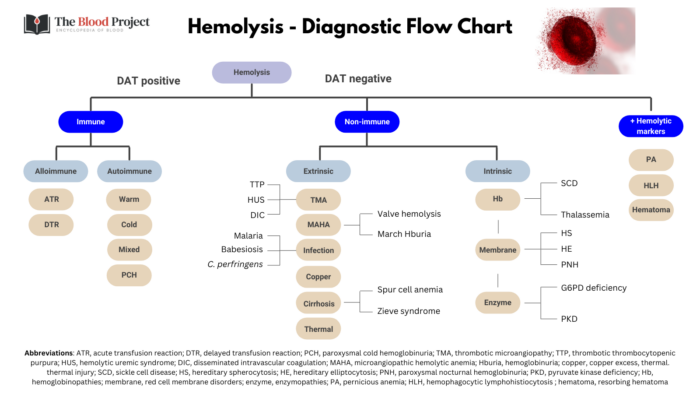
Autoimmune Disorders
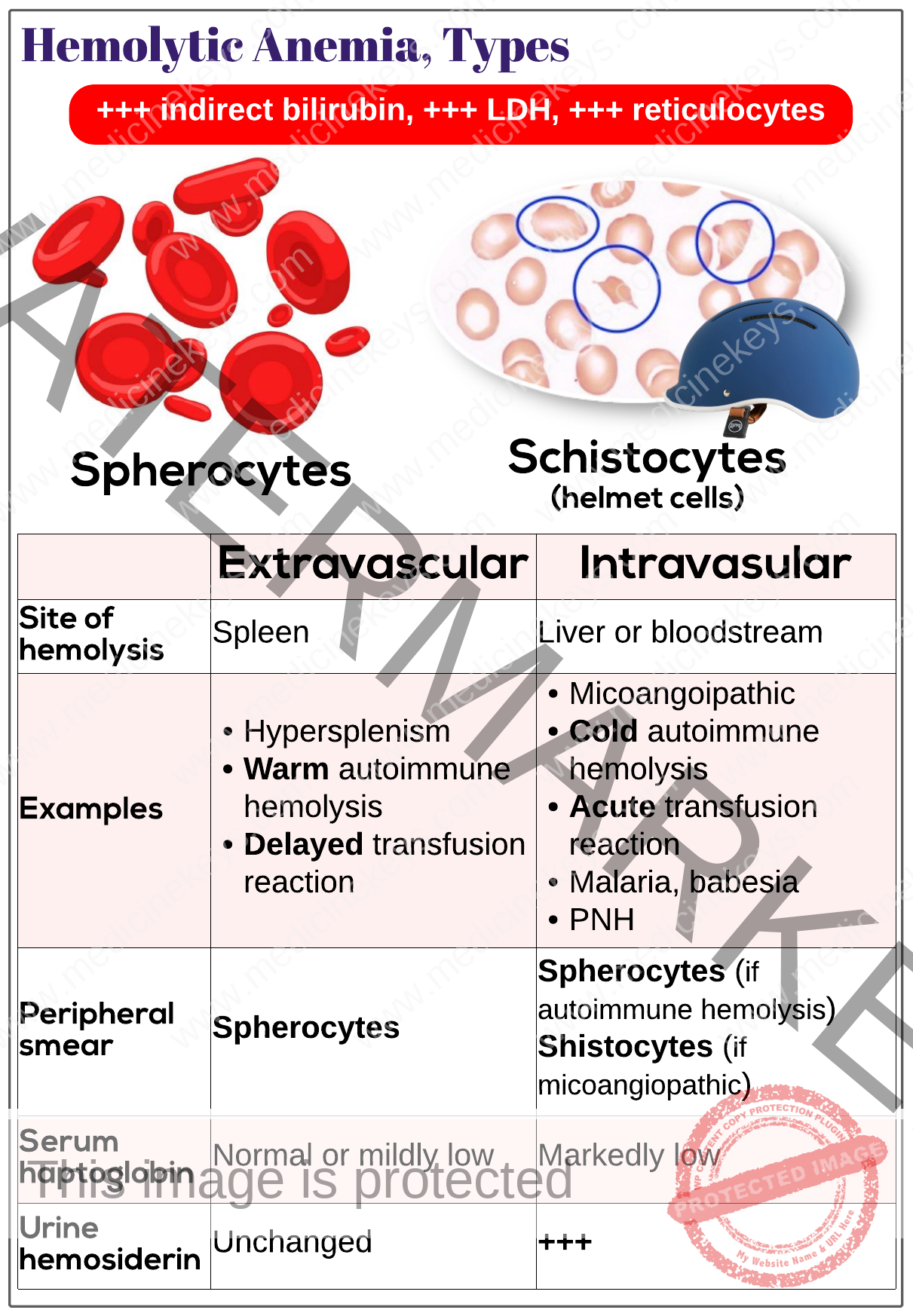
The body's own immune system can mistakenly attack red blood cells, leading to autoimmune hemolytic anemia (AIHA). Warm AIHA, triggered by antibodies that react at body temperature, is often associated with underlying conditions like lupus or lymphoma.
Cold AIHA, caused by antibodies active at lower temperatures, can occur after infections like mycoplasma pneumonia. Identifying and treating the underlying autoimmune disorder is crucial for managing AIHA effectively.
Prompt diagnosis is key to preventing severe complications arising from uncontrolled autoimmune responses.
Infections
Certain infections can directly or indirectly trigger hemolytic anemia. Malaria parasites invade red blood cells, causing their rupture and subsequent hemolysis.
Babesiosis, another parasitic infection transmitted by ticks, also leads to red blood cell destruction. Some bacterial infections, such as those caused by Clostridium perfringens, release toxins that damage red blood cells.
Preventative measures and prompt treatment of these infections are crucial in mitigating the risk of associated hemolytic anemia.
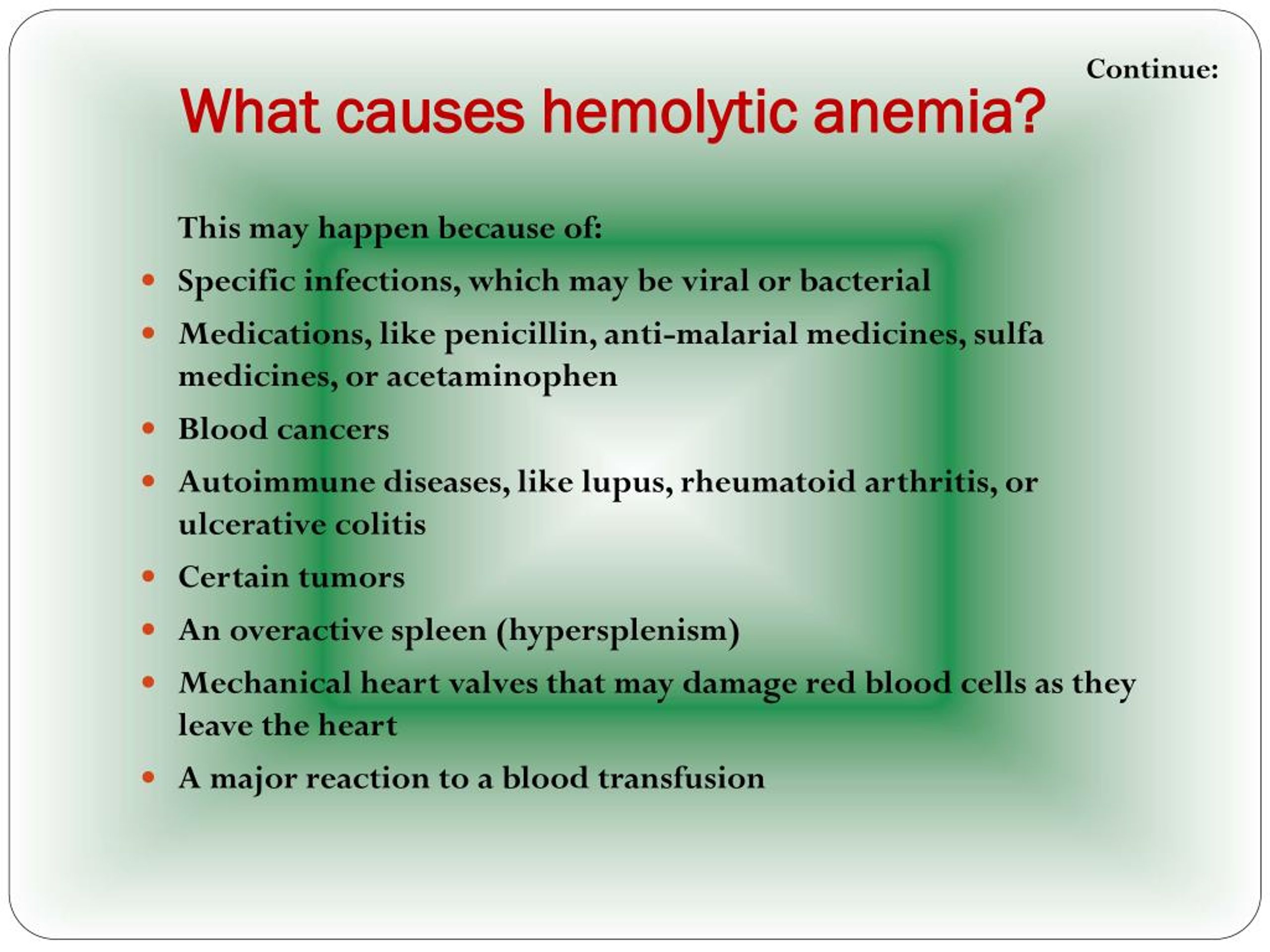
Medications and Toxins
Exposure to certain medications and toxins can induce hemolytic anemia in susceptible individuals. Drug-induced hemolytic anemia can occur due to various mechanisms, including immune-mediated reactions and direct red blood cell damage.
Drugs like penicillin and cephalosporins have been implicated in immune-mediated hemolysis. Exposure to toxins like lead and arsenic can also damage red blood cells, leading to hemolytic anemia.
Careful monitoring of patients on potentially hemolytic medications and avoidance of toxic exposures are essential preventative steps.
Mechanical Trauma
Physical trauma to red blood cells can cause mechanical hemolytic anemia. Microangiopathic hemolytic anemia (MAHA) occurs when red blood cells are damaged as they pass through narrowed or damaged blood vessels.
Conditions like thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS) are characterized by MAHA. Artificial heart valves can also cause mechanical damage to red blood cells, leading to hemolysis.
Addressing the underlying condition causing vascular damage or optimizing prosthetic valve function is crucial for managing mechanical hemolytic anemia.
Other Potential Causes
Other less common causes of hemolytic anemia include paroxysmal nocturnal hemoglobinuria (PNH), a rare acquired genetic disorder that affects red blood cells. Severe burns can also lead to red blood cell destruction.
Hypophosphatemia, a deficiency of phosphate in the blood, can impair red blood cell metabolism and lead to hemolysis. High altitude, particularly in those with certain predispositions, can exacerbate red cell breakdown.
These diverse factors underscore the complexity of hemolytic anemia diagnosis and management.
Moving Forward
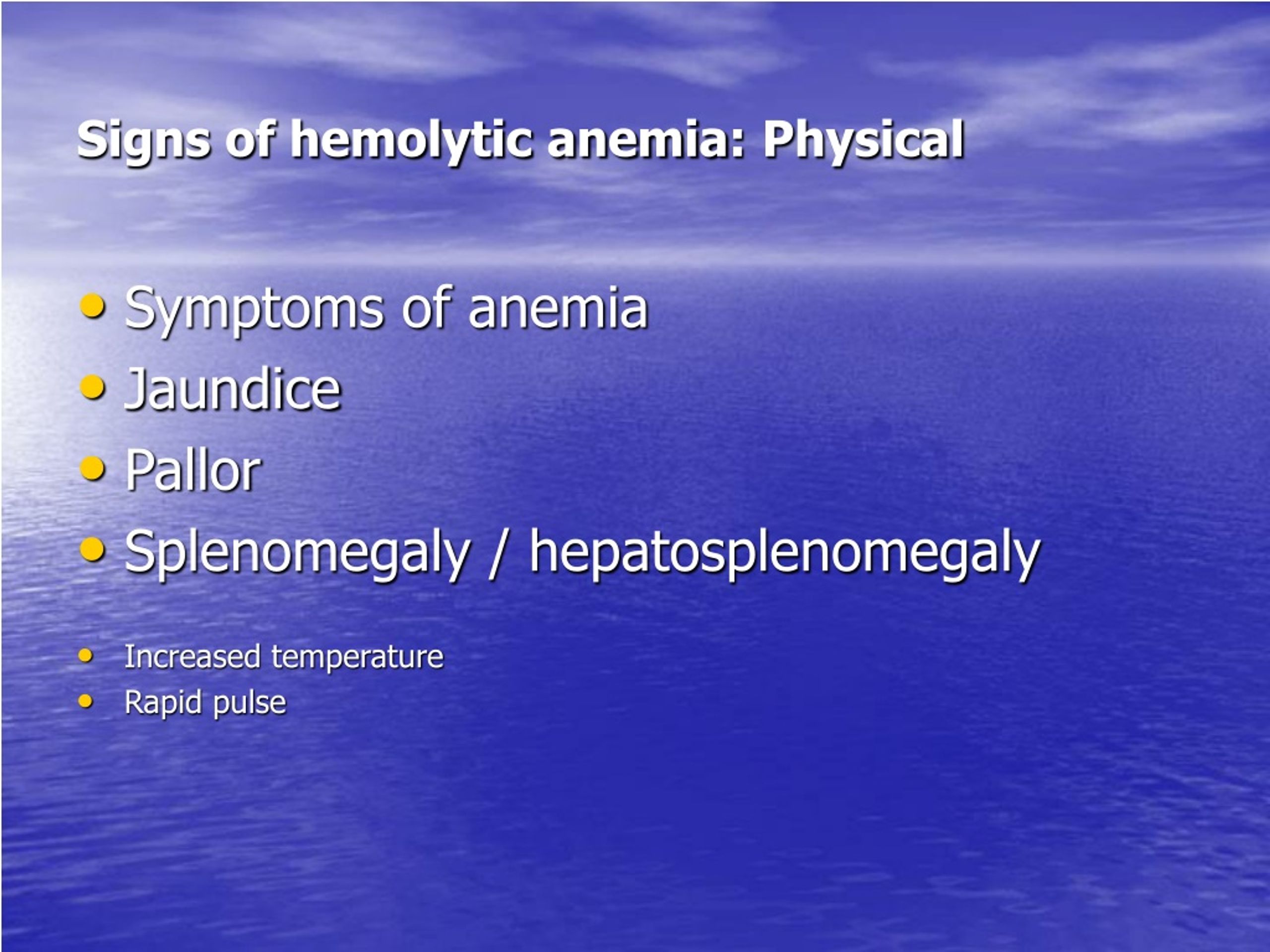
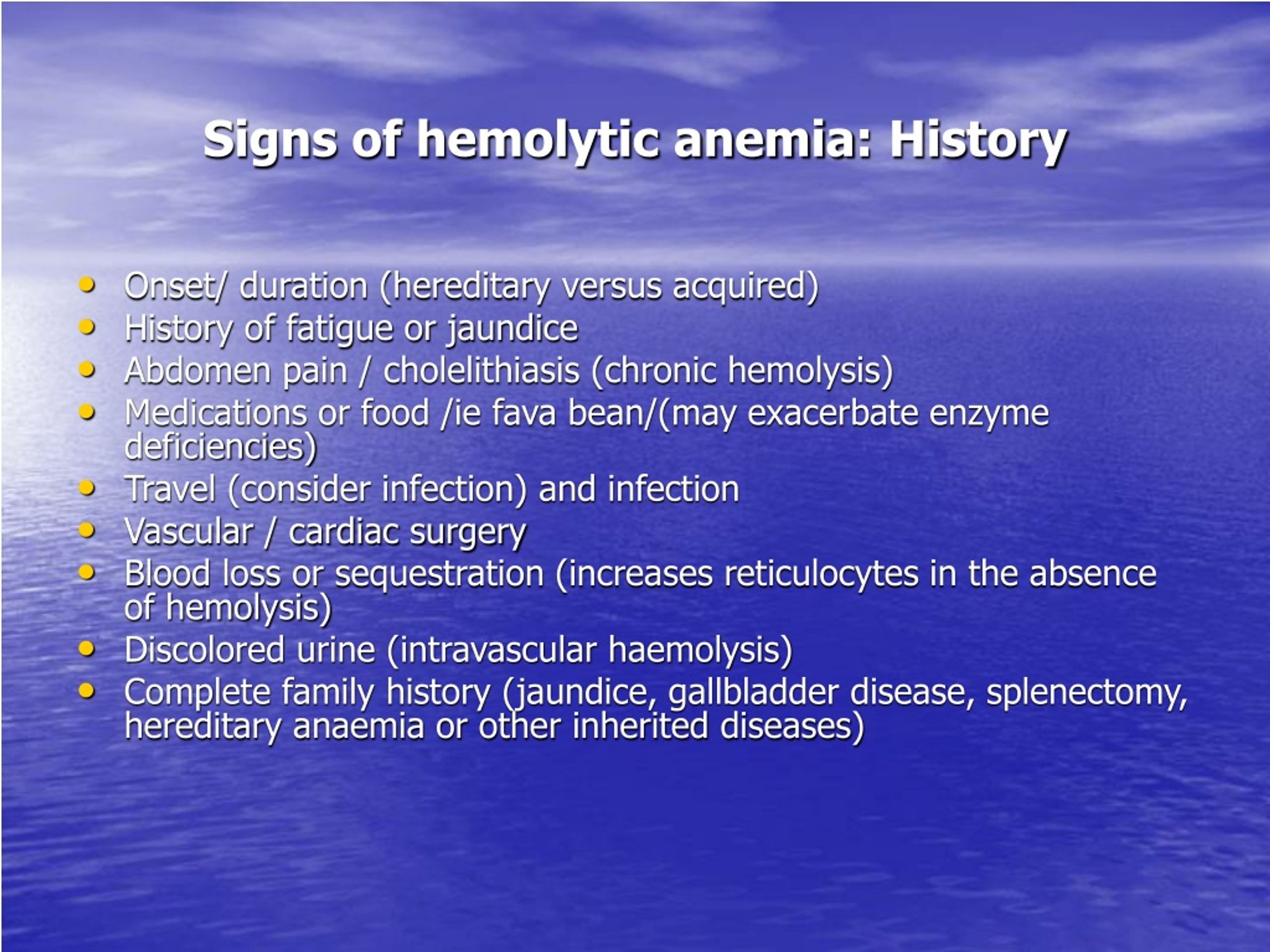
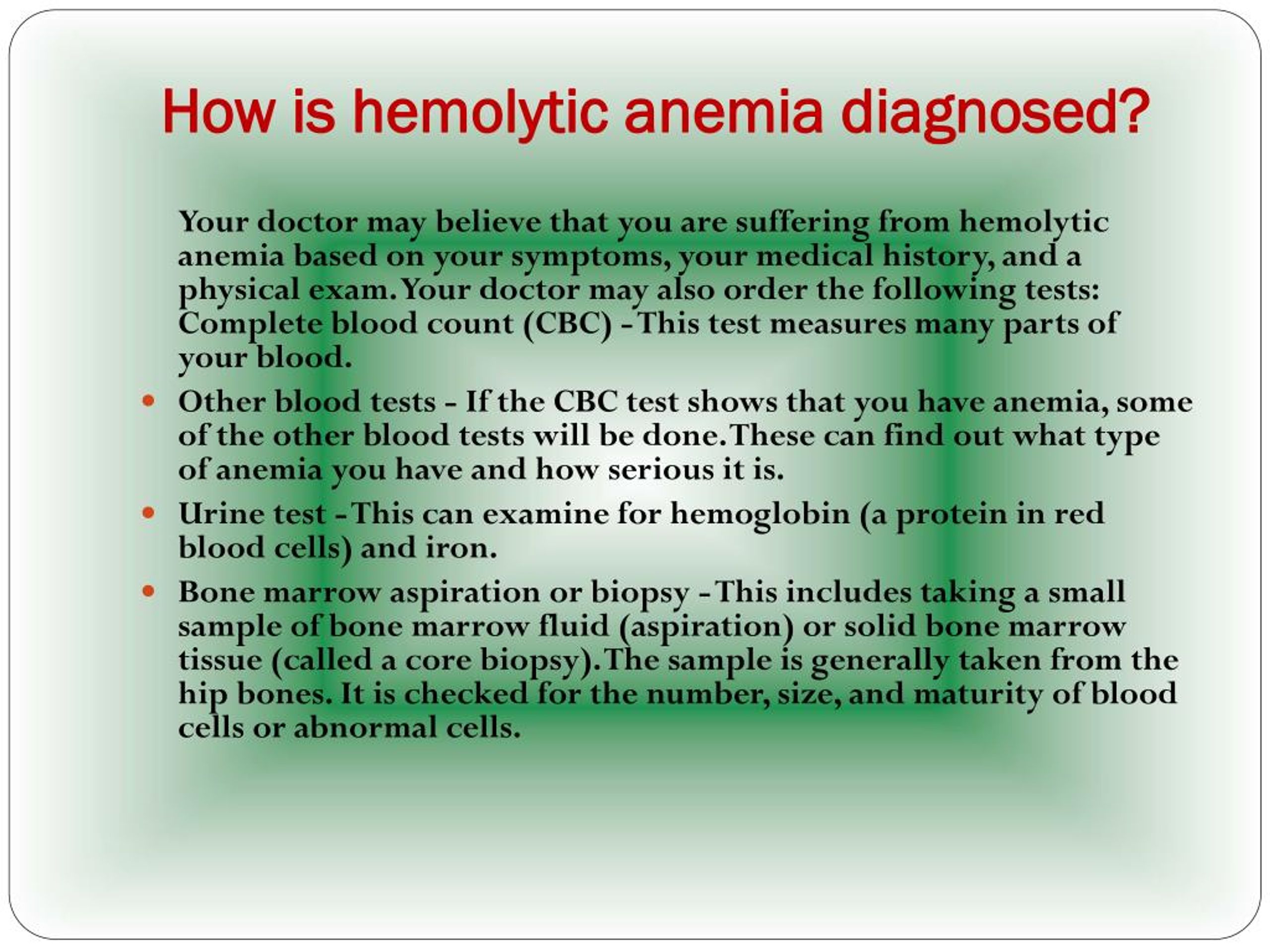
The investigation into the rising hemolytic anemia cases is ongoing. Healthcare providers are urged to maintain vigilance and promptly evaluate patients presenting with symptoms suggestive of hemolytic anemia, such as fatigue, jaundice, and dark urine.
Further research is needed to fully understand the interplay of genetic, environmental, and infectious factors contributing to the recent surge. Public health initiatives aimed at raising awareness and promoting preventative measures are crucial in mitigating the impact of hemolytic anemia.
Continued monitoring and data analysis will be essential in guiding effective interventions and improving patient outcomes.